Abstract
Transrectal ultrasound (TRUS) is an important tool for urologists and radiologists in the detection of prostate cancer. Various TRUS-guided biopsy techniques are applied in clinical practice. Frequently, only the detection rates achieved with these methods are compared. Other diagnostic performance parameters, particularly the specificity and negative predictive value, are seldom compared. After extensive assessment of the available literature, this review describes the methods of TRUS-guided biopsy for prostate cancer detection. A distinction was made between systematic biopsies and biopsies that target a perceived (hypoechoic or Doppler-enhancing) lesion on imaging. Subsequently, the diagnostic performance (sensitivity, specificity, positive and negative predictive values, accuracies) was compared between these techniques. Imaging-guided biopsy showed better diagnostic performance than systematic biopsy with higher sensitivity. The combinations of sensitivity and specificity were highest for colour Doppler and contrast-enhanced targeted biopsy. Studies targeting hypoechoic lesions had relatively high sensitivity, but specificity was low. Presently however, with widespread prostate-specific antigen screening, fewer prostate cancers are hypoechoic, and the value of targeting hypoechoic lesions has diminished. Performing colour or contrast-enhanced Doppler biopsy or adding these techniques to systematic biopsies improves diagnostic performance, particularly by increasing sensitivity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Measured by the annual number of new cases, prostate cancer is the sixth most common cancer in the world. Presently, it represents up to one-third of all new male cancers in developed countries [1]. Incidence rates vary from 1.9/100,000 per year in Asian men to 137/100,000 per year in African-American men [2–5]. Prostate cancer mortality ranges from 25–40/100,000 men [3, 6, 7]. Up to 86% of the currently detected prostate cancers are amenable to curative treatment [8]. This underscores the need for accurate early detection of prostate cancer, although "insignificant" cancers [9], that is, prostate cancers from which the patient would never have died, are also detected.
Transrectal ultrasound (TRUS) was introduced as a diagnostic device for prostate cancer in 1968. It became the most important tool for diagnosing prostate cancer by guiding prostate biopsies [10, 11]. Because the prostate-specific antigen (PSA) test used to screen for prostate cancer is neither 100% sensitive nor specific [12], TRUS-guided biopsy is essential to detect true-positives until a better biomarker is discovered.
Although there is no discussion about the usefulness of biopsies in prostate cancer detection, there is extensive debate about which biopsy scheme to use. This has resulted in institutional protocols that differ as to the number and location of biopsies per session, as well as the imaging technique used to guide the biopsy.
Most comparative studies have analysed detection rates (i.e. the number of prostate cancer cases found, divided by the total number of patients who underwent the examination) of the various biopsy techniques. However, the diagnostic performance parameters—sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), overall accuracy, and diagnostic odds ratio (DOR)–of these techniques have seldom been evaluated. An advantage of the specificity and NPV parameters is that, contrary to the detection rate or sensitivity, patients in whom no cancer was detected are also analysed. What will matter to an individual patient is the answer to the question, "What is the probability that I have prostate cancer given a negative biopsy result?" In order to address this topic, a clinician needs to know the NPV of the biopsy, which is directly dependent on the sensitivity. Likewise, a patient with an elevated PSA level will want to have the test with the highest likelihood of detecting a cancer: hence, the test with the highest sensitivity.
The purpose of this review is to describe the various techniques of TRUS-guided prostate biopsy that are currently applied in uro(radio)logical practice and to compare the diagnostic performance of systematic biopsy with imaging-guided techniques such as gray-scale, colour, and power Doppler as well as contrast-enhanced imaging.
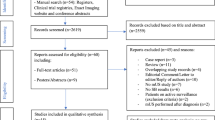
Literature search and methodology
To retrieve literature regarding the diagnostic performance of TRUS-guided prostate biopsy, a Medline search was performed using the medical subject heading terms "prostatic-neoplasms,” “ultrasonography-,”, “biopsy-,” “sensitivity-and-specificity,” and “predictive-value-of-tests.” Additionally, a free search was carried out, combining the terms “prost*,”, “stag*,” “sext*,” “hypoech*,” “biops*,” “ultrason*,” “Doppler,” and “contrast*”.
Only original articles were included for analysis. Exclusion criteria were (1) studies that examined a population of fewer than 100 patients, unless there were too few (<10) studies that encompassed this number of patients, (2) the use of transperineal biopsy protocols, since most uro(radio)logical clinics presently perform biopsies transrectally, (3) publication prior to the year 1993, in order to obtain a more homogeneous level of technological advancement, and (4) absence of all necessary data for the calculation of diagnostic performance.
The diagnostic performance parameters that were extracted were sensitivity, specificity, PPV, NPV, overall accuracy, and DOR. For an in-depth explanation of these parameters, the authors refer the reader to earlier publications [13, 14]. These and other characteristics of the included studies are shown in Tables 1, 2, 3, and 4.
Techniques to guide and direct biopsy
Targeting of hypoechoic lesions
Gray-scale imaging allows for an excellent anatomical delineation of the prostate gland in relation to the surrounding fat tissue, rectum, neurovascular bundles, and venous plexus, as well as a clear division between the inner gland (transition and central zone) and outer gland (peripheral zone) of the prostate.
