Abstract
To evaluate image quality in the assessment of the coronary arteries during routine ECG-gated multidetector CT (MDCT) of the chest. One hundred and thirty three patients in sinus rhythm underwent an ECG-gated CT angiographic examination of the entire chest without β-blockers with a 64-slice CT system. In 127 patients (95%), it was possible to assess the coronary arteries partially or totally; coronary artery imaging failed in six patients (5%), leading to a detailed description of the coronary arteries in 127 patients. Considering ten coronary artery segments per patient, 75% of coronary segments were assessable (948/1270 segments). When the distal segments were excluded from the analysis (i.e., seven coronary segments evaluated per patient), the percentage of assessable segments was 86% (768/889 proximal and mid coronary segments) and reached 93% (474/508) when assessing proximal segments exclusively. The mean number of assessable segments was significantly higher in patients with a heart rate ≤80 bpm (n=95) than in patients with a heart rate >80 bpm (n=38) (p<0.002). Proximal and mid-coronary segments can be adequately assessed during a whole-chest ECG-gated CT angiographic examination without administration of β-blockers in patients with a heart rate below 80 bpm.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Until recently, the non-invasive evaluation of coronary arteries has remained in the domain of cardiac imaging, requiring dedicated scanning protocols of the heart volume. Over time, these protocols and the potential imaging capabilities of coronary CT angiography have evolved in step with advances in CT technology. Four-slice multidetector CT (MDCT) scanners showed promising results, but were not robust enough to consistently produce reliable coronary imaging because of insufficient spatial and temporal resolution [1–4]. The introduction of 16-slice MDCT technology combined with β-blocking improved the image quality and diagnostic accuracy of MDCT to detect significant disease in coronary segments equal to or larger than 2 mm in diameter [5–9]. The recent introduction of 64-slice MDCT scanners offers new perspectives, as it is now possible to obtain retrospective ECG-gated MDCT examinations of the entire thorax within reasonable breath-hold durations. As a result, CT imaging of the thorax has the potential to widen its fields of clinical applications.
No longer restricted to a morphological assessment of respiratory diseases, CT imaging of the thorax can also provide cardiac functional information, of clinical value to the management of patients with a wide variety of acute or chronic respiratory disorders [10]. Because this CT technology offers the possibility of generating high-resolution and motion-free images of the coronary arteries, evaluation of the coronary arteries during CT examinations of the chest should further widen the clinical applications of CT for respiratory patients, keeping in mind that cigarette smoking is a shared risk factor for both impaired lung function and cardiovascular events [11]. The purpose of the present study was thus to investigate coronary imaging quality during routine ECG-gated multidetector CT (MDCT) of the chest with a 64-slice CT system.
Materials and methods
Population
During a 6-month period (October 2004-March 2005), a prospective study included 133 consecutive patients (89 males; 44 females) (mean ± SD age: 55.5±5.43 yr; range: 18–99), in sinus rhythm, referred for a CT angiographic examination of the chest. As ECG-gated CT examination of the entire thorax with 64-slice CT offers the possibility of providing additional information regarding cardiac function, the decision to obtain an ECG-gated CT angiographic study of the entire thorax was approved by our Institutional Review Board and Ethics Committee in the clinical context of known or suspected right ventricular dysfunction; informed consent from patients was not required. In the studied population, CT was indicated for the management of bronchopulmonary (n=102) or pulmonary vascular (n=31) diseases. Detailed description of the studied population and scanning parameters have been reported in a separate study [12]. In the same group of patients who did not receive β-blockers prior to CT scanning, the objective of the present study was to investigate the assessability of coronary arteries acquired by a routine ECG-gated MDCT examination of the chest.
