Abstract
The aim of this study was to correlate MR findings of gallbladder wall thickening with pathologic findings on the basis of the layered pattern and to evaluate the diagnostic value of MR imaging in gallbladder disease. We retrospectively evaluated the source images of HASTE sequences for MR cholangiography in 144 patients with gallbladder wall thickening. The layered pattern of thickened wall was classified into four patterns. Type 1 shows two layers with a thin hypointense inner layer and thick hyperintense outer layer. Type 2 has two layers of ill-defined margin. Type 3 shows multiple hyperintense cystic spaces in the wall. Type 4 shows diffuse nodular thickening without layering. MR findings of a layered pattern of thickened gallbladder were well correlated with histopathology. Chronic cholecystitis matched to type 1, acute cholecystitis corresponded to type 2, adenomyomatosis showed type 3, and the gallbladder carcinomas showed type 4. All four layered patterns were associated with PPV of 73% or greater, sensitivity of 92% or greater and specificity of 95% or greater. Our results indicate that MR findings of gallbladder wall thickening are characteristic in each entity and correlate well with pathologic findings. The classification of the layered pattern may be valuable for interpreting thickened gallbladder wall.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Efforts to differentiate diffuse wall thickening, which is a common manifestation of gallbladder diseases, have been vigorously made in research using various imaging modalities. Ultrasonography (US) has been the traditional screening method of choice in the diagnosis of gallbladder disease [1, 2]. Since the findings of thickening of the gallbladder on US are nonspecific, the differential diagnosis of gallbladder disease in patients with thickened gallbladder wall can be difficult [3, 4]. As a means of covering this disadvantage, magnetic resonance (MR) imaging has been used for the evaluation of gallbladder diseases. Recently, with refinements in MR imaging and MR cholangiography technique, MR imaging has become a modality that has potential use to evaluate the gallbladder [5, 6].
MR cholangiography is a noninvasive imaging technique that has proven to be accurate in the diagnosis of bile duct abnormality. Use of MR cholangiography is increasing for the evaluation of choledocholithiasis, ductal anatomy and ductal abnormality in many biliary diseases [7–12]. For this reason, radiologists frequently encounter gallbladder diseases during the evaluation of the MR cholangiography. However, they have no concern for gallbladder on MR cholangiography. Besides, during our practices, we have often found layered patterns of thickened gallbladder wall on the source image of half-Fourier acquisition single-shot turbo spin-echo (HASTE) sequence during MR cholangiography. We hypothesized that if MR imaging can frequently reveal a particular layered pattern of the gallbladder wall in patients with a particular disease entity, these layered patterns would then be valuable for the differential diagnosis of gallbladder diseases and give additional information on gallbladder abnormality during the evaluation of the bile duct on MR cholangiography.
Although MR findings of acute cholecystitis, chronic cholecystitis and gallbladder carcinoma have been reported [5, 6, 13–17], to our knowledge, MR imaging findings in large series of patients with gallbladder disease and the schematic analysis of MR imaging findings for gallbladder wall thickening have not been well documented. Therefore, the purpose of this study was to correlate the MR findings of gallbladder wall thickening with the pathologic findings on the basis of the layered pattern and to evaluate the diagnostic value of HASTE MR imaging in gallbladder disease.
Materials and methods
Subjects
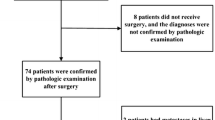
By performing a computerized search of medical records and MR imaging reports, we identified 342 patients who had undergone preoperative MR cholangiography before cholecystectomy between January 2001 and December 2002 at our institution. HASTE MR imaging (the source image for MR cholangiography) of all cases was then reviewed for selection of thickened gallbladders. We measured the gallbladder walls of all 342 patients on HASTE MR imaging. A gallbladder wall more than 3-mm thick was considered thickened [18]. One hundred ninety-eight patients were excluded because the walls of these patients were not thickened (less than 3 mm). A total of 144 patients who had a wall thickened more than 3 mm were selected for this retrospective study. The study population consisted of 94 men and 50 women (age range, 27–79 years; mean age, 55 years). All patients underwent cholecystectomy (open, n=20; laparoscopic, n=124) and had histological confirmation. Preoperative MR cholangiography was performed in all patients for the evaluation of clinically suspected choledocholithiasis. The mean interval from MR cholangiography to surgery was 3.6 days (range, 0–7 days). A pathologist reviewed the pathology reports and slides. The final patient diagnoses were acute cholecystitis (n=64) (acute cholecystitis included acute gangrenous cholecystitis and acute on chronic cholecystitis), chronic cholecystitis (n=57), adenomyomatosis (n=10), xanthogranulomatous cholecystitis (n=1) and gallbladder carcinoma (n=12).
