Abstract
The aim of this paper was to assess the diagnostic value of magnetic resonance (MR) fluoroscopy in the study of oesophageal motility disorders and to compare MR fluoroscopy results with those of manometry and barium contrast radiography. Twenty-five subjects referred for dysphagia and three patients in follow-up after pneumatic dilatation of the lower oesophageal sphincter to treat severe achalasia underwent esophageal manometry, barium contrast radiography and MR fluoroscopy. Examinations were performed on a 1.5 T scanner. Dynamic turbo- fast low angle shot (turbo-FLASH) sequences acquired during oral contrast agent administration were used to perform MR fluoroscopy. MR fluoroscopy correctly diagnosed achalasia in nine patients, uncoordination of esophageal body motility in ten and scleroderma oesophagus in one. Diagnostic performance was satisfactory, with a sensitivity of 87.5% and a specificity of 100% in the general depiction of motility alterations. Our work demonstrates that MR fluoroscopic examination in subject affected by oesophageal motility disorders is feasible and can properly depict motility and morphology alterations, achieving correct diagnosis in the majority of cases. Studies on larger populations are necessary to obtain statistically significant results.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Oesophageal motility disorders are commonly diagnosed by gastroenterologists in their daily routine and represent the second most frequent cause of dysphagia after benign obstructions [1]. According to the classification proposed by Spechler and Castell in 2001 [2], oesophageal motility disorders can be categorized into four major patterns of alterations (Table 1). In all of these conditions the diagnostic routine is mainly based on the combined employment of manometry and barium contrast radiography (BCR) [3]. While manometry provides a precise evaluation of each functional aspect, offering even the capability to measure the intensity of a single peristaltic wave or the opening pressure of the lower oesophageal sphincter (LES), BCR allows a simultaneous view of the morphological changes of the oesophagus and gastro-oesophageal junction (GEJ) during physiological events. This combination of instrumental and imaging approaches is successfully used for diagnosis [4–6] and follow-up [7] of most motility disorders. In the past years the radiological community has been slowly shifting its interest from all the almost longevous fluoroscopy techniques towards the new radiation-free imaging modalities, considering, most of all, the use of magnetic resonance (MR) fluoroscopy. The first MR fluoroscopy studies were performed by Riederer et al. [8] and Farzaneh et al. [9] in the late 1980s; shortly following were the forerunning approaches in the field of clinical practice, from the monitoring of biopsies [10] to the guidance of intravascular procedures [11] and the real-time depiction of swallowing [12]. Today, MR fluoroscopy represents an actual topic of research in various clinical fields, but its employment and evolution in the functional imaging of the upper gastrointestinal tract still remains limited to few preliminary works [13–15] mainly based on the evaluation of the oro-pharyngeal swallowing phase. Only Manabe et al. [16] evaluated oesophageal motility and morphology in healthy subjects, but current literature actually lacks clinical studies on subjects affected by oesophageal motility disorders. The aim of our work was to assess the diagnostic value of MR fluoroscopy in the evaluation of subjects affected by oesophageal motility disorders and to compare MR fluoroscopy results with the findings of manometry and BCR.
Materials and methods
Patient population
Between October 2004 and July 2005, 24 subjects (ten male, 14 female; mean age 55±12 years) referred for dysphagia to the Division of Gastroenterology at our hospital, and three patients in follow-up after pneumatic dilatation of LES for treatment of severe achalasia, underwent oesophageal manometry, BCR and MR fluoroscopy. The protocol was approved by the local ethics committee, and all patients gave written informed consent. A group of 15 healthy volunteers (eight male, seven female; mean age 35±5 years) who had undergone oesophageal MR fluoroscopy between August and October 2004, served as a control population.
Oesophageal manometry equipment and protocol
Manometric examinations were performed with an eight-channel polygraph (Dynograph Recorder–R 611, Viasys/Sensormedics, USA) with five registering open-tips. The polygraph probe was positioned with its distal extremity in correspondence with the GEJ, and the registration of endoluminal pressure levels was performed backwards every 0.5 mm with a “pull-through” technique, until the probe reached the cricopharyngeal sphincter. Amplitude and frequency of peristaltic waves, as well as opening and closure pressure of the LES, were measured.
