Abstract
Extracranial arterial dissections are a recognised cause of stroke, particularly in young adults. Clinical diagnosis may be difficult, and the classical triad of symptoms is uncommon. Imaging plays a pivotal role in the diagnosis of extracranial arterial dissections, and this review provides a detailed discussion of the relative merits and limitations of currently available imaging modalities. Conventional arteriography has been the reference standard for demonstrating an intimal flap and double lumen, which are the hallmarks of a dissection, and for detecting complications such as stenosis, occlusion or pseudoaneurysm. Noninvasive vascular imaging methods, such as ultrasound (US), magnetic resonance angiography (MRA) and computed tomography angiography (CTA) are increasingly replacing conventional angiography for the diagnosis of carotid and vertebral dissections. Ultrasound provides dynamic and “real-time” information regarding blood flow. Source data of MRA and CTA and additional cross-sectional images can provide direct visualisation of the mural haematoma and information about the vessel lumen. Anticoagulation to prevent strokes is the mainstay of medical treatment, but randomised trials to define the optimal treatment regime are lacking. Surgery has a limited role in management of dissections, but endovascular procedures are gaining importance for treatment of complications and if medical management fails.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Extracranial carotid artery dissection is an uncommon cause of stroke, accounting for less than 1% of all strokes. It is, however, an important cause of stroke in young adults (mean age of occurrence 25–45 years) with an estimated incidence of 10–25% [1, 2]. The overall incidence of internal carotid artery (ICA) dissection is 2–3 per 100,000 per year [3] and that of vertebral artery (VA) dissection approximately 1–1.5 per 100,000 [4]. The first description of an extracranial ICA dissection was reported by Jentzer in 1954 [5]. The increased diagnosis of this condition in the last decade can be attributed to the availability of diagnostic imaging techniques, such as colour Doppler ultrasound (US), computed tomography (CT) and magnetic resonance (MR) imaging. In addition, there is also an increased awareness of the diverse clinical spectrum of ICA and VA dissection.
Pathogenesis
A dissection is termed spontaneous if there is no evidence of preceding trauma. The most common cause of a traumatic dissection is blunt (severe hyperextension) or penetrating (stab wound) injury to the neck [6, 7]. There are however, no angiographic differences between spontaneous and traumatic dissections [8, 9]. External trauma may be minimal. VA dissection has been associated with stroke following long-haul air travel. The dissection was attributed to an uncomfortable neck posture with prolonged hyperextension or lateral rotation of the cervical spine [10] or simultaneous bilateral internal carotid and VA dissection following chiropractic neck manipulation [11]. Spontaneous extracranial dissection may be linked with an underlying arteriopathy, and fibromuscular dysplasia (FMD) can be found in up to 15% of patients with ICA or VA dissections [12]. Other connective tissue diseases are identified in 1–5% of patients with spontaneous ICA or VA dissections and include Ehlers-Danlos syndrome type IV, Marfan’s syndrome, autosomal dominant adult polycystic kidney disease, osteogenesis imperfecta type I and cystic medial necrosis [13, 14]. Many vascular risk factors are associated with arterial dissection although no single factor alone seems to be responsible [15]. Hypertension is present in up to 53% [16–20]; diabetes mellitus [17], smoking [17, 20, 21], hyperlipidemia [17] and the oral contraceptive pill [17, 19, 20, 22] are also linked. The pathogenesis of spontaneous dissection is often uncertain, and the dissection occurs usually in an area of macroscopically normal intima [23].
The mechanism of dissection is thought to be either a tear in the intima of the vessel, which allows intraluminal blood to dissect along the layers of the vessel wall or, alternatively, direct haemorrhage from the vasa vasorum of the media into the arterial wall. In both scenarios, the haematoma dissects longitudinally through the media. Luminal narrowing or total occlusion occurs if the haematoma lies just beneath the intima. If the haematoma dissects just beneath the adventitia, a pseudoaneurysm forms [24], and a false lumen occurs if blood reenters the true lumen. The false lumen may either remain patent, resolve completely, or thrombose and cause narrowing of the true lumen [25]. The thrombosed dissection lumen may, particularly in the acute stage, become the source of distal emboli presenting as a transient ischaemic attack (TIA) or stroke [24].
Clinical features
The classical triad of presentation of an extracranial ICA dissection is ipsilateral headache, facial or neck pain and partial Horner’s syndrome, followed hours or days later by cerebral or retinal ischaemia (amaurosis fugax). This triad of symptoms is found in less than one third of patients, but the presence of two elements of this triad strongly suggests the diagnosis. Other manifestations include syncope, neck swelling, cranial nerve dysfunction (cranial nerves IX, X and XII) and pulsatile tinnitus. In more than 50% of patients, the clinical picture does not suggest the diagnosis of spontaneous ICA dissection [15]. Cerebral infarcts are reported in 40–60% and TIA in 20–30% of patients with ICA dissection [26]. Most infarcts are thought to be embolic in origin and can be cortical or subcortical in location [27]. Less commonly, the infarct may be haemodynamic in origin due to reduced blood flow through a narrowed ICA lumen [28]. In 5% of cases, an ICA dissection remains asymptomatic.
Extracranial VA dissection may be asymptomatic or present with nonspecific complaints, such as dizziness or vertigo [29], amnesia, tinnitus, hemianopia, nausea and vomiting [19–21] or posterior cerebral circulation infarcts [30, 31]. Horner’s syndrome is reported in 36% [21] and cranial nerve dysfunction is seen in up to 13% of cases[32, 33]. Intracranial ICA dissection is rarer, occurs in a younger age group (mean age 25 years) and has a less favourable clinical outcome with a mortality rate of 75% [34]. The onset of symptoms is usually rapid, often associated with a subarachnoid haemorrhage (SAH), massive stroke and death [2]. Dissection of the intracranial VA is also less common and almost exclusively spontaneous [20, 35] and can result in SAH and pseudoaneurysm formation [36]. This is attributed to the fact that the intradural segment of the VA has a thinner media and adventitia with less prominent vasa vasorum, which may limit healing [37]. Intracranial VA dissections are frequently fatal, with the mortality rate estimated at 46% [37]. Intracranial VA dissections can lead to the formation of posterior inferior cerebellar artery (PICA) aneurysms that may subsequently rupture and present with subarachnoid haemorrhage.