In the early 1980s, hypoechoic nodules were seen as the main presentation of prostate cancer, and solely these nodules were targeted at biopsy. The hypoechoic appearance is believed to be due to the increased microvessel density [15]. However, up to 30% of all prostate cancers are isoechoic [16, 17], and it is estimated that a hypoechoic nodule has a 17–57% chance of being identified as prostate cancer [18]. Presently, in the PSA era, this percentage is reported to be as low as 9% [19].
Systematic biopsy protocols
In 1989, Hodge et al. coined the sextant biopsy method that is still the standard of reference in prostate cancer detection [20]. The prostate is bilaterally divided into three regions (apex, midgland, and base), all of which are systematically biopsied once. Many physicians take additional bilateral transition zone biopsies.
Initially, it was reported that extending the number of biopsy cores resulted in higher detection rates and that the additionally found cancers had implications for patient prognosis [21–24]. Hence, a systematic standard biopsy session may encompass any number of biopsy cores, with 10–12 currently being used most frequently [25, 26]. The location of the biopsies is also an important determinant of cancer detection [27]. For instance, the addition of six more lateral biopsies to the systematic protocol increased the detection rate from 31% to 43% [28, 29]. A number of studies have reported that expanding the number of cores does not necessarily increase prostate cancer detection [27, 30–34].
The systematic biopsy method differs from the imaging-based techniques that target hypoechoic or Doppler-enhancing lesion because it does not target lesions suspicious for TRUS but has standard locations from which biopsies are taken.
Doppler-targeted biopsy protocols
Prostate cancer tends to have increased vascularity compared with healthy prostatic tissue due to the formation of new vessels or an increase in the capacity of existing vessels [35, 36]. Also, cancer foci with higher Gleason scores have higher degrees of vascularity [37]. Because this higher degree of vascularity was reported to be correlated with a worse survival rate, the vascularity of a prostate cancer focus is an important diagnostic feature, particularly for outer gland cancers [15, 38–40].
Colour Doppler imaging measures blood flow velocity and direction. Power Doppler imaging is able to visualise smaller vessels and vessels with lower flow velocity than is the case with colour Doppler because it uses the Doppler signal amplitude instead of the velocity or direction of the flow [41, 42].
Published Doppler criteria used for tumour localisation have varied. Criteria used most often were the presence of hypervascularity, a high degree of flow, left-right asymmetry, and mass effect changes (a gap in perfusion around the lesion due to the compression of vessels by the pressure of the tumour mass) on the vessel structures [43–46]. Furthermore, Rifkin et al. categorised three flow patterns that were a sign of prostate cancer: increased flow within a lesion, increased flow surrounding a lesion, and asymmetric flow in comparison to adjacent tissue or contralateral areas [47].
Contrast-enhanced Doppler-targeted biopsy
The difference in acoustic impedance between the contrast agent (microbubbles) and adjacent tissue results in higher reflective interfaces. Because the microbubbles remain intravascular, they act as a blood pool agent [48, 49]. Therefore, these substances are optimally suited for real-time visualisation of the vasculature.
While the first-generation contrast agents were manufactured for use with probes that had a high power output (referred to as the mechanical index, MI [50], a function of ultrasound wave pressure and probe frequency), the second-generation agents are best applied at low MIs. Recent TRUS probes have been able to switch to low MIs (<0.3) to preserve these microbubbles. Important factors that influenced vessel visualisation were the level of blood flow and the amount of clustering of vessels [51].
Comparison of diagnostic performance between biopsy protocols
The essential question is whether imaging-guided biopsies into hypoechoic or Doppler-enhancing lesions, with or without contrast agent application, have better diagnostic performance compared with systematic standard biopsy protocols.
Systematic biopsy protocols (Fig. 1, Table 1)
Included studies
Only two studies met all inclusion criteria. These studies used radical prostatectomy as standard of reference, and biopsy results were analysed on a core-by-core basis.
Analysis of diagnostic performance
Sensitivity was low (39–52%) while specificity was relatively high (81–82%), resulting in high PPVs (83–84%) and low NPVs (36–48%; Table 1).
Discussion
It is theoretically not possible to determine the diagnostic performance of a systematic standard biopsy protocol unless (1) the performer or interpreter gives a subjective interpretation of suspiciousness to every site from which a core is taken, or (2) radical prostatectomy specimens are used as standard of reference. In the latter case, the problem of true-negativity and false-positivity arises. Patients whose biopsies are all negative will not undergo prostatectomy; therefore, the number of true-negatives (on a patient basis) cannot be determined. One exception is the study by Terris [52], who examined the diagnostic accuracy of sextant biopsy in men who underwent cystoprostatectomy for bladder-related diseases. In these patients, whose PSA level ranged from 0.2 to 10 ng/ml, a sensitivity and specificity of 60% and 100%, respectively, were reported (see Table 1). However, because the patient population is markedly different from that in regular systematic biopsy studies, the results are difficult to compare. Studies using prostatectomy as standard of reference defined false-positivity as an absence of prostate cancer at the site at which the biopsy was reported to be positive.
