Abstract
Leukodystrophies are genetically determined metabolic diseases, in which the underlying biochemical abnormality interferes with the normal build-up and/or maintenance of myelin, which leads to hypo- (or arrested) myelination, or dysmyelination with resultant demyelination. Although conventional magnetic resonance imaging has significantly contributed to recent progress in the diagnostic work-up of these diseases, diffusion-weighted imaging has the potential to further improve our understanding of underlying pathological processes and their dynamics through the assessment of normal and abnormal diffusion properties of cerebral white matter. Evaluation of conventional diffusion-weighted and ADC map images allows the detection of major diffusion abnormalities and the identification of various edema types, of which the so-called myelin edema is particularly relevant to leukodystrophies. Depending on the nature of histopathological changes, stage and progression gradient of diseases, various diffusion-weighted imaging patterns may be seen in leukodystrophies. Absent or low-grade myelin edema is found in mucopolysaccharidoses, GM gangliosidoses, Zellweger disease, adrenomyeloneuropathy, L-2-hydroxyglutaric aciduria, non-ketotic hyperglycinemia, classical phenylketonuria, Van der Knaap disease and the vanishing white matter, medium grade myelin edema in metachromatic leukodystrophy, X-linked adrenoleukodystrophy and HMG coenzyme lyase deficiency and high grade edema in Krabbe disease, Canavan disease, hyperhomocystinemias, maple syrup urine disease and leukodystrophy with brainstem and spinal cord involvement and high lactate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term leukodystrophy refers to a pathological process, most commonly of metabolic origin, involving the cerebral white matter exclusively or dominantly [1]. The so-called classical leukodystrophies (e.g., metachromatic leukodystrophy, globoid cell leukodystrophy, Canavan disease and X-linked adrenoleukodystrophy) are genetically determined diseases that adversely affect the normal myelin turnover. More recently, several additional entities, such as megalencephalic leukoencephalopathy with subcortical cysts, Aicardi-Goutière syndrome, vanishing white matter disease, leukodystrophy with brainstem and spinal cord involvement and high lactate and others have been described. Furthermore, since the advent of MR imaging, a large number of additional metabolic diseases (organic and amino acidopathies, etc.) have been identified that also present with dominantly white matter lesions, but have never been regarded as leukodystrophies.
Indeed, leukodystrophies are essentially histopathological and radiological entities, but the term is justified from the clinical point of view, too. Leukodystrophies usually present with cortical-spinal tract, in particular with pyramidal signs. This is in contrast to diseases affecting grey matter structures, the so-called poliodystrophies, the classical presentation of which is typically seizures and/or extrapyramidal movement disorders [1–3]. It is nevertheless noteworthy that in poliodystrophies some degree of white matter involvement is often present, and conversely, many leukodystrophies present with clinical and radiological evidence of grey matter involvement.
In leukodystrophies or leukodystrophy-like conditions, the underlying pathological processes may be diverse, notably delayed myelination, dysmyelination or demyelination, or quite frequently a combination of them [4–6]. In delayed myelination the composition of the produced myelin is normal; it is only the pattern and extent of the myelination that is inappropriate for the age. The absence or abnormality of one or more of the essential constituents of myelin (e.g., the incorporation of abnormally large quantities of very long chain fatty acids in peroxisomal disorders) leads to dysmyelination (abnormal histochemical structure of myelin), which may be associated with hypomyelination. The produced myelin is sparse, fragile and prone to breakdown, potentially leading to partial or complete demyelination (loss of myelin) after a variable length of time. The term demyelination may therefore refer to loss of either primarily normal or abnormal myelin. Possible causes of demyelination include a wide range of pathologies, notably inflammatory, toxic, ischemic, etc. In leukodystrophies dysmyelination is a frequent, perhaps the most common cause of demyelination, but a direct toxic effect or even reactive inflammatory changes may also play a role in some entities. The process of demyelination may be rather rapid in some white matter diseases and quite slow in others, and the triggering factor is often unknown.
All of the above necessitate the redefinition of the term leukodystrophy. Indeed, leukodystrophies comprise any inborn error of metabolism that interferes with the normal build-up and/or maintenance of myelin and hence has the potential to cause hypo- (or arrested) myelination, or dysmyelination with resultant demyelination.
On conventional MR imaging, delayed myelination is often easy to identify, but occasionally it may be difficult to differentiate from a coexisting demyelinating process of early onset. Dysmyelination may, but in most cases does not have conventional imaging manifestations until it leads to demyelination. Advanced MR techniques, such as proton MR spectroscopy and in particular diffusion-weighted imaging seem to further enhance the diagnostic sensitivity and specificity of the MR imaging work-up by more accurately identifying and differentiating the above pathological processes. For instance, in proton MR spectroscopy, increased choline content in normal appearing white matter—reflecting increased myelin turnover—can be an early indicator of demyelination. Despite its great potential and widespread use, the value of diffusion-weighted MR imaging in leukodystrophies has not been assessed systematically to date.
Classification of leukodystrophies
Leukodystrophies are difficult to classify because of the diversity of biochemical derangements potentially leading to white matter abnormalities. Possible metabolic errors may include peroxisomal disorders, lysosomal storage disorders, organic acidurias, aminoacidemias and other relatively rare disorders. In some of them, however, the underlying metabolic abnormality is not known at all (Table 1).
The principles of diffusion-weighted MR imaging and its relevance to the diagnostic imaging work-up of leukodystrophies
Diffusion-weighted imaging (DWI) is a functional imaging technique at the cellular level. In homogeneous media (such as water), the phenomenon of diffusion is the net movement of molecules due to a concentration gradient. In biological specimens, however, diffusion is more complex. Besides concentration gradients, pressure and thermal gradients, available volume fractions, space tortuosity, as well as ionic interactions also play some role. Hence, it is actually referred to as apparent diffusion.
Diffusion-weighted imaging in biological specimens relies on the detection of differences in water diffusion (intravoxel incoherent motion) properties of various tissues. The normal or abnormal diffusion properties of a biological specimen can be quantified; the two most commonly used parameters are the apparent diffusion coefficient (ADC) and the so-called tensor fractional anisotropy (FA) values. While the apparent diffusion coefficient describes only the overall gross mobility of the water molecules in a given tissue environment, determining fractional anisotropy provides additional information about the magnitude of anisotropy of diffusion, hence, indirectly, about the integrity of white matter tracts and cellular microstructure [7]. The latter, however, requires the availability of diffusion tensor imaging (DTI), which is not the subject of the present review.
Diffusion information may be displayed in a conventional, image-based fashion. On these so-called conventional diffusion-weighted images, the signal is the product of a T2-weighted echo planar background image, modified (typically attenuated) by the rate of apparent diffusion in the direction of the applied diffusion gradient. As a result, decreased water diffusion presents with hypersignal and, conversely, increased water diffusion with hyposignal on diffusion-weighted images.
However, because of the rather heavily T2-weighted echo-planar background image, diffusion-weighted images always contain some T2 information. For this reason, tissues or lesions with very long T2-relaxation time may contaminate the diffusion data and actually “shine through” the images, giving the false impression of water diffusion restriction. This potential problem can be reduced or eliminated by the use of strong b values and correlation with the so-called ADC map images, the latter—by definition—contain exclusively diffusion information and hence are free of any T2 contamination effect.
In the mature brain and under normal conditions, water diffusion is schematically isotropic in grey matter and markedly anisotropic within white matter. Anisotropy of cerebral white matter is the result of the so-called premyelination and the actual myelination process during intrauterine life and infancy [8–10]. As myelination progresses, water diffusion becomes increasingly anisotropic. As a result, the apparent diffusion coefficient of the white matter decreases, whereas the fractional anisotropy increases. The “physiological” anisotropy of white matter is mainly determined by axonal directions, but the amount and quality of the myelin, fiber size and cell types present also play a role. Indeed, water diffusion is relatively free along the axons and restricted across the myelin sheath.
Previously acquired anisotropy within brain parenchyma may however also be lost as a result of a wide spectrum of pathological processes, which include primary or secondary white matter diseases. Abnormal water diffusion in the brain may develop in two ways; it can become increased or decreased, but in both situations with a tendency towards isotropy. These changes are easily demonstrated by diffusion-weighted imaging and constitute the basis for differentiation of various edema types, which has great differential diagnostic importance in various pathological processes, including white matter diseases.
Edema is a non-specific reaction of brain parenchyma to different noxae. Depending on the underlying pathophysiological mechanisms, vasogenic, interstitial, cytotoxic or so-called myelin (intramyelinic) edemas may develop. All of them may affect the white matter, but the first two are characterized by isotropically increased, the latter two by isotropically restricted water diffusion.
The development of edemas is typically related to loss of structural or functional integrity of specific anatomical barriers.