Dissection sites
In a review of 200 patients with spontaneous extracranial artery dissection, the ICA was affected in 76% (unilateral in 62% and bilateral in 14%), the VA in 18% and both ICA and VA in 6% [38]. The commonest location for a spontaneous ICA dissection is the cervical segment 2–3 cm distal to the carotid bulb, an area that is probably subject to most of the stretch during extension or rotation of the neck. Dissections extend for a variable length cranially but not usually past the point of entry of the ICA into the petrous temporal bone. VA dissections are most common in the distal segment of the artery at the level of the first and second cervical vertebrae [25]. Multiple-vessel disease is common, being found in 16–28% patients with ICA dissection [31, 39, 40]. This could be due to underlying arteriopathy that would increase the risk of recurrent dissection. In the absence of an arteriopathy, recurrent dissection in the same vessel or other cervicocephalic arteries is very rare [26, 41].
Imaging
Intraarterial angiography
Intraarterial angiography has been the reference standard for diagnosis of dissections. Angiography is, however, an invasive procedure and not without risk [42]. It is increasingly being replaced by noninvasive imaging modalities, both for primary diagnosis and follow-up of dissections. Angiography will demonstrate the arterial lumen and detect associated vessel wall irregularities, such as FMD, but may miss dissections when the false lumen does not opacify with contrast medium [43, 44]. Angiography does not allow direct visualisation of the vessel wall when this contains thrombus in a false lumen. Pathognomic findings of a carotid artery dissection are (1) double lumen and (2) intimal flap. These are, however, detected in less than 10% of cases [45], and the following three angiographic patterns are found more commonly (Fig. 1) [45, 46]: (1) arterial stenosis, (2) aneurysm formation and (3) arterial occlusion.
a Selective right common carotid artery (CCA) arteriography in a patient with a traumatic internal carotid artery (ICA) dissection, demonstrating a tapered narrowed “true” lumen (black arrow) compressed by thrombus in the “false” lumen, with “rat’s tail” or “string sign”. CCA large black arrow, external carotid artery (ECA) white arrow. b A tapered narrowing (black arrow) in a patient with a spontaneous ICA dissection. CCA large black arrow, ECA white arrow). c Irregular stenosis (arrow) associated with dissection of the intracranial extradural segment of the ICA. (Courtesy of Dr. S. Connor, King’s College Hospital, London)
The most common finding, reported in almost 80% cases, is an irregular stenosis starting about 2–3 cm distal to the carotid bulb and extending for various lengths along the artery [16, 25, 45, 46]. Complete occlusion or aneurysm formation is seen less often. A tapered narrowing of the ICA (“rat’s tail” or “string sign”), a flame-shaped occlusion and aneurysms commonly affecting the distal cervical segment are also seen. Although these appearances are indicative of dissection, they are not specific [20, 47–49]. Dissection is a dynamic disease process, and serial angiography demonstrates changing patterns in the lumen, often returning to a normal calibre over time. In one series of 42 patients with spontaneous dissection of the extracranial ICA, 59% of cases had a tapered stenosis [45], progression to complete occlusion was reported in 14% of stenotic dissections, 50% of aneurysms reduced in size, 25% remained unchanged and 25% of those with an isolated aneurysm demonstrated complete resolution over a mean time of 11 months.
The angiographic appearances of VA dissections are less specific than those of ICA dissection and include dissecting aneurysms of the intradural portion (Fig. 2). In up to 20% of patients with spontaneous VA dissection, four-vessel angiography reveals concurrent dissection of the ICA or contralateral VA [50]. Follow-up angiographic studies show resolution of VA abnormalities in 70% of cases [20, 31]. Aneurysmal forms of cervical VA dissection were found to resolve in 80% of cases, more frequently than aneurysmal ICA dissections [51].
a Selective left vertebral artery (VA) angiogram demonstrates a dissecting aneurysm of the VA (arrow) close to the origin of the left posterior inferior cerebellar artery (PICA). b Endovascular treatment of the aneurysm with stenting of the intradural segment of the left VA and coiling of the PICA aneurysm. The mesh of the intracranial stent is not radio-opaque, but markers at either end of the stent are visible (open arrows). A ball of platinum coils fills the lumen of the aneurysm (arrow). c An oblique projection demonstrates preservation of the left PICA (arrow) and exclusion of the aneurysm at the end of the endovascular procedure. (Courtesy of Dr. Stefan Brew, The National Hospital for Neurology and Neurosurgery, London)
Ultrasound
Serial imaging of ICA and VA dissections is required for the detection of possible recanalisation or progression to occlusion [52]. This should be preferably performed with noninvasive modalities. Ultrasound imaging provides direct visualisation of the pathological findings related to an ICA dissection, haemodynamic information, a visual picture of flow velocity, direction of flow within the true and false lumen and evaluates vessel and lumen patency [53, 54]. Unlike angiography, US is able to demonstrate a false lumen even if this lumen is thrombosed [55, 56]. The gray-scale US findings can be divided into three categories;
-
Normal: dissection is outside the “window” of the US examination, or resolution of the dissection has occurred at the time of the examination
-
Presence of an arterial luminal flap or false lumen (Fig. 3)
-
Presence of low-reflective thrombus with or without true lumen narrowing (Fig. 4)
The pathognomonic finding is the demonstration of a membrane in the longitudinal and axial view [57]. Spectral Doppler US waveforms can be divided into four categories:
-
Normal spectral waveform
-
Damped spectral waveform (lower amplitude with biphasic pattern)
-
High-resistance spectral waveform (Fig. 5)
-
Absence of flow with no spectral Doppler waveform (Fig. 6)
a Colour and spectral Doppler ultrasound (US) of the internal carotid artery (ICA) in a dissection (arrow) demonstrating a high-resistance waveform. b Colour and spectral Doppler US demonstrating an occluded ICA (large arrow) following a dissection. The spectral Doppler US waveform in the external carotid artery (ECA) (arrow) demonstrates a lower-resistance spectral Doppler waveform pattern than normal; this is a compensatory mechanism in long-standing ICA occlusion
a Colour Doppler ultrasound (US) demonstrates absence of flow in the vertebral artery (VA) (thick arrow) following a dissection. Vertebral vein thin arrow, transverse process star. b The absence of a spectral Doppler US waveform in the VA (arrow) in the same patient confirms an occlusion. Vertebral vein arrow, transverse process star
Although these are nonspecific features also occurring in high-grade stenosis and occlusions, they should raise the possibility of a dissection in the appropriate clinical setting. The commonest spectral Doppler US findings in the affected ICA are high resistance pattern or absence of signal in a total occlusion [52, 53]. Visualisation of intramural haematoma combined with high-resistance flow strongly suggests the presence of ICA dissection. Steinke et al, found high-resistance flow in 68% of ICA dissections examined with US [52]. The diagnostic sensitivity of US decreased if an ICA dissection resulted in a low-grade stenosis. Sturzenegger et al. demonstrated high accuracy in detecting a dissection with US when an ICA occlusion or high-grade stenosis was present, falling to a 20% sensitivity in low-grade stenosis [57]. As indicated, US is less reliable for dissections located in the subpetrous segment and the carotid canal [58, 59]. A VA dissection (Fig. 7) is difficult to ascertain on colour Doppler US due to the nature of the position of the VA (between the transverse processes of the cervical vertebrae), and full interrogation is not possible. The same US features are seen as with an ICA dissection, but it is less likely to be clearly demonstrated [60].