A limitation of the analysis was the fact that a number of studies were excluded because they did not use radical prostatectomy as standard of reference or because the diagnostic performance parameters could not be calculated [43, 45, 46, 53–55]. In a number of the excluded systematic biopsy studies, certain cores taken at systematic biopsy were replaced by targeted biopsies if a suspicious area was close to that systematic biopsy site [56–60]. Thus, many studies represented a mix of systematic standard and hypoechoic lesion-targeted biopsies.
Targeting hypoechoic lesions (Fig. 1, Table 2)
Included studies
Of the 10 included studies, nine used both targeted biopsies and sextant biopsies as standard of reference. One study [53] used only systematic standard biopsy. Most studies analysed diagnostic performance on a patient-by-patient basis; three studies used a core-by-core or per-lobe analysis.
Analysis of diagnostic performance
The 10 studies can be grouped into a “high-specificity group” of five studies (sensitivity: 35–60%, specificity: 72–82%) and a "high-sensitivity group" of five studies (sensitivity 84–96%, specificity 23–58%).
Discussion
Patient inclusion criteria did not differ between these two groups, and patient characteristics (PSA levels, Gleason scores) were reported in only two studies. No difference in the number of cores taken was found. Also, the average year of publication did not differ. The high-specificity group consisted predominantly (4/5) of studies conducted in North America, while three out of five studies of the high-sensitivity group were performed in Europe. An explanation may be that in the North American studies, more patients were identified through population screening [61], and the racial composition of the populations may have differed. The low sensitivity found in the study by Flanigan et al. [53] may be explained by the fact that no targeted biopsies were performed and that only the appearance of a prostate quadrant was analysed.
Comparing the combinations of sensitivity and specificity in a receiver operating characteristic (ROC) curve figure (Fig. 1), if one generated a line fitted from these combinations of sensitivity and specificity, all studies would lie close to this line. The little scattering suggests that this method has low interobserver variability and is relatively independent of technical and operator-dependent settings.
The generally low PPVs, while also strongly dependent on the prevalence of prostate cancer, are partly explained by the fact that other disease processes, such as prostatic intraepithelial neoplasia and prostatitis, can also present themselves as hypoechoic nodules. This causes false-positives [62].
A limitation of this method of biopsy is that it leaves isoechoic or hyperechoic lesions undiagnosed, as these are not targeted.
Colour and power Doppler-guided biopsy protocols (Fig. 1, Table 3)
Included studies
A total of eight colour Doppler and six power Doppler studies were included. Targeted biopsies as well as systematic biopsies were the standards of reference for all studies. Some studies analysed results on a core-by-core basis, whereas other studies analysed results on a patient-by-patient basis.
Analysis of diagnostic performance
While sensitivity ranges for both colour and power Doppler were wide (43–87% and 17–92%, respectively), colour Doppler generally achieved higher sensitivity. Specificities did not vary markedly between the two types of Doppler imaging (Table 3).
Discussion
The higher sensitivity of colour Doppler compared with power Doppler contrasts a previous report by Halpern et al. [63], who found sensitivity/specificity pairs of 15%/95% and 31%/74% for colour and power Doppler-guided biopsy, respectively. In another study, they determined that there was no significant difference in the area under the ROC curve between these techniques [46].
Compared with studies targeting hypoechoic lesions, the results for Doppler targeted biopsy have a wider spread (Figs. 1 and 2). This reflects the larger interobserver variability and operator-dependency of this technique. Furthermore, Doppler ultrasound quality is highly dependent on the ultrasound machine that is used [64], the probe frequency, probe settings such as gain, repetition frequency, power output, and filter settings [65]. These settings are, however, seldom mentioned in clinical publications. Also, correct interpretation of Doppler images is reported to have a gradual learning curve [63].
Another reason for the scattering of results may be the high incidence of artefacts. First, stable blood flow imaging may be hindered by visceral motion or patient or probe movement [66, 67]. Second, the use of a high-frequency probe for increased resolution in the near-field decreases Doppler reception of the ventral part of the prostate, resulting in false-negative results. Furthermore, patient position can give rise to both false-negative and false-positive results; increased vascularity has been observed in the part of the prostate that the patient was lying on [68]. Also, blood flow can be too slow for Doppler imaging to detect, causing false-negative results [69].
Diagnostic performance may also be influenced by the specialist (urologist or radiologist) who performs the examination, as well as his or her experience [63]. Because most Doppler studies were published by radiologists, it is not yet clear what the diagnostic performance would be if urologists were to perform the Doppler examination.
Last, contrary to the sole criterion used in targeting hypoechoic lesions, in Doppler studies a wider array of definitions of suspicious areas is used (see section “Doppler-targeted biopsy protocols”).
Among the eight included colour Doppler-guided biopsy studies, two had low specificity with high sensitivity. In 1993, Rifkin et al. [70] reported a high (280/619) number of false-positive cases that had benign prostatic disease on biopsy, and in retrospect, all noncancerous lesions had some form of abnormal flow. Only three out of every 10 areas with increased colour Doppler flow were proven to be prostate cancer. Lavoipierre et al. [71] even had more false-positive than true-positive cases, achieving a sensitivity and PPV of 76% and 44%, respectively.