The institutional review boards at our hospitals do not require their approval or informed patient consent for review of medical records, files and images.
MR technique
MR imaging was performed on a 1.5-T superconducting unit (Magnetom Vision Plus; Siemens, Erlangen, Germany) using a body phased-array coil. Patients were asked to fast for a minimum of 6 h. Contrast agents and antispasmodic agents were not used. Prior to MR cholangiography, we performed axial T1-weighted fast low-angle shot (FLASH) sequences or true fast imaging with steady-state procession (FISP) to localize the biliary trees. MR cholangiography was performed using a HASTE sequence with breath holds and a half-Fourier rapid acquisition with relaxation enhancement. We evaluated the HASTE imaging on this study. We did not include axial T1-weighted and true FISP images in this study because not all patients went through the same imaging sequence; some had T1-weighted imaging while others true FISP imaging. We used sequential multisection acquisition (3-mm section thickness; imaging time, 18 s) and obtained an oblique coronal (10°, left anterior oblique) projection for the HASTE sequence. The imaging parameters were as follows: echo train length, 128; effective echo time, 95 ms; one excitation; field of view, 32–35 cm; matrix, 224×256. Because HASTE is a single-shot sequence, there is no repetition time. Fat saturation was routinely used to suppress the signal from peritoneal tissue.
Image analysis
The studies were randomized and retrospectively reviewed individually by three experienced abdominal radiologists (S.E.J, S.E.R and B.G.C) unaware of the pathologic diagnosis. For each patient, the layered pattern of thickened wall was determined by the presence of striation, features of the inner and outer layers and the signal intensity of each layer (compared with that of bile juice and adjacent hepatic parenchyma) and classified into one of four patterns. Type 1 pattern was defined as two layers with a discrete margin. The inner layer showed thin, uniform, and low signal intensity. The outer layer showed thick, high signal intensity (Fig. 1a). Type 2 pattern was defined as two layers with an ill-defined margin. The inner layer was broadened or interrupted. The outer layer showed heterogeneous intermediate signal intensity (Fig. 2a). Type 3 pattern was defined as multiple cystic spaces of high signal intensity in the thickened wall whether or not layering of the thickened wall was present (Fig. 3a). Type 4 pattern was defined as diffuse nodular wall thickening without layering. The wall showed homogeneous low signal intensity (Fig. 4a). Agreement regarding the classification of the thickened gallbladder wall was reached by consensus. Disagreements were resolved by majority opinion. The layered patterns included in the classification scheme were defined a priori and were based on the authors’ previous experience in reviewing MR cholangiography.
Chronic cholecystitis in a 45-year-old man. a Oblique HASTE (TE=95 ms) image for MR cholangiography shows thickened gallbladder wall with two layers. The margin of the thickened wall is discrete. The inner layer with dark signal intensity is uniform and thin. The outer layer is thick with high signal intensity. b Photomicrograph (original magnification, ×40; HE stain) shows intact mucosal and muscular layers and serosal edema with infiltrations of mononuclear inflammatory cells
Acute cholecystitis in a 71-year-old woman. a Oblique HASTE (TE=95 ms) image for MR cholangiography shows thickened gallbladder wall with two layers. The margin of the thickened wall is ill-defined. The inner layer is broadened and focally interrupted. The outer layer is heterogeneous with intermediate signal intensity. b Photomicrograph (original magnification, ×40; HE stain) shows sloughed mucosa (arrows) and a split muscular layer with hemorrhage and extensive acute inflammatory cell infiltrations
Adenomyomatosis in a 43-year-old man. a Oblique HASTE (TE=95 ms) image for MR cholangiography shows thickened gallbladder wall with multiple cystic spaces of high signal intensity. b Photomicrograph (original magnification, ×40; HE stain) shows branching duct or gland-like structures (arrows) in the wall and hyperplasia of the smooth muscle
Additionally, images were evaluated for gallbladder distension, wall thickness and pericholecystic fluid collection. Two observers (S.E.J and S.E.R) measured the wall thickness at the most thickened region and the long-axis and short-axis [magnified images (×2) in an independent console of the MR imaging system. A gallbladder was considered distended when the area of its short and long axes (in centimeters) was greater than 50 cm2 (corresponding to a surface area of 50 cm2 × [π/4]) [19].