a Longitudinal colour Doppler ultrasound (US) image of the vertebral artery (VA) (arrow) demonstrating thrombus within the artery (large arrow). Transverse process star. b Spectral Doppler US waveform of the right VA (arrow) in the same patient demonstrating a high-resistance waveform, with absent forward flow in diastole (large arrow). (c The normal left VA in the same patient for comparison, demonstrating a low-resistance, high forward flow in diastole (large arrow)
As an ICA or VA dissection is not a stable condition, serial monitoring is required. US is an excellent imaging technique for this when the dissection is clearly documented on initial US imaging. Temporal resolution or progression of a dissection may be documented, allowing alteration of medical management, as appropriate (Fig. 8).
a Longitudinal colour Doppler ultrasound (US) image of an acute dissection of the internal carotid artery (ICA) with the dissection of the lumen (arrowhead) demonstrating colour flow. ICA large arrow, external carotid artery (ECA) long arrow. b An abnormal high-resistance spectral Doppler US waveform is demonstrated in the dissection lumen (arrowhead). ICA large arrow, ECA long arrow. c. On day 14, there is intramural thrombus formation (arrowhead) with no evidence of colour Doppler US flow within the dissection false lumen. CCA star, ICA large arrow, ECA long arrow
Magnetic resonance imaging
Dissections of the craniocervical arteries can be assessed with cross-sectional T1-, T2- or proton-density (PD)-weighted images and with MR angiographic (MRA) techniques. The former can provide direct visualisation of an intramural haematoma, which is the pathological hallmark of a dissection [59, 61], and the latter allows noninvasive visualisation of blood vessels. Time-of-flight (TOF) MRA can also demonstrate a T1 hyperintense intramural clot whereas phase-contrast MRA (PC-MRA) and contrast-enhanced MRA (CE-MRA) demonstrate only the vessel lumen.
Carotid artery
Carotid artery dissection is characterised by a narrowed eccentric flow void, which is surrounded by a crescent-shaped, hyperintense area expanding the vessel diameter [62]. The intramural haematoma shows a similar temporal evolution of its MR signal as an intracerebral haemorrhage [61]. An acute intramural haematoma can be hypointense on T2- and T1-weigthed images and therefore difficult to delineate from an area of flow void. The intramural haematoma may therefore be missed on MRI within the first 24–48 h after an ICA dissection. Thereafter, the haematoma becomes of intermediate signal intensity on T1-weighted images and hyperintense on PD and T2-weighted images (Fig. 9). After a few days, the haematoma will also demonstrate high signal intensity on T1-weighted images for approximately 2 months (Fig. 10). Subsequent loss of signal intensity can make the haematoma unrecognisable after 6 months [63], as it becomes isointense with surrounding soft tissue [64]. These appearances are, however, not specific for a dissection and fresh thrombus due to an atheromatous or embolic occlusion, which may exhibit a similar evolution of MR signal intensity [65]. It may, indeed, be impossible to distinguish an intraluminal clot from an intramural clot, which causes complete obliteration of the vessel lumen. In such cases, a crescentric thickening with central signal void proximal to complete occlusion should suggest dissection rather than atheromatous occlusion [29, 66].
a Traumatic dissection of the right internal carotid artery (ICA) in a “pole” dancer. The axial proton-density-weighted images through the neck show a mural haematoma (arrow) at the lateral aspect of the right ICA. The right ICA is expanded, and its true lumen is not significantly narrowed (open arrow). b Axial diffusion-weighted imaging (DWI) shows an acute infarct in the right lentiform nucleus as a result of the dissection
Early reports described an atheromatous plaque causing subtotal occlusion appearing as a hyperintense rim on T2-weighted images, thereby mimicking a dissection [67, 68]. This rim is, however, typically isointense on T1-weighted images whereas the periarterial rim in subacute cervicocephalic arterial dissection is usually hyperintense on T1-weighted images [69]. A false positive diagnosis may also originate from misinterpretation of T1 hyperintense fat around the vessel, which can mimic an intramural haematoma; fat-suppression techniques are useful in such cases (see Fig. 10). Inflow phenomena, in the presence of slow blood flow, can be a further confounding factor. Inflow phenomena generally produce signal abnormalities that are located centrally within the flow void rather than peripherally [58, 70]. Homogeneity of the hyperintense signal on all slices associated with vessel expansion supports dissection rather than slow flow [59].
A false negative diagnosis of dissection on MR is most likely at the very early stage, when the intramural haematoma is not yet hyperintense. Vessel wall thickening and lumen narrowing may be the only indicators of dissection at this stage [63, 71], and an increase in external diameter seems to be the most sensitive sign of early ICA dissection [29, 69].
The mural haematoma can also be demonstrated on TOF-MRA, as this technique does not completely suppress stationary tissue with short T1 values (Fig. 11) [28]. In cases of a suspected dissection, it is important to review maximum intensity projections (MIP) as well as source data of TOF-MRA. Flow within the vascular lumen usually produces a more intense signal than the mural haematoma. This difference is most apparent on source data (see Fig. 11a) [62]. Inspection of source data allows assessment of the full vessel circumference, but longitudinal extent and precise location of the dissection is better appreciated on MIP images. T1 hyperintense signal form mural haematoma in the methaemoglobin stage may also map into MIP images and simulate an enlarged vascular segment (see Fig. 11b). Levy et al. described an increase in vessel external diameter in 18 out of 19 (95%) cases on TOF-MRA and found this to be the most sensitive feature of a dissection [29].