Vasogenic edema is secondary to loss of integrity of the blood-brain barrier; hence, abnormal migration of water from the intravascular into the extracellular space occurs. Interstitial edema is typically encountered in acute hydrocephalus and is related to the loss of the integrity of the ependyma and subsequent transependymal permeation of cerebrospinal fluid. In both conditions, the excess water diffuses relatively freely and randomly within the expanded interstitial space and hence vasogenic and interstitial edemas present with hyposignal on diffusion-weighted images and hypersignal on ADC maps.
In cytotoxic edema initially the functional (Na/K pump) and later the structural integrity of the cellular membrane is lost, leading to an abnormal shift of extracellular fluid into the intracellular space. The entrapped intracellular fluid and the increased viscosity in the extracellular space result in apparent restriction of water diffusion. Myelin edema typically develops in demyelinating diseases, some of which present histopathologically as vacuolating (or spongiform) myelinopathy [4]. In such cases, presumably small, fluid-containing vacuoles develop within or under myelin layers, because of the loss of integrity of the myelin sheet itself. It is suggested that within vacuoles, water diffusion is restricted, similar to cytotoxic edema. However, vacuolating myelinopathy may not be the only cause of what is referred to as “myelin edema” on diffusion-weighted images. Both cytotoxic and myelin edemas present with hypersignal on diffusion-weighted images and hyposignal on ADC maps.
In diffusion-weighted imaging evaluation of white matter diseases in general, differentiation between vasogenic versus myelin edema has great importance. Myelin edema in leukodystrophies is usually associated with active demyelination. It may be easily detected by the hypersignal on diffusion-weighted images. Acute vasogenic edema in white matter may also occur in some metabolic disorders, especially during metabolic crises, but also in so-called leukodystrophy mimics (e.g., toxic encephalopathies). On conventional MR images it may be impossible to differentiate vasogenic edema from myelin edema; nevertheless, with diffusion-weighted imaging this is straightforward.
After demyelination is accomplished—leading to loss of the tissue matrix—the physiological anisotropy of the white matter is reduced or permanently lost. Since both acute (myelin edema) and chronic histopathological changes (myelin loss, tissue rarefaction and gliosis) present with hypersignal on conventional T2-weighted images, but are distinctly different on diffusion-weighted images (myelin edema is hyperintense, whereas demyelinated, rarefied white matter and gliosis present with hyposignal), diffusion-weighted imaging is also valuable in the detection of disease activity and monitoring of disease progression from active to burned-out stages in leukodystrophies.
The diffusion-weighted imaging characteristics of leukodystrophies
Lysosomal disorders
Lysosomes are cellular organelles that contain various enzymes, the deficiencies of which lead to impaired breakdown and subsequently abnormal accumulation of specific macromolecules (proteins, nucleic acids, lipids, lipoproteins and polysaccharides). This progressively interferes with the normal function of the cell, and so-called storage diseases develop [11]. Depending on the function of the deficient enzyme and the abnormally accumulated macromolecules, several types and subtypes of lysosomal storage diseases are known. Involvement of the neural cells by the disease causes disintegration of the neuro-axonal units, whereas dysfunction of the oligodendrocytes adversely affects myelin build-up and maintenance.
Metachromatic leukodystrophy
Metachromatic leukodystrophy is caused by a deficiency of cerebroside sulfatase enzyme. As a result, galactocerebroside sulfate accumulates within oligodendrocytes and Schwann cells. Thus, myelin within both the central nervous system and peripheral nerves becomes unstable and prone to abnormal breakdown. The disease, therefore, may be regarded as an example of dysmyelination-induced demyelination.
In its classical (infantile) form, metachromatic leukodystrophy is a pure leukodystrophy with no apparent involvement of grey matter structures on MRI. The imaging abnormalities consist of progressive centrifugal white matter disease, sometimes with an additional postero-anterior gradient [12, 13]. A peculiar “tigroid” white matter lesion pattern may be seen within the centrum semiovale, which is due to the relative sparing of myelin around the transmedullary vessels. During the disease course, progressive and eventually severe diffuse brain atrophy develops and cerebellar white matter involvement may also be seen.
Diffusion-weighted images in the active stage of the disease usually show moderate hypersignal in the presumed progression zones of the disease process. The “tigroid” pattern may occasionally be conspicuous too. This suggests restricted water diffusion due to intermediate grade myelin edema [14]. ADC map data, however, indicate that some of the hypersignal may actually be due to T2-shine-through effect (Fig. 1). Therefore, the water diffusion abnormalities in the demyelinating areas may be more complex, explaining the controversial diffusion-weighted imaging findings. In the late, burned-out stage when demyelination is fully accomplished, the lesion areas are usually somewhat hypointense, consistent with rarefaction of the white matter matrix and resultant isotropically increased water diffusion (Fig. 2).
MR imaging findings in metachromatic leukodystrophy in a 3-year-old female child (acute phase). Axial T2-weighted fast spin-echo (a), diffusion-weighted (b) and ADC map (c) images. The T2-weighted image shows extensive white matter disease. On the diffusion-weighted image (b=1,000 s) the lesions areas appear to be quite uniformly hyperintense, but the ADC image provides inconsistent data. In the frontal and the deep parietal regions hyperintensities indicate increased water diffusion, therefore the hyperintensities on the diffusion-weighted images, at least partially, may correspond to T2 shine-through. Definite hypointensities are suggested only in the parietal and central periventricular areas as well as the knee of the corpus callosum; these may represent myelin edema and active demyelination
MR imaging findings in metachromatic leukodystrophy in a 10-year-old male child (chronic, burned-out phase). Axial T2-weighted fast spin-echo (a), and diffusion-weighted (b) images. In this stage of the disease, the T2-weighted image shows diffuse loss of the volume of cerebral white matter, involving all structures, including the subcortical U-fibers. On the diffusion-weighted image (b=1,000 s), the lesion areas are faintly hypointense, consistent with isotropically increased water diffusion in the demyelinated areas with practically no sign of active demyelination
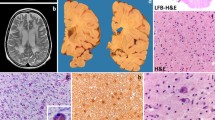
Globoid cell leukodystrophy (Krabbe disease)
The underlying metabolic derangement is the defect of galactocerebroside beta-galactosidase enzyme, resulting in the accumulation of galactocerebroside and galactosylsphingosine within the cerebral white matter. Galactosylsphingosine is known to be toxic to oligodendrocytes; hence, the disease probably affects both the production and maintenance of myelin in the central and peripheral nervous system [6].
In the classical, early infantile form, the most prominent changes are the widespread supra- and infratentorial white matter abnormalities. Supratentorially, white matter abnormalities show a centrifugal pattern with an additional postero-anterior gradient [15, 16]. With progression of the disease, practically all white matter structures become abnormal, and diffuse brain atrophy develops. Later onset forms of the disease may present with unusual imaging findings [17].
Diffusion-weighted images of the brain may show hypersignal along the progression line of the active demyelinating process in the early stage of the disease (Fig. 3). This is most probably due to myelin edema. In more advanced stages of the disease, the hyperintense signal changes subside and demyelinated areas turn into hyposignal. This indicates a complete myelin loss leading to decreased anisotropy and increased diffusivity, which are in keeping with the relentlessly progressive, devastating clinical picture [10, 18].
MR imaging findings in globoid cell leukodystrophy in an 8-month-old male child. Axial T2-weighted fast spin-echo (a), diffusion-weighted (b) and ADC map (c) images. The T2-weighted image shows extensive leukodystrophy involving all white matter structures. Note the typical hypointense appearance of the deep grey matter nuclei. Some areas exhibit prominent, others moderate hypersignal on the diffusion-weighted image (b=1,000 s). These areas are markedly or moderately hypointense on the ADC map. These lesions correspond to active demyelination and myelin edema. In the frontal and the deep occipital regions, the white matter abnormalities are faintly hypointense on the diffusion-weighted image. Accordingly, the ADC map indicates increased diffusion, consistent with complete myelin breakdown. These findings suggest a centrifugal progression pattern
Other lysosomal storage disorders
To the best of my knowledge, diffusion-weighted imaging findings have not been reported to date in other lysosomal storage disorders, such as Niemann-Pick disease, Gaucher disease, oligosaccharidoses (mannosidoses, fucosidoses and sialidoses), mucolipidoses, multiple sulphatase deficiency, GM1 gangliosidoses and in Chédiak-Higashi syndrome (a special form of lysosomal fusion disorder). No literature data are available on conventional diffusion-weighted imaging characteristics of some other entities either, but I have some personal experience with them.
Mucopolysaccharidoses
These diseases are caused by the impaired degradation of acid mucopolysaccharides. Manifestations of central nervous system involvement are related to excessive perivascular and intraneuronal storage of mucopolysaccharides. The imaging substrates of direct central nervous system involvement are hence enlarged perivascular spaces and white matter lesions.