CT examination
Acquisition parameters
CT examinations were performed with a 64-slice MDCT scanner (Sensation 64, Siemens, Forchheim, Germany). The CT protocol consisted of an ECG-gated acquisition over the entire thorax (namely, from lung apex to diaphragm), obtained in the cranio-caudal direction, with the patients scanned in the supine position and after deep inspiration. The acquisition parameters were as follows: (a) collimation: 32×0.6 mm with z-flying focal spot for the simultaneous acquisition of 64 overlapping 0.6-mm slices; rotation time: 0.33 sec; pitch: 0.3; 120 kV; 200 mAs, and (b) this examination was systematically obtained with automatic adjustment of the milliamperage according to the patient’s size (Care Dose 4D; Siemens Medical Solutions, Germany) and also monitored by the ECG tracing (ECG Pulsing, Siemens Medical Solutions, Germany). For ECG-controlled tube current modulation, the tube output is raised to the nominal level within every cardiac cycle for a limited interval in the diastolic phase where data are to be reconstructed for morphological purposes. During the remaining part of the cardiac cycle, the tube output can be reduced by approximately 80% by a corresponding decrease in the tube current. Designed for coronary CT angiography, this technique has been shown to achieve an overall exposure saving in radiation exposure of 30–50% without compromising image quality [13]. In this study, a tube current time product of 200 mAs was used because an acceptable image quality seemed to be achievable with the above-mentioned protocol in the initial patients.
Injection protocol
The injection protocol consisted of the administration of 120 ml of a contrast material with 350 mg of iodine per milliliter (iohexol; Omnipaque 350; Amersham Health, Carrigtohill, Ireland), administered at the flow rate of 4 ml/s. The automatic bolus-triggering software programme available on this CT unit (Care Bolus) was systematically applied with a circular region of interest positioned at the level of the ascending aorta, and the threshold for triggering data acquisition was preset at 120 HU.
Image reconstruction
For the purpose of assessing the coronary arteries, cross-sectional images were reconstructed from the aortic arch to the heart apex with a slice thickness of 1 mm in 0.6-mm intervals, a small field-of-view, using a soft reconstruction kernel (B20) to generate curved MPRs and MIP images of the coronary arteries. Four different sets of reconstructions at 30%, 40%, 60% and 70% of the R-R interval were systematically performed and analyzed to determine the optimal reconstruction window for each coronary artery. Adjacent positions were used if no satisfactory results were achieved with these initial window positions. To improve the temporal resolution and thus avoid motion artefacts, the multisegmented image reconstruction algorithm (utilizing raw data from up to two cardiac cycles) was systematically used for patients with a heart rate above 65 bpm (Adaptive Cardio-Volume algorithm, release VA 70; Siemens Medical Solutions). The images of selected reconstruction windows were transferred to an off-line computer workstation (Leonardo workstation; Siemens Medical Solutions) for postprocessing in a standardized fashion using a work-in-progress software for coronary artery imaging (Circulation, Siemens Medical Solutions).
CT parameters evaluated
The CT imaging protocol was supervised by two readers (DD; RS) with 2 years and 1 year of experience respectively in cardiac CT at the time of initiation of this study. They determined by consensus the optimal temporal reconstruction window for each coronary artery which was systematically recorded. Coronary arteries were then reviewed in consensus by the two radiologists on transverse images and curved MPRs and MIPs to assess image quality. For image analysis, coronary segments as defined by the American Heart Association were used, dividing the coronary tree into 15 segments [14]. In the present investigation, side branches (segments 9, 10, 12 and 14) of the left coronary artery and the distal segment of the right coronary artery (segment 4) were not included in the analysis, because of their small size and variability of its origin respectively, leading to the evaluation of ten segments per patient. By visual estimation, the readers had to determine the number of segments that could be assessed, analyzing segments 1–3 (right coronary artery, RCA), 5 (left main, LM), 6–8 (left anterior descending, LAD) and 11 and 13 (left circumflex, LCX). A coronary artery segment was considered to be of diagnostic image quality if it was visualized over its whole length and if the vessel lumen was completely depicted [15–17]. The presence of heavy calcifications within a given segment (and the resulting blooming artefacts known to interfere with the analysis of vessel lumen patency) did not lead to the scoring of this vessel as not assessable in terms of image quality, provided that the vessel was not degraded by cardiac motion artefacts and correctly opacified. The readers measured the level of enhancement within the coronary arteries, calculated after positioning a ROI (0.10 cm2) within the lumen of the proximal portion of each main coronary artery. The duration of postprocessing was systematically noted.