a Source image of \two-dimensional (2D) time-of-flight magnetic resonance imaging (TOF-MRA) through the level of the C1 vertebral body in a patient with bilateral internal carotid artery (ICA) dissections. A mural haematoma surrounds the right ICA (open arrow) and appears less bright than the flow signal. On the left side, both true and false lumens (arrows) are visible, separated by a less-T1-hyperintense haematoma. b Targeted maximum intensity projection (MIP) of the left ICA shows an expansion of its high cervical segment (arrow). This appearance is due to combined projection of the true lumen, false lumen and intervening haematoma, which are less easily separated than on the source image. c On the source image of a follow-up MR image 6 weeks later. the mural haematomas are no longer visible, but there is a persistent double lumen of the left ICA (arrows). d Targeted MIP of a three-dimensional (3D) phase-contrast MRA elegantly demonstrates flow in the persistent false lumen at the dissection site (arrow)
There are some important pitfalls in the TOF imaging of ICA dissections. In some cases, the intramural thrombus may not be detected because the high signal clot simulates flowing blood on MIP images. This phenomenon is important in the petrous segment of the ICA where no widening of the vessel can be detected and where a short-segment stenotic dissection can be missed [64]. On the other hand, MIP images of TOF-MRA are frequently hampered by susceptibility artefact at the skull base, which can give an irregular appearance to the proximal petrous segment of the ICA and may wrongly suggest the presence of a dissection, particularly if the appearances are asymmetrical. Three-dimensional (3D) or multiple overlying slices acquisition (MOTSA) are usually preferred for TOF imaging. In the presence of very severe luminal compromise with extremely slow flow, a two-dimensional (2D) TOF sequence may be more helpful to demonstrate residual lumen.
PC-MRA and CE-MRA are both luminal imaging techniques and do not allow direct visualisation of the arterial wall and intramural haematoma. PC-MRA requires the selection of appropriate velocity encoding (VENC), which is the order of 50 cm/s for arterial flow. PC-MRA is less frequently used than CE-MRA, which is rapidly becoming the MRA technique of choice with recent improvements in MR gradients and software, which allow rapid acquisitions with centric k-space filling and automatic bolus triggering. Like conventional intraarterial angiography, CE-MRA can demonstrate luminal irregularity, change of vessel calibre or occlusion (Fig. 12) and pseudoaneurysm formation (Fig. 13). The spatial and temporal resolution of CE-MRA is inferior to conventional angiography but is noninvasive. CE-MRA also has the advantage that it can be easily supplemented with T2- and T1-weighted axial images through narrowed segments to confirm or refute a suspected dissection and demonstrate associated brain lesions (see Figs. 9 and 12).
a Anteroposterior projection of a contrast-enhanced magnetic resonance angiogram (CE-MRA) showing a tapered narrowing of the left internal carotid artery (ICA) (white arrow) from the bifurcation to its intracranial portion. The right ICA (open arrow) and basilar artery (arrowhead) are of normal calibre. The left middle cerebral artery does not fill with contrast. b Axial T2-weighted image through the upper neck shows a mural haematoma surrounding the narrowed lumen of the left ICA (arrow) compared with a normal flow void in the right ICA (open arrow). c Axial T2-weighted image at the level of the horizontal (petrous) portion of the ICAs. The left ICA shows “tram-lining” ( arrow), with a peripheral mural thrombus and reduced flow centrally, which does not produce a flow void, as is seen in the petrous portion of the right ICA (open arrow). Without the findings on the CE-MRA (a), there is uncertainty as to the patency of the left ICA at this level. d Axial T2* weighted intracranial MR image show susceptibility artefact from a clot obstructing the M1 segment of the left middle cerebral artery. The acute clot is of low signal intensity (arrow). e Axial diffusion-weighted (DW) MR image demonstrates an acute striatocapsular infarct involving the left caudate and lentiform nuclei
a Axial T2-wieghted magnetic resonance image (MRI) in a patient with a traumatic right internal carotid artery (ICA) dissection shows an intramural haematoma (arrow) at the posteromedial aspect of the right ICA, which has a narrowed lumen at this stage. b Targeted maximum intensity projection (MIP) of a contrast-enhanced MR angiogram (CE-MRA) shows that the right ICA has recanalised, but a pseudoaneurysm has formed at the site of the previous intramural haematoma (arrow)
MRA can also be combined with advanced MRI methods to demonstrate physiological repercussions of a dissection. Acute ischaemic lesions are best shown on diffusion-weighted imaging (DWI) (see Figs. 9b and 12e), and areas of haemodynamic compromise can be detected with perfusion-weighted imaging (PWI). The combination of cross-sectional MRI and MRA is not only a powerful diagnostic modality but can also be used effectively for noninvasive follow up of ICA dissections [72–74] to monitor resolution of an intramural haematoma or development of complications (see Figs. 11 and 13).
Vertebral artery
MRI and MRA are less sensitive and specific for the diagnosis of VA dissections due to the smaller diameter of the normal VAs and the broad physiological variations in vessel calibre [75]. Dissection of the cervical (V2) segment may be difficult to diagnose, as the arterial lumen is often asymmetrical in normal subjects, and often the artery is surrounded by a small amount of fat, which is of high signal intensity on T1-weighted images and therefore may mimic a subacute haematoma [76]. Inflow enhancement phenomena from the venous plexus in the transverse foramina may also mimic a mural haematoma on axial images (Fig. 14). CE-MRA may show irregularities and change in calibre of VAs at the site of dissection (Fig. 15). Given the present spatial resolution of CE-MRA, these changes are more difficult to interpret in a small, nondominant VA, and one has to beware of a false positive diagnosis. CE-MRA has shown to be promising in the follow-up of VA dissections and was able to accurately detect vessel recanalisation, progression to occlusion and persistence or resolution of a pseudoaneurysm [77].
