Abstract
The aim of the study was to determine the potential diagnostic value of contrast-enhanced echocardiogram (ECG)-gated multidetector computed tomography (MDCT) in the setting of suspected acute myocarditis compared with contrast-enhanced magnetic resonance imaging (MRI). The study group consisted of 12 consecutive patients admitted for suspected acute myocarditis less than 10 days after onset of symptoms. All patients had clinical, electrocardiographic signs, and laboratory findings consistent with the diagnosis. All patients but one (severe claustrophobia) underwent cardiac MRI using T1-weighted delayed-enhancement images after injection of gadolinium. ECG-gated MDCT was performed in all patients and included a first-pass contrast-enhanced acquisition and a delayed acquisition. MRI revealed abnormal focal or multifocal myocardial enhancement and confirmed the diagnosis in 11 patients. The first-pass MDCT acquisition showed homogenous left-ventricle contrast enhancement and absence of coronary stenosis in all patients. Delayed MDCT acquisition, performed 5 min later without reinjection of contrast medium revealed multiple areas of myocardial hyperenhancement in a focal or a multifocal pattern (six and six patients, respectively). Extent and location of hyperenhancement at MDCT correlated well with that observed at MR examination for all 11 patients evaluated by both techniques (r=0.9167, p=0.0004). These preliminary results show that ECG-gated MDCT could be a useful alternative noninvasive diagnostic test in the early phase of acute myocarditis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Acute myocarditis, defined as inflammation of the heart muscle, is an infectious or immunological disease that displays a wide spectrum of clinical patterns. It is usually an asymptomatic disease, as shown by the results of postmortem studies, or it can be responsible for acute chest pain and thus mimic acute myocardial infarction. However, it can also be responsible for major alterations to cardiac function, leading to acute cardiac failure and cardiogenic shock. Diagnosis of myocarditis is often difficult. Despite the poor sensitivity of endomyocardial biopsy, histological studies remain the gold standard [1]. Noninvasive diagnosis tests would be valuable because of the invasive character and diagnostic limitations of histological studies, largely due to insufficient specimen harvest. Indium 111 antimyosin antibody scintigraphy and contrast-enhanced magnetic resonance imaging (MRI) are useful in this setting [2, 3]. Contrast-enhanced MRI provides an accurate assessment of the site and activity of inflammation and is now routinely used for the diagnosis of myocarditis vs acute myocardial infarction [4]. Since the introduction of continuous spiral techniques with electrocardiogram (ECG) synchronization, computed tomography (CT) can achieve high-quality image reconstructions of the left-ventricle (LV) myocardium. ECG-gated multidetector computed tomography (MDCT) has shown altered myocardial contrast enhancement patterns in areas of myocardium necrosis early after myocardial infarction [5]. However, nothing is known about the value of MDCT for the diagnosis of acute myocarditis. We then undertook a preliminary prospective study to evaluate MDCT myocardial contrast enhancement patterns and to compare MDCT and MRI results in the early phase of acute myocarditis.
Methods
Study group
Over a 24-month period, 12 consecutive patients admitted for suspicion of acute myocarditis based on clinical, ECG, and biological grounds, were enrolled in the study and evaluated by MDCT and MRI within 10 days of the onset of chest pain and within 48 h one from the other in all patients but one. No patient presented with exclusion criteria [i.e., iodine allergy, severe renal insufficiency, or prior myocardial infarction). Topography of ECG signs, creatine kinase (CK), troponin I, and C-reactive protein (CRP) peak blood value were recorded. Usual serological tests [Epstein Barr virus (EBV), cytomegalovirus (CMV), human immunodeficiency virus (HIV), hepatitis B virus (HBV), Cocksakie, and Lyme] were performed. To rule out significant coronary stenosis, nine patients (patients 1–7, 10, and 11) underwent coronary angiography. Follow-up involved clinical examination 6±2 weeks after admission. Diagnosis of myocarditis was confirmed by MRI examination and the absence of alternative diagnosis at follow-up. All studies were performed according to the guidelines of the hospital committee on medical ethics and clinical investigation. Written informed consent was obtained from all patients.