Statistical analysis
Statistical analysis was performed with commercially available software (SAS Institute, Cary, NC, USA). P values inferior to 0.05 were considered statistically significant. Results were expressed as means, standard deviations, and interquartile ranges for continuous variables, and as frequencies and percentages for categorical variables. Comparative analyses were obtained using the chi-square test for categorical data. For numerical variables, we used the unpaired Student t-test for groups greater than 30 in size, and the Mann-Whitney test otherwise.
Results
At the time of the MDCT examination, the mean heart rate of the studied population was 73 bpm (range: 42–120). The mean duration of data acquisition was 18.11±2.67 s (range: 10–27). In our study group, 127 patients (95%) had coronary arteries that could be partially or totally assessed; coronary artery imaging failed in six patients (5%), due to a poor level of enhancement achieved within coronary arteries in five patients (i.e., attenuation values below 200 HU) and alteration of image quality by interpolation artefacts in one patient with a heart rate of 45 bpm. The average time for post-processing varied between 15 and 20 minutes.
Vessel-by-vessel analysis
Among the 127 patients with assessable coronary arteries, a total of 1270 coronary artery segments (ten segments per patient) were systematically analyzed, including 508 proximal segments (four proximal segments per patient, i.e. segment 1 of the RCA, segment 5 or left main trunk, segment 6 of the LAD, and segment 11 of the circumflex artery) and 762 more distal segments (segments 2 and 3 of the RCA; segments 7 and 8 of the LAD, and segments 13 and 15 of the circumflex artery).
Among the 508 proximal segments analyzed, 474 segments (93%) were assessable and 34 segments (7%) were found non-assessable. The main reasons for impaired image quality of proximal segments were poorly opacified arterial lumen (n=20), cardiac motion (n=6) or both (n=8). The 474 assessable arteries included 125 LM, 118 LAD, 111 LCX and 120 RCA. The mean (± SD) attenuation value measured at the level of these 474 assessable proximal segments was 294.28 HU (±91.31). For individual coronary arteries, the mean attenuation value was 322.28 HU (±82.89) for the left main coronary artery, 326.38 HU (±90.34) for the left anterior descending artery, 312.00 HU (±92.68) for the circumflex artery and 303.05 HU (±79.24) for the right coronary artery. Table 1 summarizes the temporal windows for an optimal timing of image data reconstruction of the 474 assessable right and left coronary arteries. Motion-free delineation of 294 out of the 354 assessable left coronary arteries (83%) was obtained in the mid-to-end diastolic phase (60%–70% of the R-R interval). Among the 120 RCA rated as assessable, 49 arteries were reconstructed at 70% of the R-R interval and 27 arteries were reconstructed at 60% of the R-R interval, leading to a total of 76 RCA (63%) reconstructed during a mid-diastolic phase. The diameter of the 474 assessable proximal segments was greater than 3 mm for 311 segments, between 1.5 and 3 mm for 152 segments and below 1.5 mm for 11 segments (Table 2).
Considering ten coronary artery segments per patient (total: 1270 segments analyzed), 948 coronary segments were assessable (75%). When the distal segments (segment 3 of the RCA, segment 8 of the LAD and segment 15 of the CX) were excluded from the analysis (seven coronary segments evaluated per patient; total: 889 segments analyzed), the percentage of segments for which the image quality was acceptable rose from 75% (948/1270 segments) to 86% (768/889 segments) (p<0.0001). Table 3 summarizes the mean number of assessable segments per coronary artery. Figs. 1, 2, 3 and 4 illustrate the image quality achievable with the investigated protocol at the level of left (Figs. 1 and 2) and right (Figs. 3 and 4) coronary arteries. One hundred (94.5%) right coronary arteries were totally or partially assessable. The use of ECG-controlled tube current modulation was not found to influence the assessment of RCA. Table 4 summarizes the lesions detected at the level of the right and left coronary arteries in our study group, illustrated by Figs. 5 and 6.