Three power Doppler studies [63, 67, 72] reported both low sensitivity and specificity. Further examination of the patient groups revealed that the average PSA level of patients was distinctly lower compared with that of patients in the other power Doppler studies. This underscores the difficulty of comparing studies, as prostate cancer is likely to be larger and more vascularised at higher levels of PSA and is therefore more easily detectable.
Generally, the most recently (2003–2004) published power Doppler studies achieved both higher sensitivities and specificities, possibly indicating an advancement in Doppler technology.
Contrast-enhanced targeted biopsy protocols (Fig. 1, Table 4)
Included studies
Six of the eight included studies used direct contrast-enhanced targeted biopsy as well as systematic standard biopsy as standard of reference. One study performed only systematic standard biopsy, while one performed only targeted biopsy.
Analysis of diagnostic performance
The included studies that used contrast-enhancement to target the biopsy can be split into two groups: a group of two studies [44, 73] that had excellent results and a main group (six studies) with "average" results. Sensitivity and specificity were 40–94% and 40–88%, respectively (Table 4).
Discussion
Only two studies have examined more than 100 patients. Frauscher et al. [74] used Levovist in 230 patients and found a sensitivity of 81% with a specificity of 46% on a patient-by-patient analysis. Pelzer et al. [75] used Sonovue in 380 patients for detection and reported a sensitivity and specificity of 48% and 71%, respectively, on a core-by-core basis.
The earliest included study, by Ragde et al. [76], had the poorest results, with both a sensitivity and specificity of 40%. However, the investigators examined only 15 patients, the transducer used in this study was not able to directly target contrast-enhancing lesions, and biopsy had to be performed with another transducer by gray-scale guidance. This may explain the poor performance.
In 85 patients, Roy et al. found that contrast-enhanced Doppler detected 20% more isoechoic lesions in the peripheral zone than conventional Doppler did [44]. An advantage of contrast-enhanced biopsy is that the mean Gleason score detected was significantly higher than that detected by systematic standard biopsy [74, 75].
Results of contrast-enhanced targeted biopsy appeared to be less scattered than Doppler imaging (Fig. 2). This may reflect a smaller influence of operator-dependent parameter settings due to the fact that the contrast agent increases the visibility of the vasculature at basic imaging settings (i.e. it increases the signal-to-noise ratio). Nevertheless, machine settings for signal reception should be optimised in accordance with the contrast agent used.
A limitation of the current analysis is that only two studies [74, 75] with large patient populations have been performed. More extensive biopsy studies, conducted not only in the centres of excellence that pioneered the method, are needed to evaluate the accuracy of the contrast-enhanced technique.
Discussion of overall practice and future prospects
Biopsies that are targeted based on an imaging abnormality, either hypoechoic or Doppler-enhancing lesions, were generally found to have higher sensitivity compared with systematic biopsies. The various imaging techniques differed slightly with respect to sensitivity and specificity. In general, colour Doppler and contrast-enhanced targeted biopsy have the highest combination of sensitivity and specificity.
In the practice of systematic biopsies, the trend has been to increase the number of biopsy cores taken per session. Another advancement has been to retrospectively analyse the biopsy process by means of three-dimensional computer simulation to determine the optimal combination and localisation of systematic biopsies for cancer detection [77–79].
We had to exclude a number of studies using systematic biopsy because we were unable to calculate the diagnostic performance parameters from the data or because the study did not use radical prostatectomy as standard of reference. Additionally, some studies adjusted the systematic biopsy protocol if abnormalities were seen on TRUS and, thereby, mixed targeted biopsies with systematic biopsies. Thus, the subsequent inclusion of only two studies that performed systematic biopsy into our review is a limitation. Nevertheless, the patient populations in these two studies represented more than 200 patients.
Most studies that examined the diagnostic performance of targeting hypoechoic lesions were performed at least 7 years ago. Since then, PSA-based screening has spread, and the PSA threshold for performing biopsy has decreased, resulting in earlier detection. Because of this earlier detection, the pathognomonic feature of the hypoechoic lesion as a sign of prostate cancer has decreased in value. This is supported by a recent study that reported that only 9.3% of hypoechoic nodules in the PSA era contained prostate cancer, compared with 10.4% of isoechoic prostate areas that were targeted [19]. Thus, currently targeting only hypoechoic areas is insufficient to detect prostate cancer.
In Doppler-guided biopsy it appears that the observance of flow in a prostatic area is in itself an insufficient criterion for biopsy of that area due to the high percentage of false-positives. It would therefore be advisable to include other vascular characteristics, such as the appearance of the vessels (concentricity, contortion, pathways, and size of the vessels), in determining whether to perform a biopsy at a site.
An important consideration is the dependency of imaging techniques on the underlying gray-scale image. In clinical practice, Doppler is always performed on top of the gray-scale image, and, therefore, the decision to target a lesion suspicious on Doppler may also include abnormalities on gray-scale (abnormal echogenicity). Although this can artificially enhance the theoretical diagnostic performance of the Doppler studies, it is a reflection of regular clinical practice.
