Abstract
Differentiation between different forms of pulmonary hypertension (PH) is essential for correct disease management. The goal of this study was to elucidate the clinical impact of high spatial resolution MR angiography (SR-MRA) and time-resolved MRA (TR-MRA) to differentiate between patients with chronic thromboembolic PH (CTEPH) and idiopathic pulmonary arterial hypertension (IPAH). Ten PH patients and five volunteers were examined. Twenty TR-MRA data sets (TA 1.5 s) and SR-MRA (TA 23 s) were acquired. TR-MRA data sets were subtracted as angiography and perfusion images. Evaluation comprised analysis of vascular pathologies on a segmental basis, detection of perfusion defects, and bronchial arteries by two readers in consensus. Technical evaluation comprised evaluation of image quality, signal-to-noise ratio (SNR) measurements, and contrast-media passage time. Visualization of the pulmonary arteries was possible down to a subsegmental (SR-MRA) and to a segmental (TR-MRA) level. SR-MRA outperformed TR-MRA in direct visualization of intravascular changes. Patients with IPAH predominantly showed tortuous pulmonary arteries while in CTEPH wall irregularities and abnormal proximal-to-distal tapering was found. Perfusion images showed a diffuse pattern in IPAH and focal defects in CTEPH. TR-MRA and SR-MRA resulted in the same final diagnosis. Both MRA techniques allowed for differentiation between IPAH and CTEPH. Therefore, TR-MRA can be used in the clinical setting, especially in dyspneic patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patients with different forms of pulmonary hypertension (PH) present with similar clinical symptoms, such as shortness of breath, exhaustion at minimal level of exercise, and fatigue. The diagnostic workup of these nonspecific symptoms comprises a whole list of different procedures, including electrocardiogram, echocardiography, chest X-ray, lung-function testing, perfusion scintigraphy, as well as invasive right heart catheterization and angiography [1]. The exact diagnosis is of great importance, as different forms of PH need tailored and dedicated treatment. During the last years, magnetic resonance imaging (MRI) gained more and more importance in the visualization of cardiac morphology and function [2]. Besides cardiac causes (e.g., valvular disease, congenital defects), pathological changes in the pulmonary arterial vasculature can lead to PH. These changes can be focal, as in acute or chronic pulmonary embolism (PE or CTEPH); or more diffuse, as in idiopathic pulmonary arterial hypertension (IPAH). It was already shown that high spatial resolution MR angiography (SR-MRA) is capable of visualizing the central parts of the pulmonary vasculature [3, 4]. Using a 2D time-of-flight angiography, it was possible to differentiate between CTEPH and IPAH [5]. For acquisition of SR-MRA, patients need to hold their breath for around 25 s. This is rather long for patients suffering from dyspnea like in PH, and the rate of successfully acquired data sets in severely ill patients is not reported.
Recently, parallel imaging techniques were introduced, allowing for the following improvements in MRI acquisition: (1) Spatial resolution of SR-MRA is increased, and the whole-lung volume can be covered. (2) Time-resolved MRA techniques (TR-MRA) are available, resulting in two data sets: (a) reduced spatial resolution angiography of the pulmonary arteries, and (b) perfusion-weighted data sets of the lung parenchyma [6]. The second approach seems very promising, as 3D data sets of the whole lung are acquired in 1.5 s, almost eliminating breathing artefacts. The value of both techniques for correct differentiation between different forms of PH has not yet been evaluated. As patients suffering from PH present with limited breath-holding capabilities, we expect TR-MRA to provide better image quality as less breathing artefacts will be present compared with SR-MRA. This could facilitate the differentiation of different forms of PH.
Furthermore, the increase in pulmonary vascular resistance in patients with PH leads to a prolonged pulmonary arterial transit time compared with healthy volunteers [7]. As IPAH globally affects the pulmonary arterial vasculature and CTEPH only parts of it, it might be possible to differentiate between both disease entities using the mean transit time of the bolus of contrast agent [8].
Thus, the goal of this study was to determine the clinical impact of SR-MRA and TR-MRA to differentiate between patients with CTEPH and IPAH. Furthermore, the contrast-media dynamics were compared with those of healthy volunteers.