Forty-one-year-old male (patient’s weight: 62 kg; patient’s height: 180 cm) with a heart rate of 60 beats per minute (bpm). Curved planar reformations of the left anterior descending artery (LAD) (Figure 1a) and left circumflex artery (LCX) (Figure 1b) with normal diameters. Note the good image quality achievable with a dose-length-product of 206 mGy.cm
Sixty-one-year-old female (patient’s weight: 65 kg; patient’s height: 163 cm) with a heart rate of 69 beats per minute (bpm). Curved planar reformation of the left anterior descending artery (LAD) with a normal diameter. Note the presence of minimal image noise which does not hamper coronary artery assessment (dose-length-product of the examination: 224 mGy.cm)
64 year-old male (patient’s weight: 86 kg; patient’s height: 174 cm) with a heart rate of 80 beats per minute (bpm). Curved planar reformations of the right coronary artery (RCA) (Figure 3a; Figure 3b) with a normal diameter. Note the good image quality achievable in this large patient (dose-length-product of the examination: 422 mGy.cm)
Thirty-eight-year-old male (patient’s weight: 79 kg; patient’s height: 181 cm) with a heart rate of 62 beats per minute (bpm). Curved planar reformation of the right coronary artery (RCA) with a normal diameter. Minimal artifacts from the right atrium that do not compromise diagnostic evaluation of the arterial lumen (dose-length-product of the examination: 267 mGy.cm)
Sixty-six-year-old male (patient’s weight: 65 kg; patient’s height: 172 cm) with a heart rate of 64 beats per minute (bpm). Curved planar reformation of the left anterior descending artery (LAD) showing thin calcified plaques at the proximal level (white arrows) and more distally (black arrows) (dose-length-product of the examination: 225 mGy.cm)
Seventy-two-year-old male (patient’s weight: 75 kg; patient’s height: 169 cm) with a heart rate of 58 beats per minute (bpm). Curved planar (Figure 6a) and planar (Figure 6b) reformations of the left anterior descending artery (LAD) illustrate a partly calcified lumen reduction (arrow) (dose-length-product of the examination: 236 mGy.cm)
Patient-per-patient analysis
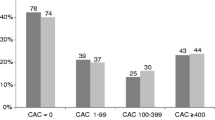
Table 5 summarizes the number of assessable segments per patient in the127 patients with a technically-successful CT angiogram of coronary arteries. A statistically significantly higher proportion of assessable segments was observed in patients with a heart rate ≤80 bpm (n=95) than in patients with a heart rate >80 bpm (n=38) whether evaluating ten segments per patient (p=0.001), seven segments per patient (p=0.0037) or four segments per patient (p=0.006). No statistically significant difference in the mean number of assessable segments was observed when comparing patients with a heart rate below 70 bpm and patients with a heart rate between 70 and 80 bpm for the three categories of segments analyzed per patient (i.e., ten, seven and four segments analyzed per patient; p>0.05).
For 67 patients (50%), the same temporal window was used for reconstruction of all coronary arteries. Fifty-six of the 67 patients (74%) had all coronary arteries reconstructed at 60% or 70% of the R-R interval (i.e., mid-diastolic phase) whereas the remaining 11 patients (26%) had all coronary arteries reconstructed at 30% or 40% of the R-R interval (i.e., end-systolic phase). The mean heart rate of the 56 patients with all coronary arteries reconstructed during a mid-diastolic phase was significantly lower (65.18±10.6 bpm; range: 43–94) than that observed for the 11 patients with all coronary arteries reconstructed during an end-systolic phase (89.08±13.9 bpm; range: 68–110) (Mann-Whitney test; p<0.0001).
4- Radiation dose
The characteristics of the studied population were as follows: (a) mean ( ±SD) weight: 70.86 (±14.54) kg; (b) mean (±SD) height: 170.16 (±7.68) cm ; (c) mean ( ±SD) body mass index (BMI): 25.63 (±4.42) (range: 14.86–40.23). The mean DLP value was 279.86 (±117.50) mGy.cm (range: 97–857). The estimated effective dose was 5.32±2.23 mSv (range: 1.84–16.28) for the overall population. Using a dedicated software package (WinDose, Institute of Medical Physics, Erlangen, Germany), the mean effective dose was 4.44±1.51 mSv (range: 2.16–11.06) for males and 5.01±2.84 mSv (range: 1.87–16.54) for females.