BCR equipment and imaging protocol
BCR examinations were performed with a remote-controlled fluoro-orthoclinoscope (Siregraph B, Siemens, Erlangen, Germany) equipped with a professional-standard videotape recorder for slow motion and stop imaging. As oral contrast agent we employed a standard barium sulphate solution (Pronto Bario H.D. V08BA01, 250% w/v, Bracco SpA, Milan, Italy). Patients were studied while they were upright (latero-lateral and antero-posterior) and lying down (left and right oblique) during the barium swallow (10–15 ml each swallow, for a total of five or six swallows). Each swallowing sequence was recorded for 10-30 s, and the total radiographic time was limited to 3 min. Accurately reported were functional alterations (delayed clearance, raised transit time, aperistalsis, non-peristaltic contractions and reflux), as well as morphological abnormalities (filling defects, calibre alterations, narrowing/stenosis and mucosal irregularities) if present.
MR imaging: patient preparation and contrast agent
All subjects fasted for at least 4 h in order to undergo examination in basal conditions. Outside the scan room the ability of each patient to swallow a small amount of water while in prone and supine positions was tested to avoid aspiration episodes inside the magnet bore [14]. Amongst the various foodstuffs we tested as oral contrast agents in the control group, we definitively chose a mixture of semi-fluid yoghurt and gadolinium diethylene triamine penta-acetic acid (Gd-DTPA) 0.5 M, 1:100 (Multihance, Bracco SpA); the choice was made on the basis of the excellent signal intensity and barium-like physical properties of the mixture, not overlooking patient acceptance. All subjects were strictly instructed to swallow the contrast agent during the examination in a single act: it is known that reiterated deglutition during image acquisition can auto-inhibit peristalsis, causing fictitious motility alteration [17].
MR imaging: equipment and imaging protocol
All examinations were performed on a 1.5 T scanner (Magnetom Vision, Siemens; gradients 25 mT/m2, slew rate 800 T/m per second, rise time 400 m/s), equipped with phased-array coil. Scans were acquired with the patients placed first in the prone position and then in the supine position. The imaging protocol was divided into two steps. The first step was to obtain a scout view of the thorax and upper abdomen to visualize the position and bending of the oesophagus and the gastro-oesophageal junction; a breath-hold half-Fourier single-shot turbo-spin echo (HASTE) T2-weigheted sequence (Table 2) orientated on coronal and axial planes was used. The second step was the acquisition of MR fluoroscopy images during the transit of contrast agent boluses through the oesophageal lumen: a single-slice slab T1-weighted dynamic turbo- fast low angle shot (turbo-FLASH) sequence was positioned with a median sagittal orientation on the centre of the oesophageal lumen, using the HASTE scout images to determine the optimum slice angle (Fig. 1). The standard parameters of the turbo-FLASH (TFL) sequence were adequately modified (Table 2) to obtain proper visualization of oesophageal motility. The current values of TR (416 ms), TE (1.2 ms) and flip angle (8°) enabled a sequence TA of 20 s, allowing a temporal resolution of approximately 2.25 frames per second (fps). Immediately before sequence start, a small amount of contrast agent (10–15 ml) was administered directly into the mouth of the examined subjects with a 50 ml syringe connected to a silicone tube. Patients were instructed to swallow the entire bolus immediately after the onset of the audible gradient pulsations. Five series of dynamic acquisitions were obtained: four acquired on the median sagittal plane (Fig. 2) to visualize esophageal motility and one on the oblique axial plane to depict GEJ functionality.
Dynamic turbo-FLASH T1-weighted images acquired on the medial sagittal plane during oesophageal transit of contrast agent in a healthy subject (images have been sampled from the whole fluoroscopic acquisition). Images were taken at 1 s (a), 2 s (b), 4 s (c), 6 s (d), and 8 s (e) from sequence start. Note the continuous progression of the contrast agent bolus along the oesophageal lumen and the regular and complete opening of the GEJ (arrow)
MR imaging: reference parameters
In order to have reference parameters for an objective comparison with the findings of subjects affected by motility disorders, we evaluated in the control population a standard set of functional and morphological parameters calculating average and standard deviation values (AV±SD): transit time 9±1.7 s; antero-posterior oesophageal calibre 21±2.3 mm; peristalsis type was only primary peristalsis (intended as a continuous and regular progression of the contrast agent bolus from cricopharyngeal sphincter to the GEJ); GEJ functionality was that the GEJ opened at bolus passage.