Materials and methods
After the ethics committee approval, ten patients suffering from PH were examined with a 1.5 T whole body MRI (Magnetom Symphony, Siemens Medical Solutions, Erlangen, Germany). The first group consisted of five patients with IPAH (four female, one male, mean age 55±20 years, height 166±9 cm, weight 75±25 kg) diagnosed according to standard algorithms [1]. The second group consisted of five patients with CTEPH as proven by ventilation/perfusion (V/Q) scintigraphy, conventional pulmonary angiography, or CT angiography (CTA) (three female, two male, mean age 65±11 years, height 169±3 cm, weight 90±18 kg). For comparison of the time-resolved angiography, five volunteers (one female, four male, mean age 28±2 years, mean height 181±8 cm, mean body weight 75±11 kg) with no history of cardiovascular or pulmonary diseases were examined.
For contrast media injection, patients were equipped with an 18 G cannula in an antecubital vein. Patients were positioned with both arms placed over their head. In three patients, this was not possible, and the arms were placed alongside the body. For signal detection, a combination of two spine array coils and two four-element body phased-array coils was used. Contrast enhanced TR-MRA was performed using a 3D gradient echo pulse sequence (FLASH 3D) in coronal orientation with parallel acquisition techniques (PAT): TE/TR: 0.8/1.9 ms; flip angle: 40°; receiver bandwidth: 1,220 Hz/pixel; GRAPPA; acceleration factor 2; reference k-space lines for calibration: 20; field of view (FOV): 480×390 mm; matrix: 110×256; slab thickness: 176 mm; 44 partitions; voxel size: 3.5×1.9×4 mm3. To increase temporal resolution with an acceptable spatial resolution, additional view-sharing was implemented [9]. Using the combination of PAT and view-sharing, an acquisition time of 1.5 s per 3D data set could be achieved. A total of n=20 consecutive data sets were acquired during inspiratory breath-hold, leading to a total scan time of 30 s. Subjects were asked to hold their breath as long as possible during the data acquisition. Measurements started simultaneously with the contrast injection (0.1 mmol/kg body weight at 5 ml/s, Gd-DTPA), which were performed with an automatic power injector (Tomojet, Bruker, GE Healthcare, Ismaning, Germany) and followed by a saline flush of 20 ml at 5 ml/s.
SR-MRA was performed using a FLASH 3D sequence in coronal orientation with PAT: TE/TR: 1.17/3.05 ms; flip angle: 25°; receiver bandwidth: 650 Hz/pixel; GRAPPA; acceleration factor 2; reference k-space lines for calibration: 24; FOV: 400 mm; matrix: 288×384; slab thickness: 192 mm; 120 partitions; voxel size: 1.2×1.0×1.6 mm3; acquisition time: 23 s. Timing of the contrast media was individually adjusted based on the individual’s circulation time, which was derived from the TR-MRA using ROI analysis (tool “Mean Curve” of the scanner). During inspiratory breath-hold, 0.1 mmol/kg body weight of Gd-DTPA was injected with a flow of 5 ml/s followed by 20 ml NaCl at the same rate.
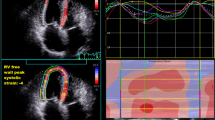
In all patients, TR-MRA was performed first, followed by SR-MRA after 30 min. Data analysis was done on the satellite console of the MR scanner. The data sets were retrospectively reviewed in consensus by two readers experienced in chest radiology who were blinded to the clinical diagnosis. The TR-MRA data sets were postprocessed by: (a) subtraction of a 3D data set at the point with the maximum contrast enhancement in the pulmonary arteries and the last baseline data set without contrast media (TR-MRA) and (b) subtraction of the data set with the maximum contrast enhancement in the lung parenchyma and the first baseline data set without contrast media (perfusion-weighted data set) (Fig. 1). For image analysis, the original data as well as multiplanar reformats (MPR) and maximum intensity projections (MIP) were used. MRA studies were assessed to the following criteria: quality of contrast media timing (too early, optimal, too late), overall quality (including breathing artifacts, contrast media timing, folding artifacts; score 1 excellent to 4 not usable). For more quantitative measures, signal intensity measurements were performed in the pulmonary artery, superior vena cava, and ascending aorta. These measures were done on the SR-MRA and TR-MRA as well as on subtraction data sets.