Discussion
To our knowledge, this is the first study demonstrating the possibility of assessing the coronary arteries during a whole-chest ECG-gated CT angiographic examination. Investigating a study group of 133 consecutive patients with a sinus rhythm, we observed that coronary artery imaging was achievable in 127 patients (95%) while it failed in six patients (5%). Among the 127 patients with a technically successful coronary CT angiogram, the mean attenuation value within proximal segments of coronary arteries was greater than 300 HU, a prerequisite for the evaluation of coronary arteries on CT angiograms [18]. In our study, the injection protocol was timed to coincide with peak enhancement of systemic arteries of the chest, incorporating not only bronchial and nonbronchial systemic arteries of the chest, but also coronary arteries, in addition to providing an excellent opacification of the pulmonary vessels. This compromise was achieved by a systematic use of bolus tracking with a circular region-of-interest positioned at the level of the ascending aorta with a threshold of 120 HU. In the absence of β receptor-blocking medication, motion-free delineation of coronary segments was possible for 93% of proximal segments (474/508), 86% of proximal and mid-segments (768/889) and 75% of all investigated coronary segments (948/1270). In the absence of similar studies with 64-slice CT scanners, these results can be compared with those obtained with dedicated coronary CT angiograms using 16-slice CT technology. In these studies, the percentages of analyzable segments ranged between 77.9% to 93.8%, depending on the size of the documented arteries and the number of coronary segments investigated per patient, which varied between eight and 15 segments [5, 8, 9, 16, 17, 19, 20]. Moreover, while none of our patients received specific medication, CT scanning was obtained in all but two of these studies [9, 16] with routine administration of an oral β-blocker. As previously reported [17, 21, 22], we noted that these results were dependent on the patient’s heart rate, with higher percentages of assessable segments at lower heart rates. However, the threshold for decreased image quality in our study is higher than that previously reported with 4- and 16-slice CT technology. With 4-detector-row CT scanners, 65 bpm was defined as the upper heart-rate threshold below which it was possible to achieve motion-free image quality [15, 23]. With 16-slice CT scanners, β-blockers were found to be useful above 70 bpm [17]. In the current study acquiring data sets with a temporal resolution of 165 ms, we found that the threshold of 80 bpm could be safely applied for coronary CT angiography in routine clinical practice. These results are in agreement with recently reported experiences with 64-slice CT scanners [24–26].
According to our initial results, good image quality can be achieved with reconstruction of a limited number of cardiac phases. On a vessel-by-vessel analysis, we found that motion-free delineation of 83% of left coronary arteries and 63% of right coronary arteries was achievable in the mid-diastolic phase (i.e., 60%–70% of the R-R interval), in agreement with previous reports based on data acquired with 16-slice CT scanners [9, 20, 24–27]. From the patient-by-patient analysis, we observed that a single temporal reconstruction window can be a priori preselected according to the patient’s heart rate. In agreement with Hoffman [9] and Bley [27], we found that good image quality was achievable at low heart rates (i.e., below 70 bpm) by using a mid-diastolic phase frame, shifting to end-systolic frames as the heart rate increases. Reconstruction of a limited number of cardiac phases represents an obvious improvement compared to reconstruction of multiple phases, as recommended elsewhere [28]. Although reconstruction time has tremendously reduced, the amount of data generated by multiphase reconstructions is difficult to manage, both for the radiologist and for the computerized network server or storage hardware, as previously emphasized in the literature [9]. One major limitation of the application of multidetector CT in the diagnosis of coronary artery disease is radiation exposure. In the present study consisting of ECG-gated acquisitions over the entire thorax, the mean DLP value was 280 mGy.cm which is far below the European reference value of 650 mGy.cm for a standard chest CT scan [29]. The estimated average effective dose of 5 mSv of our protocol is comparable to that reported for cardiac examinations obtained with ECG-controlled dose modulation [6, 30], confirming the clinical impact of recently developed scanner softwares for dose-saving during ECG-gated acquisitions. However, we should emphasise that our protocol enabled not only an evaluation of the coronary arteries but also provided morphologic information of thoracic organs as well as cardiac functional information. In a recent study, Salem et al. reported their experience with retrospective ECG-gated 64-slice MDCT angiography of the chest. Investigating 133 patients with a regular sinus rhythm who did not receive β-blockers, they found that both morphological and functional information could be obtained from the same data set in 92% of the population studied [12].