Contrast-enhanced biopsy increased the sensitivity of unenhanced Doppler examinations. Figure 3 shows an example of a prostate cancer focus being visible only after contrast administration. Its main advantage is the increase in the signal-to-noise ratio of the vasculature. This ratio can be increased further by applying contrast-agent-specific techniques, such as harmonic imaging [80, 81] and intermittent scanning [60]. For instance, Halpern et al. [82], in the only study performing intermittent scanning in prostate cancer, reported that several prostate cancers could only be visualised by this technique. Therefore, contrast-enhanced TRUS is currently the most promising biopsy guidance technique.
Example of the additive value of contrast-enhanced transrectal ultrasound in prostate cancer localization. A 64-year-old man with biopsy-proven, clinically localised prostate cancer (PSA 6.9 ng/ml, Gleason score 3+3, and organ-confined disease on digital rectal examination) underwent a preoperative transrectal ultrasound examination (Viking, Bruel & Kjaer, Denmark) 3 days prior to laparoscopic radical prostatectomy. In the radical prostatectomy specimen (a), the prostate cancer (Gleason 3+4, stage T2c) was predominantly located in the apex on the left side (outlined in blue). On gray-scale imaging (b), no abnormality could be detected. On colour Doppler (c) and power Doppler (d) imaging, no hypervascularity was discernible. During slow infusion of 2.4 ml of SonoVue (sulfur hexafluoride, Bracco, Milan, Italy) at 1 ml/min with a low (<0.3) mechanical index (e), a large hypervascular area (arrows) suspicious for prostate cancer became apparent. Note the concentrically oriented vessels
Furthermore, these new techniques may aid in detecting isoechoic as well as transition zone prostate cancers [44]. Transition zone prostate cancers often show no clear abnormalities on conventional Doppler imaging, partly due to their further distance from the probe. Because transition zone prostate cancer also displays increased vascularity after contrast administration, these tumours may be more susceptible to detection by means of contrast agent administration. Nevertheless, the false-positive rate is still high due to prostate cancer-like enhancement of benign prostatic hyperplasia and prostatitis [18, 60, 82].
While biopsy by means of magnetic resonance (MR) imaging has long been considered too difficult, time-consuming, and costly, recent reports have demonstrated the feasibility of MR imaging to perform prostate biopsy. Zangos et al. carried out transgluteal prostate biopsies targeted to suspicious lesions in an intervention MR scanner [83] in a limited number of patients (n=25) and were able to detect prostate cancer in 10 of these patients. Beyersdorff et al. [84] showed that transrectal MR-guided biopsy in a closed MR unit was also feasible. In five of the 12 patients, prostate cancer was detected with a mean procedure duration of 55 min. In both studies, complication rates were very low. More and larger studies need to be performed to determine the value of MR-guided biopsy in regular clinical practice. The addition of dynamic contrast-enhanced or MR spectroscopic imaging may further enhance detection rates. Even though the high costs and time consumption preclude the application of MR-guided biopsy to a large patient population, MR imaging may play a definite role after previous TRUS-guided biopsies have failed to detect cancer in patients at risk for prostate cancer.
Conclusions
Application of a TRUS-guided biopsy technique that targets a visual lesion increases the sensitivity of prostate cancer biopsy compared with systematic biopsy. Colour Doppler and contrast-enhanced Doppler targeted biopsy have the best diagnostic performance. Targeting hypoechoic lesions achieves high sensitivity but has low specificity. Therefore, this technique should not be used as sole biopsy guidance. Furthermore, the hypoechoic lesion is becoming less pathognomonic in the PSA screening era. With near-future innovations in contrast-enhanced ultrasound the diagnostic performance of contrast-enhanced guided biopsy can be further improved. Also, the targeting of lesions that enhance after contrast administration detects more aggressive cancers. Hence, application of a contrast agent for biopsy is recommended in order to increase both the yield of the biopsy and the detection of more aggressive cancer foci and to decrease the number of biopsy cores necessary.