Image analysis
MR fluoroscopy and BCR images were independently reviewed by two radiologists, blind to the results of manometry. To perform an optimal evaluation of oesophageal motility we reviewed the images in “cine” mode. In each patient we assessed the same set of parameters that had been evaluated in the healthy population. Three major patterns of alterations with relative diagnostic criteria were considered:
-
1.
Achalasia. In subjects with evidence of normal oesophageal calibre with smooth tapered narrowing of the distal portion (calibre >10 mm), poorly relaxing GEJ and ineffective peristalsis replaced by characteristic “to-and-fro” movements [3, 6, 7], was diagnosed as early achalasia (Fig. 3). The progressive enlargement of the oesophageal lumen (up to 50–65 mm), with completely disrupted peristalsis and extremely prolonged transit time (up to 20 s, or incomplete clearance at sequence end), were held to be the most significant findings in the advanced disease (Figs. 4, 5). In the patients who underwent pneumatic balloon dilatation of LES for achalasia, the observers considered whether the procedure obtained a successful dilatation of the sphincter, causing a permanent GEJ opening.
-
2.
Oesophageal body motility uncoordination (EBMU). Intermittent, ineffective contractions (tertiary waves) along the whole oesophageal body, diminished oesophageal calibre, with irregular “corkscrew” lumen (Fig. 6) and prolonged transit time (up to 12–15 s), in addition to mildly reduced oesophageal clearance, were considered significant diagnostic features of EBMU [4, 18, 19].
-
3.
Ineffective esophageal motility (IEM)/scleroderma esophagus (SE). For the diagnosis of IEM/SE, the readers considered a weak peristaltic activity, enlarged oesophageal lumen, GEJ incontinence with reflux and diminished clearance with delayed cleansing time [5, 20, 21].
MR fluoroscopy findings in a 45-year-old male patient with early discovered achalasia (images have been sampled from the whole fluoroscopic acquisition). Images were taken at 3 s (a), 6 s (b), 9 s (c), 12 s (d) and 15 s (e), evidencing normal oesophageal calibre with tapered narrowing of the distal portion (arrows). Primary peristalsis is replaced by characteristic ineffective “to-and-fro” movements of the contrast agent bolus (b, c, d), with strongly reduced oesophageal clearance
MR fluoroscopy findings in a 63-year-old female patient with achalasia in advanced stage (images have been sampled from the whole fluoroscopic acquisition). Time intervals between each image were at 5 s (a), 10 s (b), 15 s (c) and 20 s (d). The oesophageal lumen is grossly dilated (60 mm) and the peristaltic activity results completely disrupted, with totally insufficient bolus progression (at sequence end, contrast agent is still present in the oesophagus). Alimentary residues can be identified in the lumen (arrow)
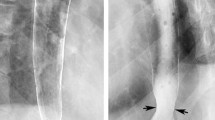
Barium fluoroscopy examination (same patient as in Fig. 6). The fluoroscopic findings strongly match those of the dynamic MR scan. The oesophagus appears grossly dilated, with an irregular and ridged aspect of the wall. Compared with MR imaging, barium fluoroscopy allows a more accurate evaluation of the GEJ that appears with the typical “beak-like” aspect
MR fluoroscopy findings in a 43-year-old female patient with diffuse oesophageal spasm (images have been sampled from the whole fluoroscopic acquisition). Time intervals were at 1 s (a), 6 s (b), 9 s (c), 12 s (d) and 15 s (e). Despite a fast filling of the oesophageal lumen, the normal transit is interrupted by intermittent, non-peristaltic, ineffective contractions (d-e), which resemble the “corkscrew” (arrow) that can commonly be seen at barium fluoroscopy. Transit time is prolonged
Results
Examinations were well tolerated in all cases. Neither difficulties nor complications were experienced during contrast administration manoeuvres or scan. Average room time, including patient preparation, was 19±3 min. The whole oesophageal region of interest, comprised of the area between the cricopharyngeal sphincter and the GEJ, was correctly visualized, acquiring good quality images in all subjects. Only one subjects had normal findings at all modalities. Diagnosed cases (Table 3) were referred to the three major patterns of alterations:
-
1.