MDCT protocol
MDCT studies were performed with a multidetector-row scanner (Siemens AG, Erlangen, Germany) using ECG synchronized tube modulation. Patients were evaluated by either 4-slice (patients 1–3) or 16-slice MDCT (patients 4–12). Patients with heart rate >70/min were given a single oral dose of 50–100 mg atenolol 1 h before the examination. During MDCT, a first acquisition (120 kVp, 500 mAs) was performed following injection at 3.5 cc/s of 1.5 cc/kg nonionic iodinated contrast medium (Iopamidol 370, Schering SA, Berlin, Germany). A delayed acquisition (80 kVp, 500 mAs) was done 5 min later without any additional injection of contrast medium. Images were reconstructed retrospectively at the diastolic phase (at 60% of the start of RR interval). The LV was imaged using two long axis views (one four-chamber and one two-chamber view) and two short axis views (basal and medium views). Variations of myocardial enhancement (hypo or hyper) were assessed visually for the two phase acquisitions by two observers to give a consensus reading, using MPR images, with a slice width of 8 mm. For the nine patients evaluated with 16-slice MDCT (patients 4–12), the presence of coronary stenosis was also assessed on thin-slab maximum-intensity projection (MIP) images for each main coronary artery (>2 mm in diameter) using the first-pass acquisition (arterial phase).
MRI protocol
During MRI studies, all patients were examined in the supine position holding their breath at tidal inspiration. MRI examinations were performed on a state-of-the-art 1.5-T MRI system (General Electric TwinSpeed, Milwaukee, WI, USA) using a dedicated, five-element cardiac phased-array surface coil. The imaging protocol included: (a) gradient echo imaging in the three orthogonal planes of the chest (scout localization imaging) to locate the long axis, then the short axis and four chamber views; (b) first-pass perfusion short-axis contrast-enhanced interleaved gradient-echo single-shot T1-weighted acquisitions with echo-planar imaging (EPI)-like readout, six to eight slices encompassing the LV according to the heart rate, time resolution of two RR intervals; (c) short-axis breath-hold cine steady-state free precession (SSFP) acquisitions; and (d) short-axis contrast-enhanced gradient-echo T1-weighted acquisitions with an inversion time of 175–240 ms to null the signal of normal myocardium according to the delay after injection. All acquisitions were cardiac gated using prospective triggering. All sequences were acquired at the same slice positions. First-pass perfusion imaging sequences encompassing the overall LV myocardium were performed after bolus infusion via a power injector of 0.1 mmol (i.e., 12–20 ml) of gadoterate dimeglumine (Dotarem; Guerbet, Aulnay-sous-Bois, France) per kilogram of body weight at a rate of 3–4 ml/s followed by a 25-ml saline flush at the same rate. The same amount of gadolinium (Gd) chelate was injected again at the end of the first-pass study to ensure sufficient contrast between normal and diseased areas on the following delayed-enhancement sequences. Consequently, the total dose before late enhancement imaging was 0.2 mmol/kg. Contrast-enhanced cine SSFP acquisitions were performed immediately before starting the delayed-enhancement sequence. Delayed-enhancement study was performed in diastole 10 min after the second injection.
Image analysis
CT and MR images were assessed by two observers (one radiologist and one cardiologist) without knowledge of the results of other corroborative studies. For both techniques, abnormalities were described following a segment-by-segment analysis. The LV myocardium was divided into 17 segments covering the entire LV [6]. The 17-segment-model analysis was used to assess the extent of contrast enhancement abnormalities in terms of the number of segments involved. Both enhancement of the subendocardial/subepicardial/centromyocardial/transmural location and enhancement pattern (nodular, band like) were described for each diseased segment. A vascular distribution was scored as present if any of the following sites were involved: anterior and/or septal for left anterior descending artery, lateral for left circumflex artery, and inferior for right coronary artery, with a clear delineation between the vascular area involved and the remaining myocardium.
Statistical analysis
Myocardial enhancement patterns obtained with the two techniques were compared segment by segment. Statview J-5.0 software (Abacus Concepts, Inc. Berkeley, CA, USA) was used for statistical analysis: analysis of variance (ANOVA) factorial analyses for quantitative values expressed as mean ± standard deviation (SD), the chi-square test for location of abnormalities, and the Mann–Whitney U test for number of segments involved in each group. A p value <0.05 was considered significant.