For diagnostic evaluation, the presence or absence of segmental arteries, abnormal proximal to distal tapering, direct visualization of thrombi, vessel wall irregularities, abrupt vessel cut-offs, meandering vessels, presence of bronchial arteries, and number of visible generations of pulmonary arteries was assessed. Perfusion-weighted MRIs were assessed on a segmental basis for normal, complete perfusion defect, subsegmental (= focal) defects, or inhomogeneous perfusion.
Afterward, another blinded read was done by another author not involved in the first evaluation. The reader was to only note the diagnosis of the data set. Datasets were displayed anonymously and shuffled regarding diagnosis and technique. Furthermore, signal time curves in the pulmonary trunk and ascending aorta were assessed using the TR-MRA data sets. The following parameters were calculated: time of first contrast media in the pulmonary trunc, the maximum signal intensity achieved in the pulmonary trunc, and the duration of contrast agent passage defined as difference between the end of signal decrease and the beginning of signal-intensity increase.
Unless specified, data are presented as mean±standard deviation (SD). Due to the small number of patients, statistical analysis was kept to a minimum. If statistical analysis were performed, the Mann-Whitney U test (SPSS for Windows, Version 11.5) was used. A p value <0.05 was considered statistically significant on a local level. Box-plot diagrams were used for data plotting.
Results
All patients and volunteers tolerated the examination well, and all data sets were eligible for evaluation. The quality of contrast media timing of SR-MRA was rated optimal in four cases and too late in one patient with IPAH. In patients with CTEPH, timing was optimal once, and four times it was too late. The overall quality in patients with IPAH was excellent in four and moderate in one case. In patients with CTEPH, the overall quality rating was excellent three times, good once, and moderate once. For TR-MRA, the best data set for optimal contrast media timing was selected retrospectively. Thus, all examinations had excellent timing. The overall image quality was excellent in all patients with IPAH and in four patients with CTEPH. The image of one CTEPH patient had some artifacts and was scored good. For the perfusion-weighted datasets in IPAH patients, four showed an excellent quality and one patient was rated good. In CTEPH, four patients were rated excellent and one patient was rated moderate. All patients were able to hold their breath for the duration of the SR-MRA. Therefore, no severe breathing artifacts were noted. For TR-MRA, only the first datasets were needed for angiography and perfusion.
Signal-to-noise ratio (SNR) values are given in Table 1. For both MRA techniques, there was a higher SNR achieved in patients of group 1 than in group 2. SNR in the pulmonary artery of healthy volunteers (TR-MRA) was comparable to group 1. Group 2 showed a markedly higher SNR.
In patients with IPAH and CTEPH, SR-MRA showed pulmonary arteries down to the fifth bifurcation and down to the fourth bifurcation in TR-MRA. Compared with SR-MRA, less segmental branches were visible with TR-MRA (Table 2). However, no statistically significant difference was found (Fig. 2). The mean number of vascular segments visible was highest in the upper and lower lobes and less high in the middle lobes (Table 2).
The central pulmonary arteries were normal but dilated in patients with IPAH (Fig. 3). Only one patient showed a meandering course of three lobar arteries while the other four showed no abnormalities down to a lobar level. On a segmental level, the predominant finding was a tortuous course of the arteries. All patients with CTEPH showed thrombotic wall adherent material in the central pulmonary arteries down to the lobar level. The predominant findings in patients with CTEPH were wall irregularities (45 findings) and an abnormal proximal-to-distal tapering (28 findings). These abnormalities were not found in patients with IPAH. All results are summarized in Table 3.