References
Jemal A, Murray T, Ward E et al (2005) Cancer statistics, 2005. CA Cancer J Clin 55:10–30
Quinn M, Babb P (2002) Patterns and trends in prostate cancer incidence, survival, prevalence and mortality. Part II: individual countries. BJU Int 90:174–184
Quinn M, Babb P (2002) Patterns and trends in prostate cancer incidence, survival, prevalence and mortality. Part I: international comparisons. BJU Int 90:162–173
Crawford ED (2003) Epidemiology of prostate cancer. Urology 62:3–12
Gronberg H (2003) Prostate cancer epidemiology. Lancet 361:859–864
Levi F, Lucchini F, Negri E, Boyle P, La Vecchia C (2003) Mortality from major cancer sites in the European Union, 1955–1998. Ann Oncol 14:490–495
Stewart SL, King JB, Thompson TD, Friedman C, Wingo PA (2004) Cancer mortality surveillance—United States, 1990–2000. MMWR Surveill Summ 53:1–108
Jemal A, Tiwari RC, Murray T et al (2004) Cancer statistics, 2004. CA Cancer J Clin 54:8–29
Augustin H, Hammerer PG, Graefen M et al (2003) Insignificant prostate cancer in radical prostatectomy specimen: time trends and preoperative prediction. Eur Urol 43:455–460
Watanabe H, Kato H, Kato T, Morita M, Tanaka M (1968) Diagnostic application of ultrasonotomography to the prostate. Nippon Hinyokika Gakkai Zasshi 59:273–279
Watanabe H (1989) History and applications of transrectal sonography of the prostate. Urol Clin North Am 16:617–622
Hernandez J, Thompson IM (2004) Prostate-specific antigen: a review of the validation of the most commonly used cancer biomarker. Cancer 101:894–904
Glas AS, Lijmer JG, Prins MH, Bonsel GJ, Bossuyt PM (2003) The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol 56:1129–1135
Langlotz CP (2003) Fundamental measures of diagnostic examination performance: usefulness for clinical decision making and research. Radiology 228:3–9
Strohmeyer D, Rossing C, Strauss F, Bauerfeind A, Kaufmann O, Loening S (2000) Tumor angiogenesis is associated with progression after radical prostatectomy in pT2/pT3 prostate cancer. Prostate 42:26–33
Dahnert WF, Hamper UM, Eggleston JC, Walsh PC, Sanders RC (1986) Prostatic evaluation by transrectal sonography with histopathologic correlation: the echopenic appearance of early carcinoma. Radiology 158:97–102
Salo JO, Rannikko S, Makinen J, Lehtonen T (1987) Echogenic structure of prostatic cancer imaged on radical prostatectomy specimens. Prostate 10:1–9
Frauscher F, Klauser A, Berger AP et al (2003) The value of ultrasound (US) in the diagnosis of prostate cancer. Radiologe 43:455–463
Onur R, Littrup PJ, Pontes JE, Bianco FJ Jr (2004) Contemporary impact of transrectal ultrasound lesions for prostate cancer detection. J Urol 172:512–514
Hodge KK, McNeal JE, Terris MK, Stamey TA (1989) Random systematic versus directed ultrasound guided transrectal core biopsies of the prostate. J Urol 142:71–74
Taylor JA, III, Gancarczyk KJ, Fant GV, McLeod DG (2002) Increasing the number of core samples taken at prostate needle biopsy enhances the detection of clinically significant prostate cancer. Urology 60:841–845
Eskicorapci SY, Baydar DE, Akbal C et al (2004) An extended 10-core transrectal ultrasonography guided prostate biopsy protocol improves the detection of prostate cancer. Eur Urol 45:444–448
Singh H, Canto EI, Shariat SF et al (2004) Improved detection of clinically significant, curable prostate cancer with systematic 12-core biopsy. J Urol 171:1089–1092
Mariappan P, Chong WL, Sundram M, Mohamed SR (2004) Increasing prostate biopsy cores based on volume vs the sextant biopsy: a prospective randomized controlled clinical study on cancer detection rates and morbidity. BJU Int 94:307–310
Matlaga BR, Eskew LA, McCullough DL (2003) Prostate biopsy: indications and technique. J Urol 169:12–19
Presti JC Jr (2003) Prostate biopsy: how many cores are enough? Urol Oncol 21:135–140
Fink KG, Hutarew G, Pytel A et al (2003) One 10-core prostate biopsy is superior to two sets of sextant prostate biopsies. BJU Int 92:385–388
Gore JL, Shariat SF, Miles BJ et al (2001) Optimal combinations of systematic sextant and laterally directed biopsies for the detection of prostate cancer. J Urol 165:1554–1559
Naya Y, Ochiai A, Troncoso P, Babaian RJ (2004) A comparison of extended biopsy and sextant biopsy schemes for predicting the pathological stage of prostate cancer. J Urol 171:2203–2208
Ravery V, Billebaud T, Toublanc M et al (1999) Diagnostic value of ten systematic TRUS-guided prostate biopsies. Eur Urol 35:298–303
Babaian RJ, Toi A, Kamoi K et al (2000) A comparative analysis of sextant and an extended 11-core multisite directed biopsy strategy. J Urol 163:152–157
Naughton CK, Miller DC, Mager DE, Ornstein DK, Catalona WJ (2000) A prospective randomized trial comparing 6 versus 12 prostate biopsy cores: impact on cancer detection. J Urol 164:388–392
Chan TY, Chan DY, Stutzman KL, Epstein JI (2001) Does increased needle biopsy sampling of the prostate detect a higher number of potentially insignificant tumors? J Urol 166:2181–2184
O’Connell MJ, Smith CS, Fitzpatrick PE et al (2004) Transrectal ultrasound-guided biopsy of the prostate gland: value of 12 versus 6 cores. Abdom Imaging 29:132–136