Histologic examination
The histopathologic findings in surgical specimens from all of the patients were retrospectively reviewed by a pathologist, with special emphasis on the layered pattern of the thickened wall. One radiologist (S.E.J) and one pathologist (K.L) correlated the MR findings with the histopathologic findings by means of a layer-to-layer comparison and correlated the layered pattern on MR imaging with the final histopathologic diagnosis.
Statistical analysis
To define a correlation between the layered pattern and the final diagnosis, we obtained the positive predictive value (PPV) for each layered pattern and the sensitivity and specificity for each histologic diagnosis. PPV indicates the probability that a specific diagnosis is present in the case of a particular type of the layered pattern. Sensitivity represents the probability that a particular type of the layered pattern will be observed in patients with a specific diagnosis. Specificity indicates the probability that a particular type of the layered pattern will be present only when a specific diagnosis is present.
We used a SPSS 10.0 version (SPSS, Inc., Chicago, IL) for statistical analysis. To determine differences of ancillary findings among histologic diagnoses, we used one-way factorial analysis of variance (ANOVA) with Scheffe’s post-hoc test for the thickness of the gallbladder and the χ2 test for gallbladder distension and pericholecystic fluid. A P value of less than 0.05 was considered to indicate a statistically significant difference.
Results
Layered pattern and pathologic correlation
Type 1 showed two layers with a discrete margin. The inner layer corresponded to intact mucosa and compact muscular layer and the outer layer corresponded pathologically to serosal edema (Fig. 1). Type 2 had two layers with an ill-defined margin. On pathologic correlation, the inner layer corresponded to sloughed mucosa and the outer layer to a split muscular layer with hemorrhage and extensive acute inflammatory cell infiltrations (Fig. 2). Type 3 showed multiple cystic spaces of high signal intensity in the thickened wall, consistent with Rokitansky-Aschoff sinuses (Fig. 3). Type 4 corresponded to diffuse tumor cell infiltrations through the entire wall (Fig. 4).
Layered pattern and corresponding diagnosis
Correlation of the layered patterns and final diagnoses of the 144 thickened walls of gallbladder are summarized in Table 1. Fifty-eight walls demonstrated the type 1 pattern of two discrete layers of thin inner layer with dark signal intensity: 55 (95%) chronic cholecystitis and 3 (5%) acute cholecystitis. Sixty lesions demonstrated the type 2 pattern of two layers with a broadened and interrupted inner layer: 58 (97%) acute cholecystitis and 2(3%) chronic cholecystitis. Eleven walls exhibited the type 3 pattern of multiple intramural cystic lesions: ten (90%) adenomyomatosis and one (10%) gallbladder carcinoma. Fifteen walls exhibited the type 4 pattern of diffuse nodular wall thickening with homogeneous dark signal intensity: 11 (73%) gallbladder carcinoma, 3 (20%) acute cholecystitis and 1 (7%) xanthogranulomatous cholecystitis.
The PPVs of each pattern for the individual final diagnoses are given in Table 2. Three types of the layered pattern were associated with PPVs of 91% or greater: type 1 pattern for chronic cholecystitis, type 2 pattern for acute cholecystitis and type 3 pattern for adenomyomatosis. The remaining type 4 pattern was associated with PPV of 73% for gallbladder carcinoma.