Patient suffering from idiopathic pulmonary arterial hypertension (IPAH). a High spatial resolution magnetic resonance angiography (SR-MRA) shows the loss of peripheral pulmonary arteries and the enlargement of the central pulmonary arteries. b Perfusion-weighted image from time-resolved magnetic resonance angiography (TR-MRA) shows no sharp perfusion defects but a diffuse reduction of peripheral, subpleural perfusion. At the same time, the central dilatation of the pulmonary artery (PA) is notable
In TR-MRA, more segments were rated normal compared with the SR-MRA. Consecutively, less pathological changes were found. However, the predominant finding in patients with IPAH was still the tortuous course of the pulmonary arteries. Patients with CTEPH presented most often with wall irregularities and abnormal proximal-to-distal tapering (Table 3) (Fig. 4).
a Example of a high spatial resolution magnetic resonance angiography (SR-MRA) of a patient suffering from chronic thromboembolic pulmonary hypertension (CTEPH) with wall adherent thromboembolic material in the right pulmonary artery (white solid arrow) (maximum intensity projection 15 mm slab thickness). Note also the web in the right upper lobe pulmonary artery (white dotted arrow). b Same patient as in a. This maximum-intensity projection (15 mm slab thickness) is reconstructed from the time-resolved MRA (TR-MRA). It allows for assessment of the same information as the SR-MRA regarding the central parts of the pulmonary arteries and also for the principle peripheral changes (i.e., torturous course)
In SR-MRA, no IPAH patient showed any dilated bronchial arteries while those were present in four patients with CTEPH (range 1–3). Only one focal perfusion defect was found in the group of patients with IPAH while all other findings were summarized as patchy and diffuse reduction in perfusion. All patients with CTEPH showed either segmental or subsegmental perfusion defects. These defects were sharply demarcated (Table 4).
In the second diagnostic read, all diagnosis was right. The characteristic disease patterns were assessed fastest on the perfusion and TR-MRA datasets. On the SR-MRA datasets, it took longer; however, the reader was more confident about diagnosis. All diagnoses based on the different MR evaluations were confirmed by invasive catheterization, V/Q scintigraphy, or CTA. In all patients, no other disease of the chest was found, especially no tumors, lymphadenopathy, or infiltrations.
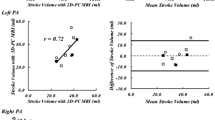
Data for analysis of the contrast media distribution are given in Table 5. Healthy volunteers showed a significantly shorter transit time for the pulmonary arteries than patients with IPAH (14±1 s versus 22±4 s) and CTEPH (25±11 s) (each p=0.01). No difference was found between both patient populations (p=1).
Discussion
Using MRA techniques, it was possible to differentiate between patients with IPAH and CTEPH. While SR-MRA could visualize the pulmonary arteries down to the fifth level, TR-MRA was capable to visualize four generations. However, looking at the abnormalities of the pulmonary vasculature, SR-MRA outperformed TR-MRA. The perfusion-weighted 3D datasets from TR-MRA enabled a fast and reliable differentiation between both disease entities. Analysis of the contrast media characteristics showed only a significant difference between the volunteers and both patient groups. However, no difference was found between either patient group.
Differential diagnosis of PH is becoming increasingly important as new treatment options are available [1]. Additionally, general practitioners become more aware of the disease and there is an increasing request for an easy-to-perform noninvasive diagnostic procedure. For noninvasive assessment of PH, echocardiography is the method of first choice. However, no information can be obtained concerning the pulmonary vasculature. CTA and MRA are two techniques for noninvasive visualization of the pulmonary arteries. Patients presenting with suspected PH are relatively young, and as the disease itself can be referred to as benign, X-ray use should be kept to a minimum. Comparing MRA with invasive pulmonary angiography in patients with CTEPH, Kreitner et al. found an excellent correlation down to the segmental level [10]. One drawback of the SR-MRA techniques is the long breath-hold time. Due to the principle of 3D MRA, the whole dataset will be disturbed even if the patient breathes at the very end of image acquisition [11]. Compared with other studies, we had a similar acquisition time of 23 s and found similar vascular changes [5, 12]. By use of TR-MRA, breathing artifacts can be reduced and patients with severe dyspnea will not get exhausted. Using ultrashort acquisition times, these datasets can also be used for calculation of a perfusion-weighted image [13] with consecutive reduced spatial information. In the present study, we found a good intertechnique agreement for the delineation of IPAH and CTEPH. Using similar MR techniques, a 91% agreement between MRA and digital subtraction angiography (DSA) has been reported [14]. If PH is due to CTEPH, the best therapeutic option is surgical pulmonary thromboendarterectomy (PTE). Surgical planning depends on data about exact localization of the stenosing material and the presence of bronchial arterial collaterals. The presence of bronchial arteries is positively correlated with a better postoperative outcome [15]. SR-MRA has already shown to be capable of evaluating whether the patient is eligible for PTE [10]. In our study, the lobar arteries and the presence of obstructing material could also be detected by TR-MRA. However, the achieved image resolution of TR-MRA was not high enough to visualize bronchial arteries. Therefore, for surgical planning, additional SR-MRA is needed.