Cerebral white matter lesions are most probably due to delayed myelination and/or demyelination secondary to accumulation of macromolecules within neurons and oligodendrocytes in particular. The frequency and magnitude of the characteristic imaging abnormalities are variable in different forms of mucopolysaccharidoses. White matter changes are typical for Hunter, Hurler, Hurler-Scheie, Sanfilippo and Maroteaux-Lamy disease [19].
Diffusion-weighted imaging findings are quite unremarkable in mucopolysaccharidoses. Usually iso- or faint hyposignal is seen within the white matter lesion areas, suggestive of dysmyelination and low-grade demyelination without significant myelin edema (Fig. 4).
MR imaging findings in Hurler disease (MPS-1) in a 30-month-old female child. Axial T2-weighted fast spin-echo (a) and diffusion-weighted (b) images. Enlarged perivascular spaces are seen on the T2-weighted image in conjunction with modest but diffuse white matter signal changes, most probably corresponding to hypo and dysmyelination. The diffusion-weighted image fails to show any hypersignal to suggest myelin edema
GM2 gangliosidoses
The deficient enzyme is beta-hexosaminidase A (classical and juvenile Tay-Sachs disease) or beta-hexosaminidase A and B (Sandhoff disease) in GM2 gangliosidoses. MR imaging demonstrates widespread white matter changes within the cerebral hemispheres in both forms, which probably correspond to myelin breakdown in the previously dysmyelinated white matter [20]. The pattern suggests centripetal demyelination. In the late stage of the disease, diffuse brain atrophy develops.
Diffusion-weighted images are usually quite unremarkable, which suggests a relatively slow, low grade demyelinating process without myelin edema (Figs. 5 and 6).
MR imaging findings in GM2 gangliosidosis in a 20-month-old male child. Axial T2-weighted fast spin-echo (a) and diffusion-weighted (b) images. Diffuse white matter disease is shown on the T2-weighted image, suggesting a centripetal progression patter in conjunction with involvement (note the swelling) of the basal ganglia. Relative sparing of the corpus callosum and the thalami. On the diffusion-weighted image the differentiation between the grey and white matter structures is rather poor, but no definite hypersignal is seen to suggest active demyelination and myelin edema. This case probably represents an early stage of the disease, characterized by dysmyelination, rather than significant myelin loss
MR imaging findings in a 3-year-old male child in a more advanced stage of GM2 gangliosidosis. Axial T2-weighted fast spin-echo (a), diffusion-weighted (b) and ADC map (c) images. The white matter changes on the T2-weighted image are obvious at this stage of the disease, and there is also evidence of involvement of the cortex, too. On the diffusion-weighted image most white matter areas are somewhat hypointense, and the ADC map shows high signal, too, indicating severe, advanced stage of demyelination, leading to isotropically increased water diffusion. In a few areas, frontal and parietal parasagittal cortex and immediate subcortical structures bilaterally, restricted water diffusion, as suggested by the hypersignal on the diffusion-weighted image, is confirmed by the hyposignal on the ADC map. This indicates a few remaining areas of active demyelination within the brain, which is otherwise globally demyelinated
Peroxisomal disorders
Peroxisomes are cellular organelles that have both anabolic and catabolic functions [21]. Since peroxisomes are involved in lipid metabolism, their functional integrity is indispensable in normal myelination and myelin maintenance. Peroxisomal diseases typically present with involvement of the central nervous system with a predilection of white matter, and the underlying histopathological processes include hypo-, dys- and demyelination.
Schematically, two types of peroxisomal disorders are known [22, 23]. Peroxisome assembly deficiencies (or peroxisomal biogenesis disorders) are caused by the dysfunction of practically all or several peroxisomal enzymes. Disease entities include Zellweger syndrome (and Zellweger-like syndrome), neonatal adrenoleukodystrophy, infantile Refsum disease and its variants. The other group of peroxisomal disorders comprises single enzyme deficiencies. The best-known diseases are pseudoneonatal adrenoleukodystrophy, X-linked adrenoleukodystrophy, adrenomyeloneuropathy, classical Refsum disease and pseudo-Zellweger syndrome. Rhizomelic chondrodysplasia punctata is an intermediate form between the generalized and the single protein peroxisomal disorders.
Zellweger syndrome
Zellweger syndrome is the most severe form of the peroxisomal assembly deficiencies. Histopathological work-up of the brain shows cortical dysplasia and neuronal migration disorders, but there is evidence of both dys- and demyelination [24].
From the MR imaging point of view, the hallmarks of the disease are bilateral, symmetrical, predominantly perisylvian polymicrogyria and markedly delayed (sometimes, almost arrested) myelination [25].
Diffusion-weighted imaging findings in Zellweger disease are rather unremarkable. The extensive hypointensities within the cerebral hemispheres correspond to non-myelinated white matter, consistent with severe retardation of the myelination process, without any evidence of active demyelination (Fig. 7). Diffusion tensor imaging findings in patients with Zellweger syndrome show reduced fractional anisotropy and elevated apparent diffusion coefficient values compared to age-matched controls [10, 26]. The fractional anisotropy changes are believed to indicate the lack of myelination of the fiber tracts, whereas the ADC value abnormalities may be related to the concomitant increase of free water diffusion within the extracellular space.
MR imaging findings in a 6-month-old female infant with Zellweger disease. Axial T1-weighted fast inversion recovery (a), diffusion-weighted (b) and ADC map (c) images. Poor overall myelination is seen on the inversion recovery image with some myelin shown within the internal capsules and the optic radiations only. The diffusion-weighted (b=1,000 s) and ADC map images do not provide evidence of active demyelination, but suggest lack of the physiological anisotropy in the peripheral white matter structures, consistent with severely delayed and hypomyelination
X-linked adrenoleukodystrophy
This is a true leukodystrophy, with no lesions within the grey matter structures. White matter abnormalities usually appear in the occipital regions initially, with early involvement of the splenium of the corpus callosum and posterior limbs of internal capsules [27]. The progression pattern of the disease is centrifugal and postero-anterior [28]. This results in the most characteristic imaging (and histopathological) feature of the disease [24]. Three distinct zones are identified in hemispheric white matter lesion areas. The center corresponds to the fully demyelinated, inactive burned-out zone. Around this area, an intermediate zone is seen, in which signal enhancement is frequently, but not always seen after intravenous contrast injection. Histopathologically, this corresponds to the inflammatory zone. Peripherally, a zone of active demyelination is identified. In the terminal stage of the disease, all supratentorial and cerebellar white matter structures are involved [28].
On conventional diffusion-weighted images, the three distinctly different lesion zones are also conspicuous. The burned-out zone is hypointense (total loss of diffusional anisotropy, due to loss of tissue matrix), the intermediate inflammatory zone is moderately hyperintense (restricted water diffusion, possibly due to low grade myelin edema and hypercellularity caused by lymphocytic infiltration) and the most peripheral demyelinating zone is very faintly hyperintense, perhaps due to T2-shine through [10] (Fig. 8). Diffusion tensor imaging findings are somewhat controversial. On the one hand, it was found to offer higher sensitivity than conventional MR or diffusion-weighted imaging in the detection of early demyelination by demonstrating increased isotropic diffusion and decreased fractional anisotropy in normal-appearing white matter structures [29]. However, in another study no significant diffusion tensor imaging abnormalities were found in normal-appearing white matter in either clinically symptomatic or asymptomatic patients [30].
MR imaging findings in a 6-year-old male child in X-linked adrenoleukodystrophy. Axial fast FLAIR (a), gadolinium-enhanced T1-weighted spin-echo (b), diffusion-weighted (c) and ADC map (d) images. Prominent and symmetrical white matter changes are shown in the parietal regions, within which the three distinct zones are well identified. The intermediate zone is markedly hyperintense on the FLAIR image and shows enhancement on the gadolinium enhanced T1-weighted image. This zone is hyperintense on the diffusion-weighted image (b=1,000 s) and hypointense on the ADC map, consistent with isotropically restricted water diffusion. Anterior to this, the zone of demyelination shows faint hypersignal on the diffusion-weighted image, but the signal is hyperintense on the ADC map, hence it mainly corresponds to T2-shine-through. The demyelinated zone is hypointense on the diffusion-weighted image and hyperintense on the ADC map, indicating increased, isotropical water diffusion due to demyelination and loss of tissue matrix. In the frontal regions the white matter is normal on all image types, but MR spectroscopic and quantitative diffusion data suggest abnormalities in the normal appearing white matter too in patients with X-ALD
Adrenomyeloneuropathy
Adrenomyeloneuropathy is one of the clinical phenotypes of X-linked adrenoleukodystrophy in which signs and symptoms of cerebellar, spinal cord and peripheral nerve involvement dominate the neurological presentation [31, 32].