Achalasia. On the basis of the described diagnostic criteria, MR fluoroscopy diagnosed early achalasia in three patients, advanced achalasia in six. The same results were obtained at BCR and manometric examinations. In the three patients in follow-up after pneumatic balloon dilatation of LES, MR fluoroscopy, BCR and manometry correctly assessed the successful dilatation of the sphincter. In particular, MR imaging and BCR evidenced in these patients a dilated GEJ and a reduction of the lumen calibre in relation to the re-establishment of sufficient oesophageal clearance.
-
2.
Oesophageal body motility uncoordination (EBMU). EBMU was diagnosed at MR fluoroscopy in ten patients, whilst BCR evidenced abnormal motility in 11 subjects. Amongst them, oesophageal manometry correctly differentiated six cases of diffuse oesophageal spasm (DES) and six cases of non-specific motility disorder (NEMD). Two of these patients had normal MR findings, and one had normal BCR results.
-
3.
Ineffective oesophageal motility (IEM)/scleroderma oesophagus (SE). Both MR fluoroscopy and BCR diagnosed one case of scleroderma oesophagus with characteristic findings. A case of IEM, identified by manometry, was missed by both imaging modalities.
Discussion
Background
The diagnostic work-up of oesophageal motility disorders is actually based on a combined approach of instrumental (manometry) and imaging (BCR) procedures. Manometry accurately explores functional aspects of oesophageal motility, including amplitude, frequency and effectiveness of peristaltic waves, opening and closure pressures of LES; obviously, oesophageal morphology cannot be investigated at all with this modality. BCR, instead, enables the visualization of oesophageal morphology and its modifications during physiological events. The high temporal resolution (up to 25–30 frames per second) available with this technique, in addition to an optimal spatial resolution that provides high-quality images of the bolus transit from the pharynx to the stomach, have made it the reference of choice in the field of functional imaging of the oesophagus. Although bony structures and soft tissue are superimposed, BCR can provide excellent information on bolus transport, reflux, aspiration, and residue, not forgetting the chance to evaluate oesophageal walls and lumen. However, this technique presents some important drawbacks that cannot be easily overcome: (1) subjects that undergo BCR are invariably exposed to radiation [22]; (2) soft tissue is not visualized at BCR: only indirect signs of soft tissue lesions can be recognized, and no characterization of these findings is possible; (3) if aspiration is present, the use of contrast agent may be dangerous. Still, at present, no true alternatives to BCR are available to obtain real-time imaging of oesophageal motility. With the introduction and wide diffusion of ultra-fast MR sequences, which have pushed scan times to the sub-second domain, MR fluoroscopic evaluation of physiological activity of soft tissue has become a reality, allowing a new, non-invasive approach to the visualization of most motility processes in the human body, including oesophageal functionality.
Our experience
Intended as a completely preliminary approach to the poorly explored field of oesophageal MR fluoroscopy, our work focuses on the diagnostic evaluation of subjects affected by motility disorders, facing a matching comparison with the reference modalities of the sector. The use of a consolidated protocol, refined through the study of a consistent control group, offered the possibility to perform examinations in an efficient and reproducible way. The HASTE sequence resulted in an optimal choice for the obtainment of scout views; good-quality images acquired during a single breath-hold successfully served for the positioning of functional-sequence slice slabs. The dynamic TFL sequence, owing to its low flip angle (FA 8°) and short repetition time (TR 416 ms) best fitted our technical requirements to allow proper depiction of oesophageal motility and LES functionality in all patients, with adequate spatial and temporal resolution. Gd-DTPA-based contrast agent provided optimum signal intensity, while its combination with semi-fluid yoghurt offered barium-like physical properties, improving, at the same time, patient comfort, and granting good compliance during the examination. The assessment of functional and morphological alterations in patients affected by motility disorders was easily allowed by the prompt comparison with the findings of healthy subjects; moreover, reporting our examination in accord with the general diagnostic indications available in the literature for BCR granted good concordance between MR imaging and X-ray results. The diagnostic performance of MR fluoroscopy was, overall, satisfactory (sensitivity of 87.5% and specificity of 100% in the general depiction of motility alterations), although the findings on three subjects affected by motility disorders (two with EBMU and one with IEM) were reported as normal. This issue could be related both to the fact that MR spatial and temporal resolution may be sub-optimal for the depiction of the subtle functional and morphological alterations specific to these disturbances and to the typical clinical behaviour of these pathological conditions in which the recognition of imaging findings is not constant.