Bigler SA, Deering RE, Brawer MK (1993) Comparison of microscopic vascularity in benign and malignant prostate tissue. Hum Pathol 24:220–226
Neumaier CE, Martinoli C, Derchi LE, Silvestri E, Rosenberg I (1995) Normal prostate gland: examination with color Doppler US. Radiology 196:453–457
Wilson NM, Masoud AM, Barsoum HB, Refaat MM, Moustafa MI, Kamal TA (2004) Correlation of power Doppler with microvessel density in assessing prostate needle biopsy. Clin Radiol 59:946–950
Ismail M, Petersen RO, Alexander AA, Newschaffer C, Gomella LG (1997) Color Doppler imaging in predicting the biologic behavior of prostate cancer: correlation with disease-free survival. Urology 50:906–912
Erbersdobler A, Fritz H, Schnoger S et al (2002) Tumour grade, proliferation, apoptosis, microvessel density, p53, and bcl-2 in prostate cancers: differences between tumours located in the transition zone and in the peripheral zone. Eur Urol 41:40–46
Bostwick DG, Iczkowski KA (1998) Microvessel density in prostate cancer: prognostic and therapeutic utility. Semin Urol Oncol 16:118–123
Rubin JM, Adler RS (1993) Power Doppler expands standard color capability. Diagn Imaging (San Franc) 15:66–69
Leventis AK, Shariat SF, Utsunomiya T, Slawin KM (2001) Characteristics of normal prostate vascular anatomy as displayed by power Doppler. Prostate 46:281–288
Sauvain JL, Palascak P, Bourscheid D et al (2003) Value of power Doppler and 3D vascular sonography as a method for diagnosis and staging of prostate cancer. Eur Urol 44:21–30
Roy C, Buy X, Lang H, Saussine C, Jacqmin D (2003) Contrast enhanced color Doppler endorectal sonography of prostate: efficiency for detecting peripheral zone tumors and role for biopsy procedure. J Urol 170:69–72
Kuligowska E, Barish MA, Fenlon HM, Blake M (2001) Predictors of prostate carcinoma: accuracy of gray-scale and color Doppler US and serum markers. Radiology 220:757–764
Halpern EJ, Frauscher F, Strup SE, Nazarian LN, O’Kane P, Gomella LG (2002) Prostate: high-frequency Doppler US imaging for cancer detection. Radiology 225:71–77
Rifkin MD, Alexander AA, Helinek TG, Merton DA (1991) Color Doppler as an adjunct to prostate ultrasound. Scand J Urol Nephrol Suppl 137:85–89
Jakobsen JA, Correas JM (2001) Ultrasound contrast agents and their use in urogenital radiology: status and prospects. Eur Radiol 11:2082–2091
Cosgrove D (2004) The advances are significant improvements in both the microbubbles used as contrast agents and in the software that allows their selective detection. Eur Radiol 14 Suppl 8:1–3
Abbott JG (1999) Rationale and derivation of MI and TI-a review. Ultrasound Med Biol 25:431–441
Delorme S, Peschke P, Zuna I, van Kaick G (1999) Sensitivity of color Doppler sonography: an experimental approach. Ultrasound Med Biol 25:541–547
Terris MK (1999) Sensitivity and specificity of sextant biopsies in the detection of prostate cancer: preliminary report. Urology 54:486–489
Flanigan RC, Catalona WJ, Richie JP et al (1994) Accuracy of digital rectal examination and transrectal ultrasonography in localizing prostate cancer. J Urol 152:1506–1509
Hammerer P, Huland H (1994) Systematic sextant biopsies in 651 patients referred for prostate evaluation. J Urol 151:99–102
Newman JS, Bree RL, Rubin JM (1995) Prostate cancer: diagnosis with color Doppler sonography with histologic correlation of each biopsy site. Radiology 195:86–90
Slonim SM, Cuttino JT Jr, Johnson CJ et al (1993) Diagnosis of prostatic carcinoma: value of random transrectal sonographically guided biopsies. Am J Roentgenol 161:1003–1006
Ellis WJ, Chetner MP, Preston SD, Brawer MK (1994) Diagnosis of prostatic carcinoma: the yield of serum prostate specific antigen, digital rectal examination and transrectal ultrasonography. J Urol 152:1520–1525
Cornud F, Belin X, Piron D et al (1997) Color Doppler-guided prostate biopsies in 591 patients with an elevated serum PSA level: impact on Gleason score for nonpalpable lesions. Urology 49:709–715
Halpern EJ, Rosenberg M, Gomella LG (2001) Prostate cancer: contrast-enhanced US for detection. Radiology 219:219–225
Halpern EJ, Frauscher F, Rosenberg M, Gomella LG (2002) Directed biopsy during contrast-enhanced sonography of the prostate. Am J Roentgenol 178:915–919
Smith RA, Cokkinides V, Eyre HJ (2005) American Cancer Society guidelines for the early detection of cancer. CA Cancer J Clin 55:31–44
Littrup PJ, Bailey SE (2000) Prostate cancer: the role of transrectal ultrasound and its impact on cancer detection and management. Radiol Clin North Am 38:87–113
Halpern EJ, Strup SE (2000) Using gray-scale and color and power Doppler sonography to detect prostatic cancer. Am J Roentgenol 174:623–627
Browne JE, Watson AJ, Hoskins PR, Elliott AT (2004) Validation of a sensitivity performance index test protocol and evaluation of colour Doppler sensitivity for a range of ultrasound scanners. Ultrasound Med Biol 30:1475–1483
Kravchick S, Cytron S, Peled R, Altshuler A, Ben Dor D (2003) Using gray-scale and two different techniques of color Doppler sonography to detect prostate cancer. Urology 61:977–981