MR perfusion techniques were used in some studies for diagnosis of PE [6, 16, 17]. The perfusion patterns resulting from PE were focal defects with sharp margins. This finding was also the leading pattern in patients with CTEPH in our study. The diffuse perfusion pattern observed in patients with IPAH has not been described so far using MR techniques. It was present in all IPAH patients. These characteristic perfusion pattern allowed in the second read for a fast differentiation between the two disease entities. However, these differences in perfusion patterns between both disease entities warrant further studies.
The absolute number of arterial segments visible was highest in the upper lobes. This might be due to the fact that first in the upper lobes respiratory motion is least and the arteries are orientated mostly in the coronal orientation. This increases visualization, as imaging orientation is also coronal. The arteries of the middle lobes were visualized nearly equally as well as the lower lobes and were less than the upper lobes. The two aspects mentioned above might have decreased the quality in the middle lobes, as here the arteries run horizontally. The lower lobes might have experienced decrease in quality by slight respiratory and cardiac motion. Overall, SR-MRA allowed for a better visualization of the number of pulmonary arteries yet without significant influence on diagnostic performance.
The prolonged mean transit time of the contrast media was a good predictor of PH. However, this prolongation did not allow for differentiation between different disease entities. SNR analysis showed some contrast media in the superior vena cava in all patients and techniques. The difference of SNR values in the pulmonary arteries regarding disease technique are an interesting finding. No possible explanation can be encountered for this finding especially as SR-MRA showed a higher SNR in patients with IPAH and TR-MRA showed higher SNR values in patients with CTEPH. This also excludes the influence of vascular obstruction with potential pooling of blood in the central pulmonary arteries. Furthermore, no difference of contrast media passage time was found (Table 5) and all examinations were done using the same contrast media injection protocol.
The major drawback of this study is the limited number of patients. Also, results were not directly correlated to results of conventional imaging techniques. As MRA has already proven to be accurate for evaluation of the pulmonary arteries, at least down to the segmental level, this is not considered a major issue [18].
In conclusion MRA techniques are eligible for differentiation between IPAH and CTEPH. TR-MRA allows for a visualization of the pulmonary arteries down to the segmental level in all cases. Furthermore, perfusion-weighted images allow for easy visualization of the characteristic pattern of the loss of perfusion. For clinical routine, perfusion images are easier to read than the high-resolution angiography datasets. The imaging strategy in suspected PH should start with a perfusion study. If the main findings are segmental perfusion defects, it should be complemented by an SR-MRA to assess eligibility for surgery and to visualize bronchial arteries.