In MR imaging the most frequently involved structures are the posterior limbs of the internal capsules, brainstem and cerebellar white matter. Occasionally, lesions may be seen within hemispheric white matter, especially in the advanced stage of the disease [28, 31].
In one personal case, diffusion-weighted images showed little evidence of active demyelination (Fig. 9). The findings suggest a lower grade demyelination, consistent with the more benign and protracted course of the disease compared to X-linked adrenoleukodystrophy.
MR imaging findings in a 30-year-old male patient in adrenomyeloneuropathy. Axial T2-weighted fast spin-echo (a, c) and diffusion-weighted (b, d) images. The brainstem and cerebellar white matter abnormalities are obvious on the T2-weighted image (a), but no active demyelination is shown on the corresponding diffusion-weighted image (b). Supratentorially, the white matter lesions are limited to the posterior limbs of the internal capsules (c), where the diffusion-weighted image (b=1,000 s) suggests small areas of hypersignal posteriorly, which may indicate loss of physiological anisotropy and restricted diffusion, consistent with some ongoing demyelination and myelin edema (d)
Other peroxisomal disorders
In other peroxisomal disorders, no diffusion-weighted imaging findings have been reported to date.
Organic acidopathies
Organic acidopathies usually present with grey matter disease, some degree of white matter involvement, however, is not rare. In a few of them, the white matter disease may actually dominate the imaging findings.
3-hydroxy-3-methylglutaryl (HMG)-coenzyme A lyase deficiency
The impairment of the catabolic pathway of HMG coenzyme A leads to inadequate ketogenesis and inhibition of normal intrinsic gluconeogenesis, which result in global metabolic fuel depletion. This has an adverse effect on the developing brain, including myelinogenesis.
Initially grey matter abnormalities may be more obvious on MR images, since white matter is not myelinated yet. With increasing age, white matter changes (which most probably correspond to dys- and subsequent demyelination) become obvious. In some phenotypes the white matter lesions are dominantly periventricular or subcortical; in others lesions they may be found in both periventricular and subcortical, or in exclusively subcortical locations [33, 34].
Diffusion-weighted imaging shows faint hypersignal within the involved grey or white matter structures, indicating an intermediate grade cytotoxic and myelin edema (Fig. 10).
MR imaging findings in a 3-year-old female patient in 3-hydroxy-3-methylglutaryl (HMG)-coenzyme A lyase deficiency. Axial T2-weighted fast spin-echo (a), diffusion-weighted (b) and ADC map (c) images. The cerebral hemispheric white matter appears to be diffusely and quite homogenously abnormal on the T2-weighted image. The diffusion-weighted image (b=1,000 s) suggests an intermediate intensity demyelination, which is most prominent in the subcortical regions, possibly indicating a centrifugal progression pattern in this particular case. Restriction of water diffusion within lesion areas is confirmed by the hyposignal on ADC map image
L-2-hydroxyglutaric aciduria
Clinically, L-2-hydroxglutaric aciduria is a slowly progressive metabolic disorder with a relatively mild clinical presentation. MRI examination of the brain, however, reveals rather prominent brain abnormalities, the overall pattern of which is practically pathognomonic of the disease [35].
White matter abnormalities exhibit a typical centripetal and slightly antero-posterior gradient; subcortical U-fibers are most severely affected. Conversely, periventricular white matter, and in particular the central cortical-spinal tracts and corpus callosum, are spared for quite a long time. The basal ganglia and dentate nuclei are always abnormal.
Diffusion-weighted images are rather unremarkable. The most prominently abnormal peripheral hemispheric white matter structures are hypointense (Fig. 11). No definite hypersignal is seen elsewhere in white matter to suggest myelin edema. Investigators found increased ADC values in the white matter lesion areas [36, 37]. This is consistent with loss of tissue matrix in a context of a very slowly progressive, low-grade demyelinating disease, which histologically corresponds to a spongiform encephalopathy.
MR imaging findings in a 7-year-old male child in L-2-hydroxyglutaric aciduria. Axial fast modular inversion recovery (a), diffusion-weighted (b) and ADC map (c) images. The conventional T2-weighted image shows extensive white matter disease with an essentially centripetal progression, but with an additional antero-posterior gradient. The heads of the caudate nuclei are also involved. On the diffusion-weighted image (b=1,000 s) the white matter lesions are hypointense, consistent with significant myelin loss and resultant isotropically increased water diffusion. No evidence of myelin edema, which is suggestive of a very low grade, slow demyelinating process. The mild hypersignal along the lateral aspect of the heads of the caudate nuclei is most probably T2 shine-through artifact, as suggested by the isointense appearance on the ADC map image
Canavan disease (N-acetylaspartic aciduria)
In Canavan disease the underlying biochemical abnormality is derangement of the metabolism of N-acetyl aspartate (NAA). The synthesis of NAA within the central nervous system is intact, but NAA is not catabolized. Histological examination of the brain in Canavan disease shows spongy degeneration of white matter in conjunction with myelin edema (without axonal damage) and swelling of the astrocytes. Since NAA probably functions as a water transporter, this may be related to a profound impairment of water homeostasis of the brain resulting in a fluid imbalance between the intracellular (axon-glial) and extracellular (interlamellar) spaces within myelinated white matter. Accumulation of NAA within neurons leads to increased water migration from the axon into the periaxonal space, where excess water progressively builds up, causing a rupture of the sealed interlamellar spaces. Hence, intramyelinic edema develops, which eventually leads to demyelination and loss of glial cells [38].
MR imaging findings are pathognomonic in the active stage of Canavan disease. Practically all white matter structures of the brain are involved, but the relative sparing of internal capsules and corpus callosum during the early stage of the disease suggests a centripetal progression pattern [39]. MR imaging shows abnormalities within thalami and globi pallidi, too. In the burned-out phase the brain is atrophic.
Since Canavan disease seems to represent a global disturbance of cerebral water homeostasis, diffusion-weighted imaging has great potential relevance in the diagnosis and the better understanding of the underlying histopathological phenomena. Indeed, diffusion-weighted images show rather uniform hypersignal within abnormal white matter structures as well as decreased ADC values, consistent with isotropically restricted water diffusion, probably due to the intramyelinic water accumulation (myelin edema) or a gel state of water molecules in the extracellular space [10, 40] (Fig. 12). In the burned-out phase, after gross myelin breakdown, this decreases, but usually does not totally disappear; indicating the prolonged persistence of some of the underlying pathological processes causing diffusion abnormalities (Fig. 13).
MR imaging findings in a 1-year-old male patient in Canavan disease (acute phase). Axial T2-weighted fast spin-echo (a) and diffusion-weighted (b) images. Diffuse prominent hypersignal within cerebral white matter, with the exception of the parietal periventricular regions, where spongy necrotic changes are suggested on the T2-weighted image. On the diffusion-weighted image (b=1,000 s), the white matter abnormalities seem to be characterized by isotropically restricted water diffusion, probably in a context of vacuolating myelinopathy. Within the parietal periventricular areas of tissue rarefaction, the diffusion is isotropically increased, very similar to the lateral ventricles
MR imaging findings in a 6-year-old male patient in Canavan disease (chronic phase). Low signal within the subcortical regions and some persistent hypersignal (myelin edema) in the deep periventricular areas are seen on the diffusion-weighted image (b=1,000 s), somewhat more marked at the level of the knee of the corpus callosum, consistent with the centripetal progression pattern of the demyelinating process
Amino-acidopathies
Amino acidopathies typically present with white matter abnormalities on conventional MR imaging.
Maple syrup urine disease
Maple syrup urine disease (MSUD) is related to a deficiency of the metabolism of branched-chain amino acids (L-leucine, L-isoleucine and L-valine).
The most severe, classical neonatal form of MSUD is characterized by early postnatal onset and rapidly progressive neurological deterioration [41]. During the acute metabolic crisis both CT and conventional MR imaging show diffuse swelling of the brain. On the one hand, this is related to the severe vasogenic edema, which involves non-myelinated white matter structures. On the other hand, within the myelinated brain areas another edema type also develops; it is believed to be secondary to vacuolating myelinopathy, therefore represents myelin edema [42, 43]. The exact pathomechanisms leading to the development of the two edema types is unknown, but vasogenic edema is seen exclusively during the acute metabolic decompensation, while some, often quite subtle, myelin edema is usually present during the compensated periods, too.