Advantages and limitations of the technique
In comparison with barium fluoroscopy, the MR imaging approach to the examination of subjects affected by oesophageal motility disorders presents some important advantages. Owing to the absence of ionizing radiation, MR fluoroscopy is a totally non-invasive procedure and can be employed without danger in paediatric patients and in pregnant women (in young patients without dysphagia, suffering from non-cardiac chest pain, globus or unexplained coughing, oesophageal motility could be investigated with MR fluoroscopy as first instance examination before BCR is performed), also allowing repeated examinations at short intervals, as most follow-up protocols require. Moreover, MR fluoroscopy offers the capability to perform direct multiplanar imaging of soft-tissue structures, such as the mediastinum or diaphragm, which are totally missed at X-ray, and could represent a reliable choice for the depiction of oesophageal extra-luminal findings, as in the case of pseudoachalasia, a condition that may easily mimic achalasia or other motility disorders. The yoghurt-based contrast agent is totally innoxious and can be safely used without precautions, aversely to barium, which can occasionally cause either acute [23, 24] or chronic [25] adverse reactions, especially if aspired. It is clear, however, that our technique suffers from various significant limitations. The spatial resolution of images obtained during functional acquisitions needs to be implemented through the use of more adequate sequences in order to obtain accurate evaluation of wall abnormalities, as commonly seen at barium fluoroscopy. Temporal resolution (2.25 fps) is still too low compared to that of X-ray (25–30 fps); the lowest possible values of flip angle, TR and TE must be employed in the attempt to achieve a true real-time visualization of oesophageal motility. Considering the actual limitations in terms of spatial and temporal resolution, it is clear that MR fluoroscopy is actually unreliable in the evaluation of fine findings such as small rings, webs and long subtle stenosis, and that all these pathological conditions still need dedicated conventional imaging in order for one to obtain optimum diagnostic performance. As an example, even a positive MR examination could probably overlook an initial, low-grade stenosis of the distal oesophagus, whilst BCR would surely offer a more accurate and reliable evaluation. Lastly, the impossibility to obtain an upright view could impair the examination of some subjects, especially those with achalasia in which the transit of contrast agent boluses through the LES is often allowed only in the standing position, although we did not experience any difficulty in diagnosing this disease.
Conclusions
In conclusion, our study demonstrates that MR fluoroscopic examination in subjects affected by oesophageal motility disorders is feasible and can properly depict motility and morphology alterations typical of these pathological conditions. This imaging modality is rapid, non-invasive, reproducible, and without discomfort for patients. Although our technique is absolutely far from the “state of the art” and represents an absolutely preliminary experience in the field of MR fluoroscopy, the optimization of this protocol and the assessment of appropriate functional and morphological MR patterns of abnormalities could most likely represent a promising step on a new path for the employment of magnetic resonance imaging in the evaluation of subjects affected by oesophageal motility disorders. An extensive study on a larger population and with the employment of a more advanced MRI unit is still necessary to consolidate and eventually upgrade the protocol and to confirm the encouraging results obtained with this work-in-progress technique.