The layered patterns associated with each diagnosis are summarized in Table 2, as are their corresponding sensitivity and specificity values. For chronic cholecystitis, the type 1 pattern of discrete two layers with a thin inner layer was also highly sensitive and specific (sensitivity, 93%; specificity, 97%). Two cases of chronic cholecystitis of decreased signal intensity in the outer layer showed prominent fibrosis in the muscular layer and serosa. For acute cholecystitis, the type 2 pattern of two layers with a broadened and interrupted inner layer is highly sensitive and specific (sensitivity, 90%; specificity, 95%). Three cases of acute cholecystitis showing type 4 pattern are acute gangrenous cholecystitis, which has extensive hemorrhagic necrosis of the entire wall, histopathologically (Fig. 5). All of the adenomyomatosis lesions exhibited the intramural cystic change, making this pattern highly sensitive and specific (sensitivity, 100%; specificity, 99%). For gallbladder carcinoma, the type 4 pattern was also highly sensitive and specific (sensitivity, 92%, specificity, 97%). A case of early gallbladder carcinoma with the type 3 pattern showed involvement of the mucosal layer of tumor cells and extension to the Rokitansky‐Aschoff sinuses.
Acute gangrenous cholecystitis in a 45-year-old man. a Oblique HASTE (TE=95 ms) image for MR cholangiography shows thickened gallbladder wall without layering. The margin of the thickened wall is ill-defined. The wall is homogeneously hypointense. b Photomicrograph (original magnification, ×40; HE stain) shows sloughed mucosa and extensive hemorrhagic necrosis involving the entire wall
Other findings and corresponding diagnoses
Gallbladder distension is significantly (P=0.0001) more common in acute cholecystitis (63 of 64 patients) than in chronic cholecystitis (19 of 57), adenomyomatosis (3 of 10), xanthogranulomatous cholecystitis (1 of 1) and carcinoma (2 of 12). The mean of gallbladder wall thickness is 9.6±2.0 mm in acute cholecystitis, 7.2±2.7 mm in chronic cholecystitis, 10.8±1.9 mm in adenomyomatosis and 11.0±2.4 mm in carcinoma. There are no significant differences among these diagnoses. Pericholecystic fluid collection is significantly (P=0.000) more common in acute cholecystitis (48 of 64 patients) than in chronic cholecystitis (5 of 57), adenomyomatosis (2 of 10) and carcinoma (4 of 12).
Discussion
In this study, we used HASTE source images for MR cholangiography to evaluate the gallbladder wall thickening. This sequence has already been shown to be a technique for evaluating gallbladder pathology. Park et al. [13] issued a report regarding the usefulness of MR cholangiography using HASTE sequence for the depiction of cystic duct and gallbladder neck calculi in the evaluation of cystic duct obstruction. They mentioned that gallbladder wall thickening in acute cholecystitis showed intermediate signal intensity on HASTE image. Regan et al. [15] described that HASTE imaging has a high degree of accuracy in diagnosing acute cholecystitis based on the single finding of pericholecystic high signal intensity. However, to our knowledge, the differentiation of the gallbladder wall thickening focusing on the layered pattern using HASTE images has not yet been established. One study describing the MR imaging features of the wall of the gastrointestinal tract revealed that mucosa showed low signal intensity, the submucosa high signal intensity, the muscular propria low signal intensity and the adventitia high signal intensity on T2-weighted high resolutional MR images [20]. The normal gallbladder wall is composed of four layers: the mucosa, lamina propria, an irregular muscle layer and serosa of loose connective tissue. There is no muscularis mucosa or submucosa [21]. Thus, we consider that the gallbladder wall showed an inner layer of low signal intensity consisting of the mucosal and muscular layers and outer layer of high signal intensity of the serosa on T2-weighted images of high resolutional MR imaging. However, there was no discernible layering in the nonthickened normal gallbladder wall on HASTE images. In the cases with thickened gallbladder wall from this study, HASTE images could distinguish mucosa and muscle from serosa. In our study, correlation of HASTE MR image findings and histologic specimens of thickened gallbladder wall could suggest that the inner layer, which has low signal intensity, represents the mucosal and muscular layers, and the outer layer with high signal intensity represents the subserosal and serosal layers.