Results
Clinical description and outcome
Clinical features of the 12 patients are summarized in Table 1. There were 11 men and one woman. No patient had history of prior myocardial infarction. All patients had a clinically obvious infectious episode less than 2 weeks prior to admission. The primary symptom was acute chest pain in all patients. No patients had dyspnea or sign of cardiac failure. The mean serum concentration of CK was 460±276 ui/l, troponin I 8.4±6.5 ng/ml, and CRP 81±35 mg/l. ECG changes in the ST segment (ST elevation in four and ST depression in six patients) and T waves (T-wave inversion in eight patients) were observed in the inferior and/or lateral leads in eight patients and were diffuse in four patients. Echocardiography was normal in three patients but revealed regional abnormalities of LV wall motion in nine patients. Coronary angiography revealed no significant coronary stenosis in the nine patients tested. All patients were discharged without any complication; nine were treated with angiotensin converting enzyme (ACE) inhibitors. At follow-up (6±2 weeks), no patient had any complication (heart failure, arrhythmias, or sudden death) or any recurrent chest-pain episode. Final diagnosis of myocarditis was confirmed at follow-up in all patients in the absence of any alternative diagnosis.
MDCT study
The 12 patients underwent MDCT evaluation with a mean delay of 4±3 (range 1–9) days after onset of chest pain. In all studies, image quality was sufficient for evaluation of myocardial density changes. MDCT first-pass acquisition revealed homogenous contrast enhancement of the whole LV myocardium in all patients (Fig. 1). MIP reconstructions of the main coronary arteries of the nine patients evaluated with 16-slice MDCT (patients 4–12) revealed no significant stenosis in any patient.
Iodinated contrast-enhanced electrocardiogram (ECG)-gated multidetector computed tomography (MDCT) four-chamber (a, c) and short-axis (b, d) views in patient 11. Upper images (a, b) show first-pass acquisition a few seconds after iodine injection. Lower images (c, d) show delayed acquisition 5 min after injection (arrowheads in c, d show subepicardial nodular enhancement). RV right ventricle; LV left ventricle
MDCT delayed acquisitions revealed myocardial late hyperenhancement in all patients. Abnormal myocardial enhancement appeared as nodular or band-like bright areas within the LV wall (Fig. 1). Abnormal myocardial enhancement was transmural in some cases and subepicardial in others but never only subendocardial. In four patients, late enhancement appeared also as thin patchy nodules within the LV wall. The mean extent of enhancement was 9±2 segments (range 7–12 segments). Late enhancement was present in the lateral wall of the LV in all patients and extended to the anterior wall or inferior wall in seven and two patients, respectively. In four patients, we observed a mild enhancement of the interventricular septum (Figs. 2 and 3). Six patients had multiple areas of enhancement scattered throughout the LV in a nonvascular, multifocal distribution.
Patient 7 with acute myocarditis predominating at an inferior and lateral location. Short axis images from multidetector computed tomography (MDCT) (a) and magnetic resonance imaging (MRI) (b) obtained close to the same level show similar subepicardial enhancement. However, the extent of subepicardial involvement in a is greater than in b, and a centromyocardial anteroseptal band of hyperenhancement is only seen in a (arrowheads). RV right ventricle; LV left ventricle
MRI study
MR studies were performed 5±3 (range 2–9) days after the acute event. One patient (patient 5) with severe claustrophobia could not undergo MRI evaluation despite use of sedative drugs. In this patient, the diagnosis of myocarditis was based on clinical grounds and the absence of an alternative diagnosis at either discharge or follow-up. First-pass perfusion studies were normal in all 11 patients examined. Delayed-enhancement sequences showed myocardial abnormalities in all these patients, with the mean number of segments involved being 8.8±2 (range 7–12) segments. The abnormal enhancement patterns included hyperenhancing nodules and transmural involvement in a focal form in six patients and a multifocal form in five patients. Location of enhancement within the myocardium was subepicardial, centromyocardial, or mixed subepicardial and centromyocardial. Abnormal delayed enhancement involved the lateral wall of the LV in all patients and the anterior or inferior wall in seven and two patients, respectively.