References
Barst RJ, McGoon M, Torbicki A, Sitbon O, Krowka MJ, Olschewski H, Gaine S (2004) Diagnosis and differential assessment of pulmonary arterial hypertension. J Am Coll Cardiol 43:40S–47S
Bouchard A, Higgins CB, Byrd BF III, Amparo EG, Osaki L, Axelrod R (1985) Magnetic resonance imaging in pulmonary arterial hypertension. Am J Cardiol 56:938–942
van Beek EJ, Wild JM, Fink C, Moody AR, Kauczor HU, Oudkerk M (2003) MRI for the diagnosis of pulmonary embolism. J Magn Reson Imaging 18:627–640
Ley S, Kauczor HU, Heussel CP, Kramm T, Mayer E, Thelen M, Kreitner KF (2003) Value of contrast-enhanced MR angiography and helical CT angiography in chronic thromboembolic pulmonary hypertension. Eur Radiol 13:2365–2371
Bergin CJ, Hauschildt J, Rios G, Belezzuoli EV, Huynh T, Channick RN (1997) Accuracy of MR angiography compared with radionuclide scanning in identifying the cause of pulmonary arterial hypertension. Am J Roentgenol 168:1549–1555
Fink C, Ley S, Puderbach M, Plathow C, Bock M, Kauczor HU (2004) 3D pulmonary perfusion MRI and MR angiography of pulmonary embolism in pigs after a single injection of a blood pool MR contrast agent. Eur Radiol 14:1291–1296
Fink C, Risse F, Buhmann R, Ley S, Meyer FJ, Plathow C, Puderbach M, Kauczor HU (2004) Quantitative analysis of pulmonary perfusion using time-resolved parallel 3D MRI-initial results. Fortschr Röntgenstr 176:170–174
Shors SM, Cotts WG, Pavlovic-Surjancev B, Francois CJ, Gheorghiade M, Finn JP (2003) Heart failure: evaluation of cardiopulmonary transit times with time-resolved MR angiography. Radiology 229:743–748
Fink C, Bock M, Kroeker R, Requardt M, Ley S, Kauczor H-U (2004) Contrast-enhanced MRA with elliptic-centric view ordering and view sharing: theoretical considerations and application in patients with cardiopulmonary disease. Proc Int Soc Mag Reson Med 11:6
Kreitner KF, Ley S, Kauczor HU, Mayer E, Kramm T, Pitton MB, Krummenauer F, Thelen M (2004) Chronic thromboembolic pulmonary hypertension: pre- and postoperative assessment with breath-hold MR imaging techniques. Radiology 232:535–543
Goyen M, Ruehm SG, Debatin JF (2000) MR-angiography the role of contrast agents. Eur J Radiol 34:247–256
Kreitner K-F, Ley S, Kauczor H-U, Kalden P, Pitton MB, Mayer E, Laub G, Thelen M (2000) Assessment of chronic thromboembolic pulmonary hypertension by three-dimensional contrast-enhanced MR angiography-comparison with selective intraarterial DSA. Fortschr Röntgenstr 172:1–6
Fink C, Bock M, Puderbach M, Schmähl A, Delorme S (2003) Partially parallel three-dimensional magnetic resonance imaging for the assessment of lung perfusion-initial results. Invest Radiol 38:482–488
Nikolaou K, Schoenberg S, Attenberger U, Nittka M, Behr J, Reiser M (2003) High-resolution MRA and fast perfusion imaging using integrated parallel acquisition techniques (iPAT) in the diagnosis of pulmonary arterial hypertension. Proc Int Soc Mag Reson Med 11:1370
Kauczor H-U, Schwickert HC, Mayer E, Schweden F, Schild HH, Thelen M (1994) Spiral CT of bronchial arteries in chronic thromboembolism. J Comput Assist Tomogr 18:855–861
Torheim G, Amundsen T, Rinck PA, Haraldseth O, Sebastiani G (2001) Analysis of contrast-enhanced dynamic MR images of the lung. J Magn Reson Imaging 13:577–587
Zheng J, Leawoods JC, Nolte M, Yablonskiy DA, Woodard PK, Laub G, Gropler RJ, Conradi MS (2002) Combined MR proton lung perfusion/angiography and helium ventilation: potential for detecting pulmonary emboli and ventilation defects. Magn Reson Med 47:433–438
Oudkerk M, van Beek EJ, Wielopolski P, van Ooijen PM, Brouwers-Kuyper EM, Bongaerts AH, Berghout A (2002) Comparison of contrast-enhanced magnetic resonance angiography and conventional pulmonary angiography for the diagnosis of pulmonary embolism: a prospective study. Lancet 359:1643–1647
Acknowledgements
The authors acknowledge the valuable help of S. Yubai and K. Knauer in performing the examinations. This work was supported by the Deutsche Forschungsgemeinschaft (Grant FOR 474).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ley, S., Fink, C., Zaporozhan, J. et al. Value of high spatial and high temporal resolution magnetic resonance angiography for differentiation between idiopathic and thromboembolic pulmonary hypertension: initial results. Eur Radiol 15, 2256–2263 (2005). https://doi.org/10.1007/s00330-005-2792-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-005-2792-z