a Axial fat-saturated T2-weighted image at the level of the C1 vertebral body. Bilateral, crescent-shaped, hyperintense areas are seen in the C1 transverse foramina around the posterolateral aspects of both vertebral arteries (VAs) (white arrows). These are due to slow blood flow in periarterial venous plexus and may simulate bilateral VA dissections. b Frontal projection of a two-dimensional (2D) phase-contrast magnetic resonance angiogram (MRA) shows normal VAs bilaterally (arrows)
a Contrast-enhanced magnetic resonance angiogram (CE-MRA) in a patient with a dissection of the intradural portion of the left vertebral artery, which has an irregular calibre (arrow). b Axial T2-weighted magnetic resonance (MR) image in the same patient shows a T2 hyperintense area in the left anterior aspect of the medulla oblongata, in keeping with a medullary infarct (arrowhead)
Computed tomography angiography
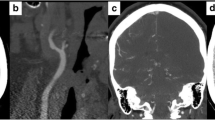
Multisection CT angiography (CTA) provides high-resolution and high-contrast images of the arterial lumen and vessel wall and is noninvasive. Axial source images provide excellent visualisation of the craniocervical arteries as a consequence of the contrast difference between the enhanced arterial lumen and the surrounding structures. Postprocessing of the source data as MIPs or curved multiplanar reformats MPR produces images that closely resemble those obtained with intraarterial angiography, and voxel-rendering techniques allow a 3D display of the vessels and surrounding soft tissues [78]. CTA of ICA dissections has shown excellent agreement with arterial angiography [79]. A 100% sensitivity and specificity was achieved using the presence of a narrowed eccentric lumen in association with enlargement of the overall vessel diameter as criterion for acute carotid dissection. Other signs of extracranial carotid artery dissection on CT include stenosis, mural thickening, occlusion, aneurysm formation and thin annular contrast enhancement (Fig. 16).
Multisection CTA has also proved useful for diagnosis of VA dissections [80]. Multisection CT achieved 100% sensitivity for detecting stenosis and occlusive and aneurysmal dissections of the VA in 17 patients. There was one misclassification of a severe atherosclerotic lesion as aneurysmal dissection, resulting in a sensitivity of 98%. CTA is also suitable for noninvasive follow-up of patients with extracranial carotid artery or VA dissections. MRI may be better for evaluation of arterial segments near the skull base, as artefacts in this region can hamper CT.
Treatment
The aim of treatment is to prevent development of neurological deficits or worsening existing ones. This can be achieved by preventing thrombosis, distal embolisation and restoring compromised blood flow if the symptoms are haemodynamic in origin. Treatment is, however, controversial, and controlled clinical trials are lacking [50]. Early anticoagulation may decrease the risk of distal embolisation from or thrombosis of the ICA or VA [81, 82]. The most frequent medical therapy is intravenous heparin for 1 week, followed by warfarin or aspirin for 3–6 months [50]. In cases of residual pseudoaneurysm, persisting severe stenosis or an underlying arteriopathy, long-term aspirin should be considered [83]. Thrombolytic therapy, both intravenous and intraarterial, has been successfully used in acute dissection without significant complications or evidence of lesion extension [84]. Early anticoagulation is recommended in extracranial VA dissection to reduce the risk of posterior circulation infarction. In intracranial VA and ICA dissection, anticoagulants are contraindicated because of the risk of subarachnoid haemorrhage. Anticoagulation is also contraindicated in patients with a pseudoaneurysm because of the risk of pseudoaneurysm rupture [24].
Surgical intervention is often difficult, as the typical location of the dissection is distal to the surgical field. Various surgical methods have been employed in the treatment of ICA dissections, including ICA ligation or clipping, thromboendarterectomy and “patch” angioplasty as well as extracranial to intracranial bypass procedures [40, 85, 86]. More recently, endovascular metallic stent insertion has been used in patients who have recurrent thromboembolic events [87]. In cases of a persistent pseudoaneurysm, coil embolisation may be performed [88–90]. Covered endovascular stents have also been used to treat symptomatic ICA-dissecting pseudoaneurysm [91–93]. A recent report describes the placement of a coronary stent graft to occlude a dissecting pseudoaneurysm of the extracranial ICA in a patient with a progressively enlarging pseudoaneurysm [91]. This led to resolution of clinical symptoms and radiologic restoration of normal blood flow. There have also been several other case reports showing a high technical success rate of stent grafts in the extracranial portion of the ICA [93, 94]. Although there are reports of complete stent-graft patency after a follow-up period ranging between 14 months and 4 years [92, 93], there is generally a paucity of data on long-term follow-up.
Intradural VA dissections, especially when complicated by dissecting aneurysms, need to be managed more aggressively because of a high risk of a subarachnoid haemorrhage and high rebleeding rates [95]. Endovascular treatment is increasingly replacing surgical treatment and includes proximal occlusion, aneurysm trapping, coil embolisation or stenting (see Fig. 2b and c) [96]. This has a high technical success rate but can be associated with an up to 20% mortality, which compares favourably with the natural history of these lesions [37].
Prognosis
The reported death rate from dissections of carotid and VAs is less than 5%, and about three fourths of patients who have a stroke make a good functional recovery [16, 25, 26, 81]. The risk of recurrent dissection in an initially unaffected artery is about 2% during the first month but then decreases to a rate of only about 1% per year [26]. However, the increased risk persists for at least a decade and possibly longer [97, 98]. Dissections of the intradural VA have a worse prognosis, with a mortality rate of up to 50% in untreated cases [37].
Recommendation for imaging of carotid and vertebral artery dissections
Carotid dissections
The initial diagnosis should be made with a technique able to visualise the vessel wall (to confirm the presence of a mural haematoma) as well as the vessel lumen (to provide evidence of vascular narrowing or occlusion). Additional imaging of the brain parenchyma is helpful to document associated ischaemic events. This can be achieved by a combination of MRI and MRA or by CT and CTA. In our institution, we prefer MRI and MRA because of the superior soft tissue contrast and higher sensitivity of DW MRI to demonstrate acute ischaemic complications. Fat-saturated axial T2- or T1-weighted images through the neck are best suited to show the mural haematoma, and CE-MRA of the neck vessel provides a more accurate definition of the lumen than TOF-MRA. The latter can, however, provide simultaneous visualisation of the vessel lumen and mural haematoma. Axial CT or source data of the CTA have a theoretical advantage in the very acute phase when the mural haematoma is still hypointense on MRI.
After making the diagnosis of a dissection by MRI and MRA or by CT and CTA, we normally perform an US examination. This forms the baseline for follow-up US studies to document recanalisation, stabilisation or progressive vascular occlusion. Follow-up of luminal restoration or compromise by US is more accessible and cost effective and can be performed more frequently than follow-up with MRA and CTA (which adds to ionising radiation exposure). Follow-up luminal imaging by MRA or CTA (preferably CE-MRA) is indicated if the dissection lies outside or extends outside the US field of view. Invasive angiography should be reserved for the rare cases that present with diagnostic difficulty and that cannot be resolved by any noninvasive technique, as well as an adjunct to endovascular treatment of unstable dissections with progressive neurology.