Identification and differentiation of the two distinctly different edema types is straightforward with diffusion-weighted imaging. Myelin edema presents with isotropically restricted water diffusion, hence appears to be hyperintense on all directional anisotropy images. Fractional anisotropy (FA) is also decreased in areas of myelin edema [44]. On the contrary, vasogenic edema is characterized by isotropically increased water diffusion, which causes hyposignal. On ADC map images, areas of myelin edema are hypointense [45–48] (Fig. 14). The diagnosis of MSUD has been revolutionized by diffusion-weighted imaging in recent years. The sharp contrast between signal properties of these two edema types and the peculiar distribution of the pathological hypersignal (strictly limited to myelinated white matter structures) result in a pathognomonic pattern on conventional diffusion-weighted images.
MR imaging findings in a 28-day-old female patient in maple syrup urine disease, during metabolic crisis. Axial T2-weighted fast spin-echo (a), diffusion-weighted (b) and ADC map (c) images. Diffuse swelling of the brain and exaggerated hyperintense appearance of the white matter on the T2-weighted image. The diffusion-weighted image (b=1,000 s) shows very marked hypersignal (myelin edema) in myelinated (and presumed premyelinated) white matter structures, and hyposignal (vasogenic edema) within non-myelinated areas. The ADC map image confirms increased water diffusion in non-myelinated and restricted diffusion in myelinated structures
In the intermittent and intermediate forms of MSUD, diffusion-weighted images may show hyperintense signal abnormalities within various white matter areas, the globi pallidi and diencephalic structures; usually they are rather subtle. In treated MSUD cases, conventional MRI and diffusion-weighted imaging abnormalities almost never return to completely normal, and the pattern of the structural lesions is very similar to those observed in the intermittent form [43, 46].
Non-ketotic hyperglycinemia
Nonketotic hyperglycinemia is caused by a defect of the glycine cleavage system, which leads to accumulation of glycine in body fluids and the central nervous system, which is thought to be critical in neurotoxicity.
The imaging hallmarks of non-ketotic hyperglycinemia are callosal abnormalities and delayed or arrested myelination [49]. It seems that initially the myelination process progresses fairly normally, approximately till the age of 4 months, after which it slows down and, eventually, may become totally arrested. The progressive delay in myelination is probably associated with hypo- or dysmyelination (resulting from inappropriate synthesis of myelin precursors).
Diffusion-weighted imaging findings are often quite unremarkable; occasionally, however, they show faint hypersignal within the white matter, suggesting demyelinating activity (Fig. 15). Indeed, some data suggest the presence of restricted water diffusion, possibly indicating myelin vacuolation, within the pyramidal tracts, middle cerebellar peduncles and dentate nuclei [50].
MR imaging findings in a 13-month-old male patient in non-ketotic hyperglycinemia. Axial T2-weighted fast spin-echo (a), diffusion-weighted (b) and ADC map (c) images. Almost total absence of myelin is seen on the T2-weighted image. The diffusion-weighted image (b=1,000 s) shows faint hypersignal. On the ADC map the findings are somewhat ambiguous, in some areas faint hypo- (parietal regions) in others (frontal lobes) faint hypersignal is suggested. These findings raise the possibility of low-grade demyelination in a globally hypomyelinated brain
Hyperhomocystinemias
Hyperhomocystinemias develop in several different conditions due to the complexity of the homocysteine metabolism. Homocysteine is the product of metabolism of methionine through the so-called methyl-transfer pathway [51]. Homocysteine may be further metabolized through two different pathways, either “recycled” into methionine by methionine-synthethase or 5, 10-methylene-tetrahydrofolate reductase enzyme (remethylation pathway), or alternatively, it may be catabolized into cystathionine, cysteine and eventually sulphate (transsulphuration pathway) by cystathionine beta-synthetase.
The major clinical manifestations of hyperhomocystinemias are ophthalmological (lens dislocation), vascular (occlusive arterial or venous disease) and neurological. The latter are related to myelination abnormalities within the brain and spinal cord. Impairment of the methyl-transfer pathway is believed to be the major pathogenetic factor leading to hypo-, dys- and subsequent demyelination in hyperhomocystinemias [52, 53].
On MR imaging, cystathionine beta-reductase deficiency may present with non-specific, diffuse white matter involvement, the pattern of which is occasionally suggestive of “retrograde” demyelination [54]. In 5, 10-methylene-tetrahydrofolate reductase deficiency, MR imaging usually shows rather prominent and extensive leukodystrophy-like white matter abnormalities in the brain. In some other cases, MR imaging abnormalities are, however, milder [55]. On therapy, white matter lesions may show improvement (evidence of remyelination).
Diffusion-weighted images in the early onset forms show extensive and rather prominent hypersignal within the white matter lesions, suggestive of vacuolating myelinopathy and myelin edema (Fig. 16). Diffusion-weighted abnormalities (similar to conventional MR imaging findings) may appear later during the disease course, too, especially in poorly controlled or non-compliant cases and may remain visible on follow-up studies until appropriate treatment is administered.
MR imaging findings in a 1-year-old male patient with hyperhomocystinemia. Axial T2-weighted fast spin-echo (a), diffusion-weighted (b) and ADC map (c) images. Besides the diffuse white matter disease, the T2-weighted image shows signal abnormalities within globi pallidi, too. Both grey and white matter lesions exhibit hypersignal on the diffusion-weighted image (b=1,000 s). The ADC map confirms the isotropically restricted water diffusion within these lesions, indicating myelin edema and high-grade demyelinating process in white matter, perhaps in conjunction with cytotoxic edema within the globi pallidi
Phenylketonuria
Phenylketonuria (PKU) is a common “pure neurometabolic” disorder, and it has two forms, the more frequent “classical” type 1 phenylketonuria (98%) and the “malignant” and rare type 2.
Although phenylketonuria is associated with increased brain phenylalanine concentrations, the most likely cause of secondary central nervous system abnormalities is probably the associated decreased tyrosine and tryptophan content. Intracerebral unavailability of these amino acids causes impairment of myelin synthesis. The reduced amount of synthesized myelin (hypomyelination) is abnormal too (dysmyelination), presumably due to reduction of the sulphatide content. This causes fragility of myelin basic protein in particular, with subsequent increased myelin breakdown (demyelination). Phenylalanine itself may also have a direct toxic effect on some oligodendrocytes (so-called phenylalanine sensitive oligodendrocytes, residing in areas that myelinate after birth), leading to decreased myelin producing activity (hypomyelination) [56]. Indeed, neuropathological studies in untreated phenylketonuria patients show evidence of defective myelination (hypo- and dysmyelination) and myelin maintenance (demyelination).
In early treated patients with type 1 and type 2 phenylketonuria, MR images often show mild to moderate, dominantly parieto-occipital periventricular white matter signal abnormalities [57]. In non-compliant or untreated patients with type 1 phenylketonuria, patchy or confluent white matter changes are present, initially in the occipital periventricular region, and later extend anteriorly to frontal and temporal regions of the brain [57, 58].
On diffusion-weighted images in classical PKU, cerebral periventricular white matter lesions were found to exhibit either high signal intensity associated with decreased apparent diffusion coefficient values or an iso- or hypointense appearance and increased apparent diffusion coefficient values [59–61] (Fig. 17). These data suggest that two different types of histopathological changes may occur within cerebral white matter in classical PKU, probably representing different stages of white matter injury. Diffusion-weighted imaging data are not available in type 2 phenylketonuria to date.
MR imaging findings in a 10-year-old male patient in poorly controlled classical phenylketonuria. Axial T2-weighted fast spin-echo (a) and diffusion-weighted (b) images. The T2-weighted image shows diffuse paucity of myelin within cerebral hemispheres, perhaps with somewhat more prominent hyperintensities in frontal and peritrigonal white matter. In the latter regions, the diffusion-weighted image (b=1,000 s) shows moderate hypersignal. This may indicate ongoing demyelination in dysmyelinated areas
3-phosphoglycerate-dehydrogenase deficiency
This is the only known aminoacidopathy that affects the anabolism rather than catabolism of amino acids. MR imaging findings consist of white matter abnormalities, suggestive of a combination of delayed and hypomyelination [62]. Diffusion-weighted imaging findings have not been reported yet.
Miscellaneous
MR imaging evidence of variable degrees of white matter disease is well documented in a host of other metabolic diseases, such as galactosemia, disorders of the pyruvate metabolism, defects of the respiratory chain and in abnormality of polyol metabolism [63, 64]. In most of these entities, no diffusion-weighted imaging data are available. However, in one case of mitochondrial encephalomyopathy in a 5-month-old infant, the extensive white matter abnormalities were found to be related to vasogenic edema, as suggested by an increased apparent diffusion coefficient and decreased fractional anisotropy [65].
Leukodystrophies of unknown etiology
Megalencephalic leukoencephalopathy with subcortical cysts (Van der Knaap disease)
Affected patients present with macrocephaly. Clinically, the disease is characterized by a slowly progressive course [66]. MR imaging findings are pathognomonic. The brain is diffusely swollen during early stage of the disease; later sulcal and ventricular enlargement may be present. White matter disease is always severe and shows a clear centripetal progression pattern. Peripheral white matter structures of cerebral hemispheres are the most severely involved, as shown by the presence of large subcortical cyst formations in the fronto-parietal and temporal regions [67].