References
Esfandyari T, Potter JW, Vaezi MF (2002) Dysphagia: a cost analysis of the diagnostic approach. Am J Gastroenterol 97:2733–2737
Spechler S J, Castell DO (2001) Classification of oesophageal motility abnormalities. Gut 49:145–151
Richter JE (2001) Oesophageal motility disorders. Lancet 358:823–828
Prabhakar A, Levine MS, Rubesin S, Laufer I, Katzka D (2004) Relationship between diffuse esophageal spasm and lower esophageal sphincter dysfunction in barium studies and manometry in 14 patients. AJR Am J Roentgenol 183:409–413
Fuller L, Huprich JE, Theisen J, Hagen JA, Crookes PF, Demeester SR, Bremner CG, Demeester TR, Peters JH (1999) Abnormal esophageal body function: radiographic–manometric correlation. Am Surg 65:911–914
Schima W, Ryan JM, Harisinghani M, Schober E, Pokieser P, Denk DM, Stacher G (1998) Radiographic detection of achalasia: diagnostic accuracy of videofluoroscopy. Clin Radiol 53:372–375
Fiorentino E, Barbiera F, Grassi N, Buscemi G, Latteri S, Valenti A, Mastrosimone A (2005) Digital videofluorography and esophageal achalasia: from diagnosis to follow-up. Chir Ital 57:59–64
Riederer SJ, Tasciyan T, Farzaneh F, Lee JN, Wright RC, Herfken RJ (1988) MR fluoroscopy: technical feasibility. Magn Reson Med 8:1–15
Farzaneh F, Riederer SJ, Lee JN, Tasciyan T, Wright JC, Spritzer CE (1989) MR fluoroscopy: initial clinical studies. Radiology 171:545–549
Lufkin R, Teresi L, Chiu L, Hanafee W (1988) A technique for MR guided needle placement. AJR Am J Roentgenol 151:193–196
Dumoulin CL, Souza SP, Darrow RD (1993) Real-time positioning of invasive devices using magnetic resonance. Magn Reson Med 29:411–415
Hagen R, Haase A, Matthaei D, Henrich D (1990) Diagnosis of oropharyngeal function with FLASH-MR tomography. HNO 38:421–425
Anagnostara A, Stoeckli S, Weber OM, Kollias SS (2001) Evaluation of the anatomical and functional properties of deglutition with various kinetic high-speed MRI sequences. J Magn Reson Imaging 14:194–199
Barkhausen J, Goyen M, von Winterfeld F, Lauenstein T, Arweiler-Harbeck D, Debatin JF (2002) Visualization of swallowing using real-time TrueFISP MR fluoroscopy. Eur Radiol 12:129–133
Ajaj W, Goyen M, Herrmann B, Massing S, Goehde S, Lauenstein T, Ruehm SG (2005) Measuring tongue volumes and visualizing the chewing and swallowing process using real-time TrueFISP imaging: initial clinical experience in healthy volunteers and patients with acromegaly. Eur Radiol 15:913–918
Manabe T, Kawamitsu H, Higashino T, Lee H, Fujii M, Hoshi H, Sugimura K (2004) Esophageal magnetic resonance fluoroscopy: optimization of the sequence. J Comput Assist Tomogr 28:697–703
Aly Y A (2000) Digital radiography in the evaluation of oesophageal motility disorders. Clin Radiol 55:561–568
Brusori S, Braccaioli L, Bna C, Lugaresi ML, Di Simone MP, Mattioli S, Gavelli G (2001) Role of videofluorography in the study of esophageal motility disorders. Radiol Med (Torino) 101:125–132
Schima W, Stacher G, Pokieser P, Uranitsch K, Nekahm D, Schober E, Moser G, Tscholakoff D (1992) Esophageal motor disorders: videofluoroscopic and manometric evaluation—prospective study in 88 symptomatic patients. Radiology 185:487–491
Nelson JB, Castell DO (1988) Esophageal motility disorders. Dis Mon 34:297–389
Ipsen P, Egekvist H, Aksglaede K, Zachariae H, Bjerring P, Thommesen P (2000) Oesophageal manometry and video-radiology in patients with systemic sclerosis: a retrospective study of its clinical value. Acta Derm Venereol 80:130–133
Crawley MT, Savage P, Oakley F (2004) Patient and operator dose during fluoroscopic examination of swallow mechanism. Br J Radiol 77:654–656
Gernez Y, Barlesi F, Doddoli C, Chetaille B, Forel JM, Astoul P, Papazian L (2005) Acute respiratory distress syndrome following inhalation of barium sulphate. Rev Mal Respir 22:477–480
Gray C, Sivaloganathan S, Simpkins KC (1989) Aspiration of high-density barium contrast medium causing acute pulmonary inflammation—report of two fatal cases in elderly women with disordered swallowing. Clin Radiol 40:397–400
Voloudaki A, Ergazakis N, Gourtsoyiannis N (2003) Late changes in barium sulfate aspiration: HRCT features. Eur Radiol 13:2226–2229
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Panebianco, V., Habib, F.I., Tomei, E. et al. Initial experience with magnetic resonance fluoroscopy in the evaluation of oesophageal motility disorders. Comparison with manometry and barium fluoroscopy. Eur Radiol 16, 1926–1933 (2006). https://doi.org/10.1007/s00330-006-0246-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-006-0246-x