Vertebral artery dissections
VA dissection represents a greater diagnostic challenge. The initial diagnosis is again best made with a combination of mural and luminal imaging, such as MRI and MRA or by CT and CTA. Particular awareness of artefacts from periarterial venous plexus on MRI is required. CE-MRA is superior to TOF-MRA, which frequently shows a signal dropout in the horizontal portions of the VAs around C1. The role of US in VA dissection is limited to documenting vessel patency or occlusion. Arterial angiography in VA dissection is particularly indicated for complications of intracranial segment dissections, such as pseudoaneurysm formation, as these require early endovascular treatment. Luminal imaging for follow-up of VA dissections is best done with CE-MRA or CTA.
References
Ducrocq X, Lacour JC, Debouverie M, Bracard S, Girard F, Weber M (1999) Accidents vasculaires cerebraux ischemiques du sujet jeune: etude prospective de 296 patients ages de 16 a 45 ans. Rev Neurol (Paris) 155:575–582
Hart RG, Easton JD (1985) Dissections. Stroke 16:925–927
Lucas C, Moulin T, Deplanque D, Tatu L, Chavot D (1998) Stroke patterns of internal carotid artery dissection in 40 patients. Stroke 29:2646–2648
Bogousslavsky J, Regli F (1987) Ischemic stroke in adults younger than 30 years of age: cause and prognosis. Arch Neurol 44:479–482
Jentzer A (1954) Dissecting aneurysm of the left internal carotid artery. Angiology 5:232–234
Provenzale JM, Barboriak DP, Taveras JM (1995) Exercise-related dissection of craniocervical arteries: CT, MR and angiographic findings. J Comput Assit Tomogr 19:268–276
Mokri B (1990) Traumatic and spontaneous extracranial internal carotid artery dissections. J Neurol 237:356–361
Biller J, Hingtgen WL, Adams HP, Smoker WRK, Godersky JC, Toffol GJ (1986) Cervicocephalic arterial dissections. A ten-year experience. Arch Neurol 43:1234–1238
Luken MG, Ascherl GF, Correll JW, Hilal SK (1975) Spontaneous dissections of the extracranial internal carotid artery. Clin Neurosurg 26:353–357
Descamps MJ, Lewis MJ, Hart PE, Brew S, Jager HR, Greenwood R (2004) Brainstem infarction during long-haul air travel. Eur Neurol 52:181–184
Nadgir RN, Loevner LA, Ahmed T, Moonis G, Chalela J, Slawek K et al (2003) Simultaneous bilateral internal carotid and vertebral artery dissection following chiropractic manipulation: case report and review of the literature. Neuroradiol 45:311–314
Mas JL, Bousser MG, Hasboun D, Laplane D (1987) Extracranial vertebral artery dissection. A review of 13 cases. Stroke 18:889–903
Schievink WI, Michels VV, Piepgras DG (1994) Neurovascular manifestations of heritable connective tissue disorders: a review. Stroke 25:889–903
Schievink WI, Bjornsson J, Piepgras DG (1994) Coexistance of fibromuscular dysplasia and cystic medial necrosis in a patient with Marfan’s syndrome and bilateral carotid artery dissections. Stroke 25:2492–2496
Karacagil S, Hardemark HG, Bergovist D (1996) Spontaneous internal carotid artery dissection. Int Angiol 15:291–294
Mokri B, Sundt TH, Houser OW, Piepgras DG (1986) Spontaneous dissection of the cervical internal carotid artery. Ann Neurol 19:126–138
Ast G, Woimant F, Georges B, Laurian C, Haguenau M (1993) Spontaneous dissection of the internal carotid artery in 68 patients. Eur J Med 2:466–472
Provenzale JM, Morgenlander JC, Georges B, Laurian C, Haguenau M (1996) Spontaneous vertebral dissection: clinical, conventional angiographic, CT, and MR findings. J Comput Assit Tomogr 20:185–193
Chiras J, Marciano S, Molina J, Touboul J, Poirier B, Bories J (1985) Spontaneous dissecting aneurysm of the extracranial vertebral artery (20 cases). Neuroradiol 27:327–333
Mokri B, Houser OW, Sandok BA (1988) Spontaneous dissections of the vertebral arteries. Neurology 38:880–885
Sturzenegger M (1994) Headache and neck pain: the warning symptoms of vertebral artery dissection. Headache 34:187–193
Biousse V, D’Anglejan-Chatillon J, Massiou H, Bousser MG (1994) Head pain in nontraumatic carotid artery dissection: a series of 65 patients. Cephalgia 14:33–36
Davies MJ, Treasure T, Richardson PD (1996) The pathogenesis of spontaneous arterial dissection. Heart 75:434–435
Anson J, Crowell RM (1991) Cervicocranial arterial dissection. Neurosurg 29:89–96
Fisher CM, Ojemann RG, Roberson GH (1978) Spontaneous dissection of cervico-cerebral arteries. Can J Neurol Sci 5:9–19
Schievink WI, Mokri B, O’Fallon WM (1994) Recurrent spontaneous cervical-artery dissection. N Engl J Med 330:393–397
Vilela P, Goulao A (2005) Ischemic stroke: carotid and vertebral artery disease. Eur Radiol 15:427–433
Wityk RJ (2001) Stroke in a healthy 46-year-old man. JAMA 285:2757–2762
Levy C, Laissy JP, Raveau V, Amarenco P, Servois V, Bousser MG et al (1994) Carotid and vertebral artery dissections: three-dimensional time-of-flight MR angiography and MR imaging versus conventional angiography. Radiology 190:97–103
Caplan LP, Zarins CK, Hemmati M (1985) Spontaneous dissection of the extracranial vertebral arteries. Stroke 16:1030–1038
Hinse P, Thie A, Lachenmayer L (1991) Dissection of the extracranial vertebral artery: a report of four cases and a review of the literature. J Neurol Neurosurg Psychiatry 54:863–869
Mokri B, Silbert PL, Schievink WI, Piepgras DG (1996) Cranial nerve palsy in spontaneous dissection of the extracranial internal carotid artery. Neurology 46:356–359
Gobert M, Mounier-Vehier F, Lucas C, Leclerc X, Leys D (1996) Cranial nerve palsies due to internal carotid artery dissection: seven cases. Acta Neurol Belg 96:55–61