Comparison of MDCT and MRI results
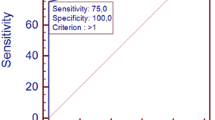
Results are summarized in Figs. 4 and 5. For the 11 patients evaluated by both techniques, MRI and MDCT studies gave similar results for the extent of late enhancement (8.8±2 and 9±2 segments, respectively, p<0.05). There was also a good correlation between the two methods in the number of segments involved (Spearman, y=(1.17)×−1.17, r=0.9167, p=0.0004). A focal distribution of late enhancement was found in six patients with both MRI and MDCT. Segment-by-segment comparison showed a high level of correlation (y=(0.93)×+0.12, r=0.90, p<0.0001). However, there were some differences between both methods in localization of detected enhancement: CT showed more enhancement in apical segments and the anterior wall while MR showed slightly more involved segments in the inferior and lateral wall.
Discussion
Our study shows that ECG-gated MDCT demonstrated constant areas of myocardial delayed hyperenhancement in cases of acute myocarditis. Moreover, there was a high degree of correlation between the results of MDCT and MRI performed less than 7 days after onset of chest pain and within 48 h of one from the other in all patients but one.
The diagnosis of myocarditis remains difficult and mostly dependent on clinical suspicion. When acute myocarditis is revealed by chest pain symptoms, it can mimic myocardial infarction [7]. In this study, clinical grounds, ECG, and laboratory and echocardiographic data were presumptive of the diagnosis, and in nine of the patients, emergency coronary angiography ruled out acute coronary syndrome. We did not perform endomyocardial biopsy, the reference diagnostic technique. Because of its invasive character and its lack of sensitivity [8], it is not routinely used in our institution for acute myocarditis. Several studies [3, 4, 9] have reported the usefulness of contrast-enhanced T1-weighted MRI acquisitions, which allow assessment of localization, activity, and extent of inflammation in cases of acute myocarditis. A recent study [10] showed that increased myocardial delayed-enhancement with MRI correlated well with the presence of active inflammation detected by histopathology of samples harvested from endomyocardial biopsies. Cardiac MRI showed no abnormalities in precontrast T1-weighted images and constant myocardial hypersignal in postcontrast T1-weighted images in our study group, thereby confirming the presumptive diagnosis of myocarditis.
Previous studies using dual-phase contrast enhancement ECG-gated MDCT have reported constant abnormalities of myocardial contrast enhancement patterns early after acute myocardial infarction [5, 11, 12]. Early enhancement defects on the first-pass acquisition as well as late enhancement on the delayed acquisition were observed in the area of myocardial infarction. In our study, first-pass acquisition revealed no myocardial enhancement defect. However, as myocarditis could mimic acute myocardial coronary syndrome, this first-pass acquisition was useful to rule out atheromatous lesions in coronary arteries. Even if CT is not the gold standard to assess coronary arteries, high-resolution images obtained with 16 slices ECG-gated MDCT acquisitions can rule out coronary stenosis with a specificity of 86–97% and a constant high negative predictive value (95–99%) [13–15]; therefore, it can be used in the setting of acute myocarditis to eliminate the presence of a significant coronary lesion. Normal coronary arteries on first-pass acquisition may then exclude any coronary atherosclerosis with a high probability. Our study showed that CT ruled out coronary artery disease in the nine patients with normal coronary angiograms; assessment of coronary arteries neither prolonged CT examination nor increased X-ray or contrast agent dose.
In the present study, hyperenhancement affected any of the regions of the LV but was mainly present in the lateral wall in all patients. This agreed with previous MRI studies [4, 10] in which delayed hypersignal was mostly observed in the lateral free wall. Consistent with the myocardial hypersignal in MRI studies, hyperenhancement could be transmural, subepicardial, or confined to a layer of the myocardium wall (as small foci within the myocardium). Another study [9] reported that the hypersignal evolved from a focal to a diffuse pattern as a function of the time delay between onset of chest pain and MRI. As all MDCT examinations were performed early (less than 10 days after chest pain in all patients), we could not assess the diffusion of myocardial enhancement with time.
Histological studies during the early phase of acute myocarditis reveal interstitial lymphocytic infiltration, cell damage, interstitial edema, and hyperemia [1]. The interpretation of contrast enhancement as shown by cardiac MRI has been described by Mahrholdt et al. [10]. Iodine contrast is a nonspecific contrast agent, such as Gd-chelate, that concentrates in extravascular space, which explains that we observed the same results with gadolinium-enhanced cardiac MRI and iodine-enhanced MDCT. Myocyte membrane rupture leading to increased extracellular space volume, increased vascular permeability responsible for an increased distribution volume of iodine contrast, and diminished clearance could explain why enhancement persisted longer in regions involved in myocarditis than in adjacent normal myocardium as detected by MDCT delayed-enhancement acquisition. During the myocarditis process, areas of cell necrosis are small and disseminated throughout the whole myocardium. This could explain the multifocal pattern of myocardial enhancement observed in some patients.