Diffusion-weighted imaging shows prominent hyposignal within subcortical cysts and decreased signal within affected white matter. The ADC is increased and diffusion tensor imaging data show reduced fractional anisotropy [67–69]. No definite hypersignal is seen within non-affected white matter structures or along the interface between normal and abnormal areas (Fig. 18). This is keeping with the clinical pattern of slow progression and suggests low grade demyelination presenting with diffuse loss of tissue matrix and increased extracellular space, but no sign of active myelin edema. These findings are in contradiction to the described underlying histopathological changes, corresponding to vacuolating myelinopathy, which typically presents with restricted water diffusion (see maple syrup urine disease, Canavan disease) [70].
MR imaging findings in a 19-month-old male patient with megalencephalic leukodystrophy with subcortical cysts (van der Knaap disease). Axial T2-weighted fast spin-echo (a, c) and diffusion-weighted (b, d) images. On the T2-weighted images the cerebral white matter is diffusely and prominently abnormal, except for corpus callosum. The diffusion-weighted images (b=1,000 s) show isotropically increased water diffusion, consistent with severe demyelination, without evidence of active, ongoing myelin breakdown, even along the interface between abnormal and spared areas. Note the temporal subcortical cysts (a), better depicted on the diffusion-weighted image by their marked hyposignal (b)
Vanishing white matter disease
Clinically the disease is characterized by a chronic progressive course, but periodical episodes of deterioration and subsequent partial improvements are typical, too [71, 72].
On MR imaging the brain appears to be slightly swollen. Cerebral hemispheric white matter changes are very prominent. As the disease progresses, signal properties of affected myelin become practically identical to those of CSF both on T1- and T2-weighted images. On FLAIR images, markedly hypointense areas are seen within deeper white matter areas, most probably corresponding to cavitations [73, 74]. On follow-up studies the extent of white matter abnormalities and, in particular of cavitations, increases, and atrophic changes progress, too.
On diffusion-weighted images the cavitated periventricular regions are markedly, other areas moderately hypointense (Fig. 19). These findings are consistent with a demyelinating process leading eventually to complete myelin loss and hence isotropically increased water diffusion. To date, however, no diffusion imaging data are available in the very early stage of the disease.
MR imaging findings in the vanishing white matter disease (courtesy of M.S. van der Knaap, Amsterdam, The Netherlands). Axial T2-weighted fast spin-echo (a) and diffusion-weighted (b) images. Very prominent myelin loss is shown in cerebral hemispheres on the T2-weighted image in all areas. The hyposignal on the diffusion-weighted image (b=1,000 s) confirms extensive demyelination, especially within deep white matter structures, leading to isotropically increased water diffusion. Total loss of tissue matrix in parietal periventricular areas (cavitations), presenting with diffusion properties identical to those of cerebrospinal fluid in ventricles. Faint hyperintensities are suggested in subcortical U-fibers in some areas, perhaps indicating some residual ongoing demyelination and myelin edema
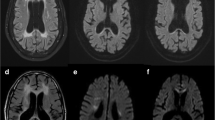
Leukodystrophy with brainstem and spinal cord involvement and high lactate
This is the most recent of the newly identified leukodystrophies [75]. Affected patients present with slowly progressive gait and sensory disturbances. The conventional MR imaging pattern consists of extensive, predominantly periventricular white matter changes within the cerebral hemispheres; the deepest white matter shows signs of rarefaction. Within the brainstem, pyramidal tracts, medial lemnisci and anterior spinocerebellar tracts, intraparenchymal trajectories of trigeminal nerves are typically involved. Spinal cord abnormalities consist of lesions within lateral corticospinal tracts and dorsal columns. On follow-up studies, no evidence of progression was found. Overall, the findings suggest a demyelinating process, with a possible associated axonal degeneration.
Diffusion-weighted imaging shows moderate, sometimes rather prominent hyperintensities within the involved deep white matter structures, suggestive of myelin edema [Fig. 20]. Measurement of mean diffusivity and fractional anisotropy also suggest primary damage to the white matter matrix.
MR imaging findings in a presumed case of leukodystrophy with brainstem and spinal cord involvement and high lactate in a 16-month-old male patient. Axial T2-weighted fast spin-echo (a and d), diffusion-weighted (b and f) images (b=1,000 s) and ADC map (c and f) images. The T2-weighted images illustrate some of the characteristic lesion pattern elements of the disease. In the brainstem, lesions within the inferior cerebellar peduncles (a) are conspicuous. The deep cerebellar white matter is also abnormal. Supratentorially, most white matter structures are involved (d). On the diffusion-weighted images the inferior cerebellar peduncles, the knee of the corpus callosum as well as the anterior limbs of the internal capsules show hypersignal, indicating restricted water diffusion. The deep peritrigonal and cerebellar white matter is hypointense, suggesting complete myelin breakdown with increased water diffusivity within rarefied tissue matrix. These data are confirmed on ADC map images
Pelizaeus-Merzbacher disease
The rare X-linked disease is most probably due to a defect of the so-called proteolipid protein, which results in impairment of myelin formation. The typical MR imaging finding in Pelizaeus-Merzbacher disease is an almost total absence of myelin within brain (connatal type) or arrested (classical form) myelination. Pelizaeus-Merzbacher disease seems to be characterized by an essentially neonatal pattern of the diffusion properties of the brain, with some detectable diffusion anisotropy, however, in specific areas, supporting the hypothesis of a dominantly non- and dysmyelinating pathomechanism [10, 76]. Nevertheless, no further age-related development of the physiological anisotropy was found.
Other entities
In some other classical leukodystrophies, such as Alexander disease, Cockayne disease and Aicardi- Goutière syndrome, no diffusion-weighted imaging findings have been published to date.
The value of conventional diffusion-weighted imaging in the diagnostic work-up of leukodystrophies
Conventional diffusion-weighted MR imaging is a robust technique that is nowadays routinely used in most clinical settings. Increasing clinical evidence suggests that diffusion-weighted imaging is a useful tool in the diagnostic imaging work-up of white matter diseases, and in particular leukodystrophies and leukodystrophy-like conditions. Its value and current role may be summarized as follows. (1) Diffusion-weighted imaging allows confident differentiation of certain edema types, in particular myelin edema from vasogenic edema with even simple visual assessment. This may be helpful in the differentiation of leukodystrophies from leukodystrophy mimics in acute diseases. However, in chronic, burned-out leukodystrophies, complete demyelination and the loss of the tissue matrix present with non-specific, isotropically increased water diffusion. (2) Diffusion-weighted imaging allows better understanding of the underlying histopathological phenomena in leukodystrophies as well as the dynamics of the disease processes. Notably, disease activity, as suggested by the presence of myelin edema, is easier to depict by diffusion than with conventional MR imaging. Furthermore, progression patterns are often better identified and progression itself better monitored by diffusion-weighted imaging than by conventional MRI. It is, however, noteworthy that apparently similar histopathological changes may present with different diffusion-weighted imaging findings (e.g., vacuolating myelinopathy in megalencephalic leukodystrophy with subcortical cysts and L-2 hydroxyglutaric aciduria does not seem to be associated with myelin edema, whereas in Canavan disease or maple syrup urine disease it is). This suggests that the term myelin edema is not necessarily related to a unique or universal pathomechanism or it occurs in specific stages of the disease process only. (3) Similarly to conventional imaging, various lesion “patterns” may be identified in leukodystrophies by diffusion-weighted imaging. Although in the majority of the cases, however, this does not enhance diagnostic sensitivity, it may be a useful adjunct to the characterization of the different entities in the process of pattern recognition. (4) As a very crude classification scheme, leukodystrophies characterized by absent, low, intermediate and high-grade myelin edema may be distinguished, depending on the diffusion-weighted imaging presentation (Table 2.). In some instances, this may be regarded as an indicator of activity of the demyelination process, which may, but does not necessarily correlate with the pattern and dynamics of clinical evolution. For example, leukodystrophy with brainstem and spinal cord involvement is a clinically very slowly progressive disease; diffusion-weighted imaging, however, usually suggests intermediate or even high-grade myelin edema at least during the early stage of the disease. Conversely, to date no myelin edema−as a possible indicator of active demyelination−has been demonstrated in vanishing white matter disease, despite clinically obvious episodes of deterioration.
Future trends
Simple visual assessment of diffusion-weighted images may provide clinically valuable information in some cases, as illustrated in many of the diseases discussed above, but may be insufficient in other situations, especially in the early stages of leukodystrophies. Therefore, it is increasingly necessary to measure and quantify diffusion parameters (apparent diffusion coefficient and fractional anisotropy) in order to enhance the diagnostic sensitivity of diffusion-weighted imaging.