Goossen T, Wijkstra H (2003) Transrectal ultrasound imaging and prostate cancer. Arch Ital Urol Androl 75:68–74
Okihara K, Miki T, Joseph BR (2002) Clinical efficacy of prostate cancer detection using power Doppler imaging in American and Japanese men. J Clin Ultrasound 30:213–221
Halpern EJ, Frauscher F, Forsberg F et al (2002) High-frequency Doppler US of the prostate: effect of patient position. Radiology 222:634–639
Aarnink RG, Beerlage HP, de la Rosette JJ, Debruyne FM, Wijkstra H (1998) Transrectal ultrasound of the prostate: innovations and future applications. J Urol 159:1568–1579
Rifkin MD, Sudakoff GS, Alexander AA (1993) Prostate: techniques, results, and potential applications of color Doppler US scanning. Radiology 186:509–513
Lavoipierre AM, Snow RM, Frydenberg M et al (1998) Prostatic cancer: role of color Doppler imaging in transrectal sonography. Am J Roentgenol 171:205–210
Remzi M, Dobrovits M, Reissigl A et al (2004) Can power Doppler enhanced transrectal ultrasound guided biopsy improve prostate cancer detection on first and repeat prostate biopsy? Eur Urol 46:451–456
Bogers HA, Sedelaar JP, Beerlage HP et al (1999) Contrast-enhanced three-dimensional power Doppler angiography of the human prostate: correlation with biopsy outcome. Urology 54:97–104
Frauscher F, Klauser A, Volgger H et al (2002) Comparison of contrast enhanced color Doppler targeted biopsy with conventional systematic biopsy: impact on prostate cancer detection. J Urol 167:1648–1652
Pelzer A, Bektic J, Berger AP et al (2005) Prostate cancer detection in men with prostate specific antigen 4 to 10 ng/ml using a combined approach of contrast enhanced color Doppler targeted and systematic biopsy. J Urol 173:1926–1929
Ragde H, Kenny GM, Murphy GP, Landin K (1997) Transrectal ultrasound microbubble contrast angiography of the prostate. Prostate 32:279–283
Loughlin M, Carlbom I, Busch C et al (1998) Three-dimensional modeling of biopsy protocols for localized prostate cancer. Comput Med Imaging Graph 22:229–238
Egevad L, Frimmel H, Mattson S, Bengtsson E, Busch C (1999) Biopsy protocol stability in a three-dimensional model of prostate cancer: changes in cancer yield after adjustment of biopsy positions. Urology 54:862–868
Egevad L, Frimmel H, Norberg M et al (1999) Three-dimensional computer reconstruction of prostate cancer from radical prostatectomy specimens: evaluation of the model by core biopsy simulation. Urology 53:192–198
Burns PN (1996) Harmonic imaging with ultrasound contrast agents. Clin Radiol 51(Suppl 1):50–55
Burns PN, Hope SD, Averkiou MA (2000) Nonlinear imaging. Ultrasound Med Biol 26(Suppl 1):S19–S22
Halpern EJ, McCue PA, Aksnes AK, Hagen EK, Frauscher F, Gomella LG (2002) Contrast-enhanced US of the prostate with Sonazoid: comparison with whole-mount prostatectomy specimens in 12 patients. Radiology 222:361–366
Zangos S, Eichler K, Engelmann K et al (2005) MR-guided transgluteal biopsies with an open low-field system in patients with clinically suspected prostate cancer: technique and preliminary results. Eur Radiol 15:174–182
Beyersdorff D, Winkel A, Hamm B, Lenk S, Loening SA, Taupitz M (2005) MR imaging-guided prostate biopsy with a closed MR unit at 1.5 T: initial results. Radiology 234:576–581
Salomon L, Colombel M, Patard JJ et al (1999) Value of ultrasound-guided systematic sextant biopsies in prostate tumor mapping. Eur Urol 35:289–293
Wefer J, Hricak H, Vigneron DB et al (2000) Sextant localization of prostate cancer: comparison of sextant biopsy, magnetic resonance imaging and magnetic resonance spectroscopic imaging with step section histology. J Urol 164:400–404
Kelly IM, Lees WR, Richards D (1993) Prostate cancer and the role of color Doppler US. Radiology 189:153–156
Norberg M, Egevad L, Holmberg L, Sparen P, Norlen BJ, Busch C (1997) The sextant protocol for ultrasound-guided core biopsies of the prostate underestimates the presence of cancer. Urology 50:562–566
Patel U, Rickards D (1994) The diagnostic value of colour Doppler flow in the peripheral zone of the prostate, with histological correlation. Br J Urol 74:590–595
Ito H, Kamoi K, Yokoyama K, Yamada K, Nishimura T (2003) Visualization of prostate cancer using dynamic contrast-enhanced MRI: comparison with transrectal power Doppler ultrasound. Br J Radiol 76:617–624
Inahara M, Suzuki H, Nakamachi H et al (2004) Clinical evaluation of transrectal power Doppler imaging in the detection of prostate cancer. Int Urol Nephrol 36:175–180
Acknowledgements
The authors wish to thank Yvonne L. Hoogeveen, PhD, for her assistance in preparing the manuscript.
This review was supported by a grant from the Dutch Cancer Society (grant KUN 2003–2925).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Heijmink, S.W.T.P.J., van Moerkerk, H., Kiemeney, L.A.L.M. et al. A comparison of the diagnostic performance of systematic versus ultrasound-guided biopsies of prostate cancer. Eur Radiol 16, 927–938 (2006). https://doi.org/10.1007/s00330-005-0035-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-005-0035-y