Schievink WI, Mokri B, Piepgras DG (1994) Spontaneous dissections of the cervicocephalic arteries in childhood and adolescence. Neurology 44:1607–1612
Caplan LR, Baquis GD, Pessin MS, D’Alton J, Adelman LS, DeWitt LD et al (1988) Dissection of the intracranial vertebral artery. Neurology 38:868–877
Ramgren B, Cronqvist M, Romner B, Brandt L, Holtas S, Larsson EM (2005) Vertebrobasilar dissection with subarachnoid hemorrhage: a retrospective study of 29 patients. Neuroradiol 47:158–164
Rabinov J, Hellinger F, Morris P, Ogilvy C, Putman C (2003) Endovascular management of vertebrobasilar dissecting aneurysms. AJNR Am J Neuroradiol 24:1421–1428
Sandmann W, Hennerici M, Aulich A, Kniemeyer H, Kremer KW (1984) Progress in carotid artery surgery at the base of the skull. J Vasc Surg 1:734–743
Schievink WI, Mokri B, Whisnant JP (1993) Internal carotid artery dissection in a community. Rochester. Minnesota. 1987–1992. Stroke 24:1678–1680
Treiman GS, Treiman RL, Foran RF, Levin PM, Cohen JL, Wagner WH et al (1996) Spontaneous dissection of the internal carotid artery: a nineteen-year clinical experience. J Vasc Surg 24:597–605
Hirai T, Korogi Y, Ikushima I, Shigematsu Y, Morishita S, Yamashita Y (2003) Intracranial artery dissections: serial evaluation with MR imaging, MR angiography, and source images of MR angiography. Radiat Med 21:86–93
Grzyska U, Freitag mJ, Zeumer H (1990) Selective cerebral intraarterial DSA. Complication rate and control of risk factors. Neuroradiol 32:296–299
Roome NS, Aberfeld DC (1977) Spontaneous dissecting aneurysm of the internal carotid artery. Arch Neurol 34:251–252
Weinberger J (1981) Doppler pulse waveform analysis of carotid artery flow in dissecting aortic aneurysm. Arch Neurol 38:256–257
Houser OW, Mokri B, Sundt TM, Baker HL, Reese DF (1984) Spontaneous cervical cephalic arterial dissection and its residuum: angiographic spectrum. AJNR Am J Neuroradiol 5:27–34
Hart RG, Easton JD (1983) Dissections of cervical and cerebral arteries. Neurol Clin 1:155–182
Pelkonen O, Tikkakoski T, Leinonen S, Pyhtinen J, Lepojarvi M, Sotaniemi K (2003) Extracranial internal carotid and vertebral artery dissections: angiographic spectrum, course and prognosis. Neuroradiology 45:71–77
Friedman DP, Flanders AE (1992) Unusual dissection of the proximal vertebral artery: description of 3 cases. AJNR Am J Neuroradiol 13:283–286
Simeone FA, Goldberg HI (1968) Thrombosis of the vertebral artery from hyperextension injury to the neck. J Neurosurg 29:540–543
Schievink WI (2000) The treatment of spontaneous carotid and vertebral artery dissections. Curr Opin Cardiol 15:316–321
Touze E, Randoux B, Meary E, Arquizan C, Meder JF, Mas JL (2001) Aneurysmal forms of cervical artery dissection. Associated factors and outcome. Stroke 32:418–423
Steinke W, Rautenberg W, Schwartz A, Hennerici M (1994) Noninvasive monitoring of internal carotid artery dissection. Stroke 25:998–1005
Logason K, Hardemark HG, Barlin T, Bergqvist D, Ahlstom H, Karacagil S (2002) Duplex scan findings in patients with spontaneous cervical artery dissections. Eur J Vasc Endovasc Surg 23:295–298
Bluth EI, Shyn PB, Sullivan M, Merritt CR (1989) Doppler color flow imaging of carotid artery dissection. J Ultrasound Med 8:149–153
Sidhu PS, Jonker ND, Khaw KT, Patel N, Blomley MJK, Ray-Chaudhuri K et al (1997) Spontaneous dissections of the internal carotid artery: appearances on color Doppler ultrasound. Br J Radiol 70:50–57
Gardner DJ, Gosink BB, Kallman CE (1991) Internal carotid artery dissections: duplex ultrasound imaging. J Ultrasound Med 10:607–614
Sturzenegger M, Mattle HP, Rivoir A, Baumgartner RW (1995) Ultrasound findings in carotid artery dissection: analysis of 43 patients. Neurology 45:691–698
Waluch V, Bradley WG (1984) NMR even echo rephasing in slow laminar flow. J Comput Assit Tomogr 8:594–598
Aggarwal S, Kucharczyk W, Keller MA (1999) Asymptomatic postendarterectomy dissection of the internal carotid artery detected incidentally on MRI. Neuroradiol 35:586–587
Sturzenegger M, Mattle HP, Rivoir A, Rihs F, Schmid C (1993) Ultrasound findings in spontaneous extracranial vertebral artery dissection. Stroke 24:1910–1921
Goldberg HI, Grossman RI, Gomori JM, Asbury AK, Bilaniuk LT, Zimmerman RA (1986) Cervical internal carotid artery dissecting hemorrhage: diagnosis using MR. Radiology 158:157–161
Stringaris K, Liberopoulos K, Giaka E, Kokkinis K, Bastounis E, Klonaris EC et al (1996) Three-dimensional time-of-flight MR angiography and MR imaging versus conventional angiography in carotid artery dissections. Int Angiol 15:20–25
Kitanaka C, Tanaka J, Kuwahara M, Teraoka A (1994) Magnetic resonance imaging study of intracranial vertebrobasilar artery dissections. Stroke 25:571–575
Kirsch E, Kaim A, Engelter S, Lyrer P, Stock KW, Bongartz G et al (1998) MR angiography in internal carotid artery dissection: improvement of diagnosis by selective demonstration of the intraluminal haematoma. Neuroradiology 40:704–709
Schwaighofer B, Klein MV, Lyden PD, Hesselink JR (1990) MR imaging of vertebrobasilar vascular disease. J Comput Assit Tomogr 14:895–904
Zuber M, Meary E, Meder JF, Mas JL (1994) Magnetic resonance imaging and dynamic CT scan in cervical dissections. Stroke 25:576–581
Heinz ER, Yeates AE, Djang WT (1989) Significant extracranial carotid stenosis: detection on routine cerebral MR images. Radiology 170:843–848
Katz BH, Quencer RM, Kaplan JO, Hinks RS, Post MJ (1989) MR imaging of intracranial carotid occlusion. AJR Am J Roentgenol 152:1271–1276
Provenzale JM (1995) Dissection of the internal carotid and vertebral arteries: imaging features. AJR Am J Roentgenol 165:1099–1104