Although conventional MR imaging is a powerful modality in the assessment of normal and abnormal myelination, in a yet not fully myelinated brain (e.g., in early infancy), it may be quite challenging to depict early demyelination. However, quantified diffusion-weighted imaging may be more sensitive than conventional MR imaging techniques in detecting early white matter changes in early infantile onset leukodystrophies.
Furthermore, both conventional and diffusion-weighted imaging techniques are rather inefficient in confident detection and identification of dysmyelination in white matter diseases. In the past, preserved diffusion anisotropy despite signal changes on conventional images have been believed to indicate dysmyelination. However, emerging new data suggest that diffusion tensor imaging—by selectively measuring diffusion changes in different directions—may allow more confident and early identification of dysmyelination as a potential cause of demyelination [18, 26]. This is based on the presumption that when the diffusion tensor is represented by an ellipsoid, the primary or main eigenvalue reflects the axonal integrity, whereas the secondary eigenvalues are indicators of the quality of the myelin sheath. Therefore, abnormal (increased) secondary eigenvalues may indicate myelin composition abnormalities even in cases of integrity of the neuroaxonal unit. Hence, diffusion tensor imaging is likely to push further the limits of early diagnosis of leukodystrophies, perhaps leading to increased diagnostic specificity as well in the near future. This may have great potential in early identification of affected, but clinically asymptomatic patients in very early disease stages, who are optimal candidates for preventive treatment, such as bone marrow transplantation.
References
Aicardi J (1993) The inherited leukodystrophies: a clinical overview. J Inherit Metab Dis 16:733–743
Hoon AH, Reinhardt EM, Kelley RI, Breiter SN, Morton H, Naidu S, Johnston MV (1997) Brain magnetic resonance imaging in suspected extrapyramidal cerebral palsy: observations in distinguishing genetic-metabolic from acquired causes. J Pediatr 131:240–245
Gascon GG, Ozand PT, Brismar J (1994) Movement disorders in childhood organic acidurias. Clinical, neuroimaging, and biochemical correlations. Brain Dev 16(Suppl):94–103
Kendall BE (1993) Inborn errors and demyelination: MRI and the diagnosis of white matter disease. J Inherit Metab Dis 16:771–786
Kolodny EH (1993) Dysmyelinating and demyelinating conditions in infancy. Curr Opin Neurol Neurosurg 6:379–386
Matthieu JM (1993) An introduction to the molecular basis of inherited myelin diseases. J Inherit Metab Dis 16:724–732
Huisman TA (2003) Diffusion-weighted imaging: basic concepts and application in cerebral stroke and head trauma. Eur Radiol 13:2283–2297
Prayer D, Barkovich AJ, Kirschner DA, Prayer LM, Roberts TPL, Kucharczyk J, Moseley ME (2001) Visualization of nonstructural changes in early white matter development on diffusion-weighted MR images: evidence supporting premyelination anisotropy. Am J Neuroradiol 22:1572–1576
Morriss MC, Zimmerman RA, Bilaniuk LT, Hunter JV, Haselgrove JC (1999) Changes in brain water diffusion during childhood. Neuroradiology 41:929–934
Engelbrecht V, Scherer A, Rassek M, Witsack HJ, Modder U (2002) Diffusion-weighted MR imaging in the brain in children: findings in the normal brain and in the brain with white matter diseases. Radiology 222:410–418
Beck M (2001) Variable clinical presentation in lysosomal storage disorders. J Inherit Metab Dis 24(Suppl-51)
Faerber EN, Melvin J, Smergel EM (1999) MRI appearances of metachromatic leukodystrophy. Pediatr Radiol 29:669–672
Kim TS, Kim IO, Kim WS, Choi YS, Lee JY, Kim OW, Yeon KM, Kim KJ, Hwang YS (1997) MR of childhood metachromatic leukodystrophy. Am J Neuroradiol 18:733–738
Sener RN (2003) Metachromatic leukodystrophy. Diffusion MR imaging and proton MR spectroscopy. Acta Radiologica 44:440–443
Tada K, Taniike M, Ono J, Tsukamoto H, Inui K, Okada S (1992) Serial magnetic resonance imaging studies in a case of late onset globoid cell leukodystrophy. Neuropediatrics 23:306–309
Loes DJ, Peters C, Krivit W (1999) Globoid cell leukodystrophy: distinguishing early-onset from late-onset disease using a brain MR imaging scoring method. Am J Neuroradiol 20:316–323
Turazzini M, Beltramello A, Bassi R, Del Colle R, Silvestri M (1997) Adult onset Krabbe’s leukodystrophy: a report of two cases. Acta Neurol Scand 96:413–415
Guo AC, Petrella JR, Kurtzberg J, Provenzale JM (2001) Evaluation of white matter anisotropy in Krabbe disease with diffusion tensor MR imaging: initial experience. Radiology 218:809–815
Barone R, Nigro F, Triulzi F, Musumeci S, Fiumara A, Pavone L (1999) Clinical and neuroradiological follow-up in mucopolysaccharidosis type III (Sanfilippo syndrome). Neuropediatrics 30:283–288
Yuksel A, Yalcinkaya C, Islak C, Gunduz E, Seven M (1999) Neuroimaging findings of four patients with Sandhoff disease. Pediatr Neurol 21:562–565
Fournier B, Smeitnink JAM, Dorland L, Berger R, Saudubray JM, Poll-The BT (1994) Peroxisomal disorders: a review. J Inherit Metab Dis 17:470–486
Gartner J (2000) Organelle disease: peroxisomal disorders. Eur J Pediatr 159:(Suppl-9)
Poggi-Travert F, Fournier B, Poll-The BT, Saudubray JM (1995) Clinical approach to inherited peroxisomal disorders. J Inherit Metab Dis 18:(Suppl-18)
Martin JJ (1995) Neuropathology of peroxisomal diseases. J Inherit Metab Dis 18(Suppl 1):19–33
Barkovich AJ, Peck WW (1997) MR of Zellweger syndrome. Am J Neuroradiol 18:1163–1170
ter Rahe BS, Majoie CB, Akkerman EM, den Heeten GJ, Poll-The BT, Barth PG (2004) Peroxisomal biogenesis disorder: comparison of conventional MR imaging with diffusion-weighted and diffusion-tensor imaging findings. Am J Neuroradiol 25:1022–1027
Barkovich AJ, Ferriero DM, Bass N, Boyer R (1997) Involvement of the pontomedullary corticospinal tracts: a useful finding in the diagnosis of X-linked adrenoleukodystrophy. Am J Neuroradiol 18:95–100
van der Knaap MS, Valk J (1991) The MR spectrum of peroxisomal disorders. Neuroradiology 33:30–37
Schneider JFL, Il’yasov KA, Boltshauser E, Hennig J, Martin E (2003) Diffusion tensor imaging in cases of adrenoleukodystrophy: preliminary experience as a marker for early demyelination. Am J Neuroradiol 24:819–824
Eichler FS, Itoh R, Barker PB, Mori S, Garrett ES, van Zijl PC, Moser HW, Raymond GV, Melhem ER (2002) Proton MR spectroscopic and diffusion tensor brain MR imaging in X-linked adrenoleukodystrophy: initial experience. Radiology 225:245–252
van Geel BM, Bezman L, Loes DJ, Moser HW, Raymond GV (2001) Evolution of phenotypes in adult male patients with X-linked adrenoleukodystrophy. Ann Neurol 49:186–194
van Geel BM, Assies J, Weverling GJ, Barth PG (1994) Predominance of the adrenomyeloneuropathy phenotype of X-linked adrenoleukodystrophy in The Netherlands: a survey of 30 kindreds. Neurology 44:2343–2346
Yalcinkaya C, Dincer A, Gündüz E, Ficicioglu C, Kocer N, Aydin A (1999) MRI and MRS in HMG-CoA lyase deficiency. Pediatr Neurol 20:375–380
van der Knaap MS, Bakker HD, Valk J (1998) MR imaging and proton spectroscopy in 3-hydroxy-3-methylglutaryl coenzyme A lyase deficiency. Am J Neuroradiol 19:378–382
D’Incerti L, Farina L, Moroni I, Uziel G, Savoiardo M (1998) L-2-Hydroxyglutaric aciduria: MRI in seven cases. Neuroradiology 40:727–733
Aydin K, Ozmen M, Tatli B, Sencer S (2003) Single-voxel MR spectroscopy and diffusion-weighted MRI in two patients with l-2-hydroxyglutaric aciduria. Pediatr Radiol 33:872–876