Study limitations
This preliminary studied involved, of course, a small number of patients, limiting the value of statistical results. We did not perform endomyocardial biopsy because of its invasive character and its lack of sensitivity, particularly in the early phase of acute myocarditis. We used cardiac MRI as the reference diagnostic technique because delayed MRI hyperenhancement and histological findings have previously shown good agreement [10]. There was a high correlation between the MRI and MDCT findings in our study even though the delayed-enhancement sequences used with the two techniques were obtained at slightly different times after contrast injection (5 and 10 min with MDCT and MRI, respectively): this may explain some differences in the distribution of abnormalities. Indeed, little is known about the washin and washout kinetics of cardiac inflammatory lesions such as in acute myocarditis. The time after injection of contrast medium is of importance for detecting late enhancement. A recent study [4] has shown that a delay of 10 min with MRI could differentiate acute myocarditis and acute myocardial infarction. With CT, we arbitrarily chose a standard delay of 5 min after injection on the basis of initial cases and for ethical reasons, we did not perform repeated acquisitions at different times. The same two-phase protocol, with a 5-min delay between the two acquisitions, has shown to be adequate in postinfarction LV evaluation [16]. A different time lag between injection and acquisition may result in different findings, but this delay was associated with a good correlation in this preliminary work even if some slight differences of localization were observed. No attempt was made to assess LV function with MDCT by comparison with MRI, but a recent study showed acceptable agreement between the two techniques [12].
As few as 2% of patients experience claustrophobia with MRI. In one patient that could not undergo MRI because of severe claustrophobia but could be evaluated by MDCT without any problem, the diagnosis of myocarditis was based on clinical, biological, and ECG data and on the absence of alternative diagnosis at follow-up.
There are some difficulties to design an optimal protocol for detection of myocardial late enhancement in CT. Based on the methods of previous studies assessing MDCT after acute myocardial infarction, we used a two-phase acquisition protocol. Radiation dose may be high using cardiac CT (up to 15 mSv), so we used an ECG-pulsing technique and weight-adapted settings in a systematic manner to decrease radiation dose by a factor of at least two in the early phase. In addition, we lowered the kilovoltage to 80 kV for the delayed acquisition to give better visualization of contrast uptake in the myocardium (iodine has a high atomic number, responsible for more attenuation at lower kV settings) [17]. This 80-kV setting allowed a further 66% reduction in dose for delayed images, similar to the dose reduction recently reported [18]. In addition, radiation dose in the delayed phase was estimated to be only 2 mSv (typically, dose product length value was 120 mGy/cm for an ECG-gated acquisition at 80 kV and 500 mAs). This low dose acquisition was responsible for noisy native images, but noise was strongly reduced using 8-mm-thick multiplanar slice reconstructions, making assessment of myocardial changes possible in all cases of the series. Although MDCT results in this small study population were relatively constant, larger studies are required to assess the clinical value of MDCT in the diagnosis of acute myocarditis.
In conclusion, this preliminary study shows that two-phase (early and 5-mn delayed) iodine enhanced ECG-gated MDCT in the early phase of acute myocarditis correlated with the results of gadolinium enhanced cardiac MRI in terms of detection and extent of late enhancement abnormalities. This late enhancement in myocarditis has been well established. The potential advantage of MDCT over MRI is the incremental value of a 2-phase protocol, i.e.: at first pass, coronary atheromatous lesion may be excluded, making myocardial infarction unlikely; evidence of subepicardial late enhancement on the second phase supports the diagnosis of myocarditis. Also MDCT examination time is shorter, and its availability is greater in emergency situations. ECG-gated MDCT, by ruling out any significant coronary stenosis and assessing myocardial contrast enhancement within a single examination, could be useful in cases of chest pain with non diagnostic ECG.