This study suffers from several limitations. Firstly, we evaluated image quality for coronary artery imaging, but did not compare CT images with conventional coronary angiograms. Consequently, it was not possible to evaluate the diagnostic accuracy of the 64-slice MDCT protocol in our study group. Secondly, the stratification of assessable coronary artery segments did not take into consideration their respective diameters, an important parameter with regard to subsequent therapeutic options. Thirdly, all studies were evaluated by two radiologists in a joint review manner. A separate data evaluation would have allowed an investigation of the interobserver variability in coronary artery assessment. Lastly, the studied group was limited to 133 patients, and our preliminary results should be confirmed by further investigations.
In conclusion, high-quality coronary imaging without administration of β-blockers can be obtained in routine ECG-gated 64-slice MDCT examinations of the entire thorax for patients with a heart rate below 80 bpm with a reasonable radiation exposure. Because of CT technological developments, it appears that a CT examination of the chest wall is no longer dissociable from an examination of the heart; a trend toward cardiothoracic imaging is going to be reinforced with the next generation of scanners using a dual tube.
References
Achenbach S, Giesler T, Ropers D et al (2001) Detection of coronary artery stenoses by contrast-enhanced, retrospectively electrocardiographically-gated, multislice spiral computed tomography. Circulation 103:2535–2538
Knez A, Becker CR, Leber A et al (2001) Usefulness of multislice computed tomography angiography for determination of coronary artery stenoses. Am J Cardiol 88:1191–1194
Nieman K, Rensing BJ, van Geuns RJ et al (2002) Usefulness of multislice computed tomography for detecting obstructive coronary artery disease. Am J Cardiol 89:913–918
Nieman K, Rensing BJ, van Geums RJM et al (2002) Non-invasive coronary angiography with multislice spiral computed tomography: the impact of the heart rate. Heart 88:470–474
Nieman K, Cademartiri F, Lemos PA, Raaijmakers R, Pattynama PM, Reyter PJ (2002) Reliable noninvasive coronary angiography with fast submillimeter multislice spiral computed tomography. Circulation 106:2051–2054
Ropers D, Baum U, Pohle K, Anders K, Ulzheimer S, Ohnesorge B, Schlundt C, Bautz W, Daniel WG, Achenbach S (2003) Detection of coronary artery stenoses with thin-slice multidetector row spiral computed tomography and multiplanar reconstruction. Circulation 107:664–666
Mollet NR, Cademartiri F, Krestin G, McFadden EP, Arampatzis CA, Serruys PW, de Feyter PJ (2005) Improved diagnostic accuracy with 16-row multislice computed tomography coronary angiography. J Am Coll Cardiol 45:128–132
Heuschmid M, Kuettner A, Schroeder S, Trabold T, Feyer A, Seemann M, Kuzo R, Claussen CD, Kopp AF (2005) ECG-gated 16-MDCT of the coronary arteries: assessment of image quality and accuracy in detecting stenoses. AJR Am J Roentgenol 184:1413–1419
Hoffmann MHK, Shi H, Manzke R, Schmid FT, De Vries L, Grass M, Brambs HJ, Aschoff AJ (2005) Noninvasive coronary angiography with 16-detector row CT: effect of heart rate. Radiology 234:86–97
Oldershaw P (1992) Assessment of right ventricular function and its role in clinical practice. Br Heart J 68:12–15
Multiple risk factor intervention trial research group (1982) Multiple risk factor intervention trial. Risk factor changes and mortality results. JAMA 248:1465–1477
Salem R, Remy-Jardin M, Delhaye D, Khalil C, Teisseire A, Delannoy-Deken V, Duhamel A, Remy J (2006) Integrated cardiothoracic imaging with ECG-gated 64-slice multidetector-row CT: preliminary experience in 133 patients. Eur Radiol (in press)
Jakobs TF, Becker CR, Ohnesorge B, Flohr T, Suess C, Schoepf UJ, Reiser MF (2002) Multislice helical CT of the heart with retrospective ECG gating: reduction of radiation exposure by ECG-controlled tube current modulation. Eur Radiol 12:1081–1086