Sener RN (2003) L-2 hydroxyglutaric aciduria: proton magnetic resonance spectroscopy and diffusion magnetic resonance imaging findings. J Comput Assist Tomogr 27:38–43
Baslow MH (1999) Molecular water pumps and the aetiology of Canavan disease: a case of the sorcerer’s apprentice. J Inherit Metab Dis 22:99–101
Brismar J, Brismar G, Gascon G, Ozand P (1990) Canavan disease: CT and MR imaging of the brain. Am J Neuroradiol 11:805–810
Sener RN (2003) Canavan disease: diffusion magnetic resonance imaging findings. J Comput Assist Tomogr 27:30–33
Riviello JJ Jr, Rezvani I, Di George AM, Foley CM (1991) Cerebral edema causing death in children with maple syrup urine disease. J Pediatr 119:42–45
Sie LT, van der Knaap MS, Wezel-Meijler G, Valk J (1997) MRI assessment of myelination of motor and sensory pathways in the brain of preterm and term-born infants. Neuropediatrics 28:97–105
Brismar J, Aqeel A, Brismar G, Coates R, Gascon G, Ozand PT (1990) Maple syrup urine disease: findings on CT and MR scans of the brain in 10 infants. Am J Neuroradiol 11:121–128
Parmar H, Sitoh YY, Ho L (2004) Maple syrup urine disease: diffusion-weighted and diffusion-tensor magnetic resonance imaging findings. J Comput Assist Tomogr 28:93–97
Cavalleri F, Berardi A, Burlina AB, Ferrari F, Mavilla L (2002) Diffusion-weighted MRI of maple syrup urine disease encephalopathy. Neuroradiology 44:499–502
Jan W, Zimmerman RA, Wang ZJ, Berry GT, Kaplan PB, Kaye EM (2003) MR diffusion imaging and MR spectroscopy of maple syrup urine disease during acute metabolic decompensation. Neuroradiology 45:393–399
Righini A, Ramenghi LA, Parini R, Triulzi F, Mosca F (2003) Water apparent diffusion coefficient and T2 changes in the acute stage of maple syrup urine disease: evidence of intramyelinic and vasogenic-interstitial edema. J Neuroimaging 13:162–165
Ha JS, Kim TK, Eun BL, Lee HS, Lee KY, Seol HY, Cha SH (2004) Maple syrup urine disease encephalopathy: a follow-up study in the acute stage using diffusion-weighted MRI. Pediatr Radiol 34:163–166
Press GA, Barshop BA, Haas RH, Nyhan WL, Glass RF, Hesselink JR (1989) Abnormalities of the brain in nonketotic hyperglycinemia: MR manifestations. Am J Neuroradiol 10:315–321
Sener RN (2003) Nonketotic hyperglycinemia: diffusion magnetic resonance imaging findigns. J Comput Assist Tomogr 27:538–540
Fowler B (1997) Disorders of homocysteine metabolism. J Inherit Metab Dis 20:270–285
Surtees R (1993) Biochemical pathogenesis of subacute combined degeneration of the spinal cord and brain. J Inherit Metab Dis 16:762–770
Hyland K, Smith I, Bottiglieri T, Perry J, Wendel U, Clayton PT, Leonard JV (1988) Demyelination and decreased S-adenosylmethionine in 5,10-methylenetetrahydrofolate reductase deficiency. Neurology 38:459–462
Surtees R, Leonard J, Austin S (1991) Association of demyelination with deficiency of cerebrospinal-fluid S-adenosylmethionine in inborn errors of methyl-transfer pathway. Lancet 338:1550–1554
Engelbrecht V, Rassek M, Huismann J, Wendel U (1997) MR and Proton MR spectroscopy of the brain in hyperhomocysteinemia caused by methylenetetrahydrofolate reductase deficiency. Am J Neuroradiol 18:536–539
Dyer CA (2000) Comments on the neuropathology of phenylketonuria. Eur J Pediatr 159(Suppl 2):107–108
Bick U, Ullrich K, Stöber U, Möller H, Schuierer G, Ludolph AC, Oberwittler C, Weglage J, Wendel U (1993) White matter abnormalities in patients with treated hyperphenylalaninaemia: magnetic resonance relaxometry and proton spectroscopy findings. Eur J Pediatr 152:1012–1020
Thompson AJ, Tillotson S, Smith I, Kendall B, Moore SG, Brenton DP (1993) Brain MRI changes in phenylketonuria. Associations with dietary status. Brain 116:811–821
Phillips MD, McGraw P, Lowe MJ, Mathews VP, Hainline BE (2001) Diffusion-weighted imaging of white matter abnormalities in patients with phenylketonuria. Am J Neuroradiol 22:1583–1586
Sener RN (2003) Diffusion MRI findings in phenylketonuria. Eur Radiol 13:226–229
Sener RN (2003) Phenylketonuria: diffusion magnetic resonance imaging and proton magnetic resonance spectroscopy. J Comput Assist Tomogr 27:541–543
de Koning TJ, Jaeken J, Pineda M, Van Maldergem L, Poll-The BT, van der Knaap MS (2000) Hypomyelination and reversible white matter attenuation in 3-phosphoglycerate dehydrogenase deficiency. Neuropediatrics 31:287–292
Munoz A, Mateos F, Simon R, Garcia-Silva MT, Cabello S, Arenas J (1999) Mitochondrial diseases in children: neuroradiological and clinical features in 17 patients. Neuroradiology 41:920–928
van der Knaap MS, Wevers RA, Struys EA, Verhoeven NM, Pouwels PJ, Engelke UF, Feikema W, Valk J, Jakobs C (1999) Leukoencephalopathy associated with a disturbance in the metabolism of polyols. Ann Neurol 46:925–928
Majoie CB, Akkerman EM, Blank C, Barth PG, Poll-The BT, den Heeten GJ (2002) Mitochondrial encephalomyopathy: comparison of conventional MR imaging with diffusion-weighted and diffusion tensor imaging: case report. Am J Neuroradiol 23:813–816
van der Knaap MS, Barth PG, Stroink H, van Nieuwenhuizen O, Arts WF, Hoogenraad F, Valk J (1995) Leukoencephalopathy with swelling and a discrepantly mild clinical course in eight children. Ann Neurol 37:324–334
Sener RN (2000) van der Knaap syndrome: MR imaging findings including FLAIR, diffusion imaging, and proton MR spectroscopy. Eur Radiol 10:1452–1455
Gelal F, Calli C, Apaydin M, Erdem G (2002) van der Knaap’s leukoencephalopathy: report of five new cases with emphasis on diffusion-weighted MRI findings. Neuroradiology 44:625–630
Brockmann K, Finsterbusch J, Terwey B, Frahm J, Hanefeld F (2003) Megalencephalic leukoencephalopathy with subcortical cysts in an adult: quantitative proton MR spectroscopy and diffusion tensor MRI. Neuroradiology 45:137–142
van der Knaap MS, Barth PG, Vrensen GF, Valk J (1996) Histopathology of an infantile-onset spongiform leukoencephalopathy with a discrepantly mild clinical course. Acta Neuropathologica 92:206–212
Hanefeld F, Holzbach U, Kruse B, Wilichowski E, Christen HJ, Frahm J (1993) Diffuse white matter disease in three children: an encephalopathy with unique features on magnetic resonance imaging and proton magnetic resonance spectroscopy. Neuropediatrics 24:244–248
van der Knaap MS, Barth PG, Gabreels FJ, Franzoni E, Begeer JH, Stroink H, Rotteveel JJ, Valk J (1997) A new leukoencephalopathy with vanishing white matter. Neurology 48:845–855
Francalanci P, Eymard-Pierre E, Dionisi-Vici C, Boldrini R, Piemonte F, Virgili R, Fariello G, Bosman C, Santorelli FM, Boespflug-Tanguy O, Bertini E (2001) Fatal infantile leukodystrophy: a severe variant of CACH/VWM syndrome, allelic to chromosome 3q27. Neurology 57:265–270
Senol U, Haspolat S, Karaali K, Luleci E (2000) MR imaging of vanishing white matter. Am J Roentgenol 175:826–828
van der Knaap MS, van der Voorn P, Barkhof F, van Coster R, Krageloh-Mann I, Feigenbaum A, Blaser S, Vles JS, Rieckmann P, Pouwels PJ (2003) A new leukoencephalopathy with brainstem and spinal cord involvement and high lactate. Ann Neurol 53:252–258
Ono J, Harada K, Mano T, Sakurai K, Okada S (1997) Differentiation of dys- and demyelination using diffusional anisotropy. Pediatr Neurol 16:63–66
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Patay, Z. Diffusion-weighted MR imaging in leukodystrophies. Eur Radiol 15, 2284–2303 (2005). https://doi.org/10.1007/s00330-005-2846-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-005-2846-2