Abbreviations
- MDCT:
-
multidetector computed tomography
- MRI:
-
magnetic resonance imaging
- CK:
-
creatine kinase
- CRP:
-
C reactive protein
- LV:
-
left ventricle
- ACE inhibitors:
-
angiotensin-converting enzyme inhibitors
References
Fenoglio JJ Jr, Ursell PC, Kellogg CF et al (1983) Diagnosis and classification of myocarditis by endomyocardial biopsy. N Engl J Med 308:12–18
Dec GW, Palacios I, Yasuda T et al (1990) Antimyosin antibody cardiac imaging: its role in the diagnosis of myocarditis. J Am Coll Cardiol 16:97–104
Friedrich MG, Strohm O, Schulz-Menger J et al (1998) Contrast media-enhanced magnetic resonance imaging visualizes myocardial changes in the course of viral myocarditis. Circulation 97:1802–1809
Laissy JP, Hyafil F, Feldman LJ et al (2005) Differentiating acute myocardial infarction from myocarditis: diagnostic value of early- and delayed-perfusion cardiac MR imaging. Radiology 237:75–82
Wada H, Kobayashi Y, Yasu T et al (2004) Multi-detector computed tomography for imaging of subendocardial infarction: prediction of wall motion recovery after reperfused anterior myocardial infarction. Circ J 68:512–514
Cerqueira MD, Weissman NJ, Dilsizian V et al (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105:539–542
Sarda L, Colin P, Boccara F et al (2001) Myocarditis in patients with clinical presentation of myocardial infarction and normal coronary angiograms. J Am Coll Cardiol 37:786–792
Felker GM, Thompson RE, Hare JM, Hruban RH et al (2000) Underlying causes and long-term survival in patients with initially unexplained cardiomyopathy. N Eng J Med 342:1077–1084
Laissy JP, Messin B, Varenne O et al (2002) MRI of acute myocarditis: a comprehensive approach based on various imaging sequences. Chest 122:1638–1648
Mahrholdt H, Goedecke C, Wagner A et al (2004) Cardiovascular magnetic resonance assessment of human myocarditis: a comparison to histology and molecular pathology. Circulation 109:1250–1258
Koyama Y, Matsuoka H, Mochizuki T et al (2005) Assessment of reperfused acute myocardial infarction with two-phase contrast-enhanced helical CT: prediction of left ventricular function and wall thickness. Radiology 235:804–811
Kopp AF, Heuschmid M, Reimann A et al (2005) Evaluation of cardiac function and myocardial viability with 16- and 64-slice multidetector computed tomography. Eur Radiol 15(Suppl 4):D15–D20
Ropers D, Baum U, Pohle K et al (2003) Detection of coronary artery stenoses with thin-slice multi-detector row spiral computed tomography and multiplanar reconstruction. Circulation 107:664–666
Kuettner A, Kopp AF, Schroeder S et al (2004) Diagnostic accuracy of multidetector computed tomography coronary angiography in patients with angiographically proven coronary artery disease. J Am Coll Cardiol 43:831–839
Dorgelo J, Willems TP, Geluk CA et al (2005) Multidetector computed tomography-guided treatment strategy in patients with non-ST elevation acute coronary syndromes: a pilot study. Eur Radiol 15:708–713
Paul JF, Wartski M, Caussin C et al (2005) Late defect on delayed contrast-enhanced multi-detector row CT scans in the prediction of SPECT infarct size after reperfused acute myocardial infarction: initial experience. Radiology 236:485–489
Sigal-Cinqualbre AB, Hennequin R, Abada HT et al (2004) Low-kilovoltage multi-detector row chest CT in adults: feasibility and effect on image quality and iodine dose. Radiology 231:169–174
Hohl C, Muhlenbruch G, Wildberger JE et al (2006) Estimation of radiation exposure in low-dose multislice computed tomography of the heart and comparison with a calculation program. Eur Radiol Feb 3;1–6 (E-pub ahead of print)
Acknowledgement
The authors wish to declare no competing interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dambrin, G., Laissy, J.P., Serfaty, J.M. et al. Diagnostic value of ECG-gated multidetector computed tomography in the early phase of suspected acute myocarditis. A preliminary comparative study with cardiac MRI. Eur Radiol 17, 331–338 (2007). https://doi.org/10.1007/s00330-006-0391-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-006-0391-2