American Heart Association Committee Report (1979) A reporting system on patients evaluated for coronary artery disease. Circulation 51:7–34
Schroeder S, Kopp AF, Kuettner A et al (2002) Influence of heart rate on vessel visibility in noninvasive coronary angiography using new multislice computed tomography: experience in 94 patients. Clin Imaging 26:106–111
Zhang SZ, Hu XH, Zhang QW, Huang WX (2005) Evaluation of computed tomography coronary angiography in patients with a high heart rate using 16-slice spiral computed tomography with 0.37-s gantry rotation time. Eur Radiol 15:1105–1109
Hamoir XL, Flohr T, Hamoir V, Labaki L, Tricquet JY, Duhamel A, Kirsch J (2005) Coronary arteries : assessment of image quality and optimal reconstruction window in retrospective ECG-gated multislice CT at 375 ms gantry rotation time. Eur Radiol 15:296–304
Becker CR (2005) Coronary CT angiography in symptomatic patients. Eur Radiol 15 (suppl 2):B33–B41
Martuschelli E, Romagnoli A, D’Eliseo A, Razzini C, Tomassini M, Sperandio M, Simonetti G, Romeo F (2004) Accuracy of thin-slice computed tomography in the detection of coronary stenoses. Eur Heart J 25:1043–1048
Shim SS, Kim Y, Lim SM (2005) Improvement of image quality with beta-blocker premedication on ECG-gated 16-MDCT coronary angiography. AJR Am J Roentgenol 184:649–654
Hong C, Becker CR, Huber A, Schoepf UJ, Ohnesorger B, Knez A et al (2001) ECG-gated reconstructed multi-detector-row CT coronary angiography: effect of varying trigger delay on image quality. Radiology 220:712–717
Achenbach S, Moshage W, Ropers D, Bachmann K (1998) Curved multiplanar reconstructions for the evaluation of contrast-enhanced electron-beam CT of the coronary arteries. AJR Am J Roentgenol 170:895–899
Giesler T, Baum U, Ropers D et al (2002) Noninvasive visualization of coronary arteries using contrast-enhanced multidetector CT: influence of heart rate on image quality and stenosis detection. AJR Am J Roentgenol 179:911–916
Leschka S, Alkadhi H, Plass A, Desbiolles L, Grunenfelder J, Marincek B, Wildermuth S (2005) Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur Heart J 26:1482–1487
Leber AW, Knez A, Becker A et al (2004) Accuracy of multidetector spiral computed tomography in identifying and differentiating the composition of coronary atherosclerotic plaques: a comparative study with intracoronary ultrasound. J Am Coll Cardiol 43:1241–1247
Leber AW, Knez A, von Ziegler F, Becker A, Nikolaou K, Paul S, Wintersperger B, Reiser M, Becker CL, Steinbeck G, Boekstegers P (2005) Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol 46:147–154
Bley TA, Ghanen NA, Foell D, Uhl M, Geibel A, Bode C, Langer M (2005) Computed tomography coronary angiography with 370-millisecond gantry rotation time: evaluation of the best image reconstruction interval. J Comput Assist Tomgr 29:1–5
Kopp AF, Schroeder S, Kuettner A, Heuschmid M, Georg C, Ohnesorge B, Kuzo R, Claussen CD (2001) Coronary arteries: retrospectively ECG-gated multidetector row CT angiography with selective optimization of the image reconstruction window. Radiology 221:683–688
EC99. European guidelines on quality criteria for computed tomography. Report EURO 16262 EN. Luxembourg 1999; 69–78
Trabold T, Buchgeister M, Kuttner A et al (2003) Estimation of radiation exposure in 16-detector row computed tomography of the heart with retrospective ECG-gating. Röfo 175:1051–1055
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Delhaye, D., Remy-Jardin, M., Salem, R. et al. Coronary imaging quality in routine ECG-gated multidetector CT examinations of the entire thorax: preliminary experience with a 64-slice CT system in 133 patients. Eur Radiol 17, 902–910 (2007). https://doi.org/10.1007/s00330-006-0403-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-006-0403-2