Gelbert F, Assouline E, Hodes JE, Reizine D, Woimant F, George B et al (1991) MRI in spontaneous dissection of vertebral and carotid arteries. 15 cases studied at 0.5 tesla. Neuroradiol 33:111–113
Ozdoba C, Sturzenegger MN, Schroth G (1996) Internal carotid artery dissection. MR imaging features and clinical-radiologic correlation. Radiology 199:191–198
Grolimund P, Seller RW, Aaslid R, Huber P, Zurbruegg H (1987) Evaluation of cerebrovascular disease by combined extracranial and transcranial Doppler sonography. Experience in 1,039 patients. Stroke 18:1018–1024
Middleton WD, Foley WD, Lawson TL (1988) Color-flow Doppler imaging of carotid artery abnormalities. AJR Am J Roentgenol 150:419–425
Sipponen JT, Sepponen RE, Sivula A (1983) Nuclear magnetic resonance (NMR) imaging of intracerebral hemorrhage in the acute and resolving phases. J Comput Assit Tomogr 7:954–960
Tay KY, U-King-Im JM, Trivedi RA, Higgins NJ, Cross JR, Weissberg PL et al (2005) Imaging the vertebral artery. Eur Radiol 15:1329–1343
George B, Laurian C (1987) The vertebral artery. Pathology and surgery. Springer Verlag, Vienna
Leclerc X, Lucas C, Godefroy O, Nicol L, Moretti A, Leys D et al (1999) Preliminary experience using contrast-enhanced MR angiography to assess vertebral artery structure for the follow-up of suspected dissection. AJNR Am J Neuroradiol 20:1482–1490
Schuknecht B (2004) Latest techniques in head and neck CT angiography. Neuroradiol 46:s208–s213
Leclerc X, Godefroy O, Salhi A, Lucas C, Leys D, Pruvo JP (1996) Helical CT for the diagnosis of extracranial internal carotid artery dissection. Stroke 27:461–466
Chen CJ, Tseng YC, Lee TH, Hsu HL, See LC (2004) Multisection CT angiography compared with catheter angiography in diagnosing vertebral artery dissection. AJNR Am J Neuroradiol 25:769–774
Biousse V, D’Anglejan-Chatillon J, Touboul PJ, Amarenco P, Bousser MG (1995) Time course of symptoms in extracranial carotid artery dissections. A series of 80 patients. Stroke 26:235–239
Srinivasan J, Newell DW, Sturzenegger M, Mayberg MR, Winn HR (1996) Transcranial Doppler in the evaluation of internal carotid artery dissection. Stroke 27:1226–1230
Leys D, Lucas C, Gobert M, Deklunder G, Pruvo JP (1997) Cervical artery dissections. Eur Neurol 37:3–12
Arnold M, Nedeltchev K, Sturzenegger M, Schroth G, Loher TJ (2002) Thrombolysis in patients with acute stroke caused by cervical artery dissection: analysis of 9 patients and review of the literature. Arch Neurol 59:549–553
Coffin O, Maiza D, Galateau-Salle F, Martel B, Vignon C, Neri E et al (2004) Results of surgical management of internal carotid artery aneurysm by the cervical approach. Ann Vasc Surg 24:597–605
Muller BT, Luther B, Hort W, Neumann-Haefelin T, Aulich A, Sandmann W (2000) Surgical treatment of 50 carotid dissections: indications and results. J Vasc Surg 31:980–988
Kadkhodayan Y, Jeck DT, Moran CJ, Derdeyn CP, Cross DT (2005) Angioplasty and stenting in carotid dissection with or without associated pseudoaneurysm. AJNR Am J Neuroradiol 26:2328–2335
Liu AY, Paulsen RD, Marcellus ML, Steinberg GK, Marks MP (1999) Long-term outcomes after carotid stent placement for treatment of carotid artery dissection. Neurosurg 45:1368–1379
Simionato F, Righi C, Scotti G (1999) Post-traumatic dissecting aneurysm of extracranial internal carotid artery: endovascular treatment with stenting. Neuroradiol 41:543–547
Saito R, Ezura M, Takahashi A, Yoshimoto T (2000) Combined neuroendovascular stenting and coil embolization for cervical carotid artery dissection causing symptomatic mass effect. Surg Neurol 53:318–322
Heye S, Maleux G, Vandenberghe R, Wilms G (2005) Symptomatic internal carotid artery dissecting pseudoaneurysm: endovascular treatment by stent-graft. Cardiovasc Intervent Radiol 28:499–501
Lupattelli T, Garaci FG, Hopkins CE, Simonetti G (2003) Covered stent deployment and follow-up of a case of internal carotid artery pseudoaneurysm. Cerebrovasc Dis 16:98–101
Tseng A, Ramaiah V, Rodriguez-Lopez JA, Perkowshi PE, Del Santo PB, Gowda RG et al (2003) Emergent endovascular treatment of a spontaneous internal carotid artery dissection with pseudoaneurysm. J Endovascular Therapy 10:643–646
Felber S, Henkes H, Weber W, Milosavski E, Brew S, Khune D (2004) Treatment of extracranial and intracranial aneurysms and arteriovenous fistulae using stent grafts. Neurosurg 55:631–638
Sugiu K, Tokunaga K, Watanabe K, Sasahara W, Ono S, Tamiya T et al (2005) Emergent endovascular treatment of ruptured vertebral artery dissecting aneurysms. Neuroradiol 47:158–164
Rabinov JD, Hellinger FR, Morris PP, Ogilvy CS, Putman CM (2003) Endovascular management of vertebrobasilar dissecting aneurysms. AJNR Am J Neuroradiol 24:1421–1428
Schievink WI, Wijdicks EF, Michels VV, Vockley J, Godfrey M (1998) Heritable connective tissue disorders in cervical artery dissections: a prospective study. Neurology 50:1166–1169
Schievink WI, Meyer FB, Parisi JE, Wijdicks EF (1998) Fibromuscular dysplasia of the internal carotid artery associated with alpha1-antitrypsin deficiency. Neurosurg 43:229–234
Author information
Authors and Affiliations
Corresponding author
Additional information
H. Rolf Jäger and Paul S. Sidhu contributed equally as senior authors.
Rights and permissions
About this article
Cite this article
Flis, C.M., Jäger, H.R. & Sidhu, P.S. Carotid and vertebral artery dissections: clinical aspects, imaging features and endovascular treatment. Eur Radiol 17, 820–834 (2007). https://doi.org/10.1007/s00330-006-0346-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-006-0346-7