Chronic cholecystitis showed mononuclear cell infiltrations in the wall and subserosal fibrosis and edema on histologic examination. The mucosa itself was generally preserved. Intact mucosa and muscular layer corresponded to the thin inner layer of dark signal intensity. Subserosal edema corresponded to the thicker outer layer of high signal intensity in most of the cases. Two cases of chronic cholecystitis showed intermediate signal intensity of the outer layer as in the type 2 pattern. However, intermediate signal intensity corresponded to marked subepithelial and subserosal fibrosis. Fibrosis is a characteristic finding in chronic cholecystitis; however, in the cases from the present study, the degree of inflammatory reaction and fibrosis was variable, and no signal change was seen in most cases except for two.
In acute cholecystitis, the gallbladder wall is thickened due to filling of the spaces by edematous fluid, extravasated blood and inflammatory cells with sloughed mucosa. The signal of an edematous gallbladder wall would not be suppressed completely on MR cholangiography, because it would contain fluid although the amount might be minimal. Sloughed mucosa was consistent with a broadened or interrupted inner layer on HASTE images. Three cases of acute cholecystitis showed a diffusely thickened wall of the type 4 pattern. This lesion showed gangrenous cholecystitis on pathologic examination. Gangrenous cholecystitis shows ischemic necrosis of the gallbladder wall with or without associated cystic artery thrombosis [22]. Accordingly, we suppose that total ischemic hemorrhagic necrosis of the gallbladder wall corresponds to diffuse low signal intensity of the wall without layering on HASTE MR imaging. Differentiation between gangrenous cholecystitis showing a type 4 pattern and gallbladder carcinoma can be difficult, especially in case of gallbladder carcinoma presenting gangrenous cholecystitis. However, in general, ancillary findings, such as pericholecystic fluid collection, may be helpful in the diagnosis of gangrenous cholecystitis.
Clinically, gangrenous cholecystitis portends high conversion rates in patients undergoing laparoscopic cholecystectomy. It is important to identify preoperative factors predictive of gangrenous cholecystitis so that the surgeon may be informed of this potential complication [23, 24].
Adenomyomatosis is a subtype of chronic cholecsytitis that histologically shows branching duct or gland-like structures (Rokitansky-Aschoff sinus) in the wall and hyperplasia of the smooth muscle [21]. Multiple intramural sinuses were clearly defined as discrete, hyperintense intramural cystic structures within the thickened wall on HASTE images in our study. Other investigators [16, 17] reported wall thickening, and intramural sinuses were depicted on T2-weighted images as well as gadolinium-enhanced breath-hold images. Yoshimitsu et al. [17] suggested that the half-Fourier rapid acquisition with relaxation enhancement is more useful for diagnosis than other T2-weighted images or contrast-enhanced dynamic MR sequences. HASTE images were not included in their study. We suggested that HASTE imaging is useful for detection of intramural cystic structures.
In our study, most gallbladder carcinomas show homogeneous low signal intensity without layering; this represents infiltration of the cancer into the wall. A case of gallbladder carcinoma showed thickened wall with intramural cystic structures corresponding to involvement of the mucosa layer of cancer cells and extension to the Rokitansky-Aschoff sinuses. This finding is suggestive of varying imaging findings in gallbladder carcinoma according to its local extension.
Xanthogranulomatous cholecystitis is a pseudotumoral inflammatory condition of the gallbladder that radiologically simulates gallbladder carcinoma [25]. The overlap in the imaging features of xanthogranulomatous cholecystitis and gallbladder carcinoma makes preoperative distinction between these entities virtually impossible [25, 26]. CT may demonstrate low-attenuation foci in the gallbladder wall that correspond to the hypoechoic nodules seen on US, which represent xanthogranuloma or intramural abscess. There are some reports of the MR imaging appearance of xanthogranulomatous cholecystitis [27–29]. On MR imaging, intramural abscess or necrosis shows as the very high signal intensity areas on T2-weighted images without enhancement, and abundant proliferation of foamy cells reveals as the slightly high-intensity areas on T2-weighted images with strong enhancement on delayed phase [28]. However, if intramural abscess or xanthoma is not apparant, the MR findings are nonspecific. We had only one case of xanthogranulomatous cholecystitis that showed a type 4 pattern, and this case could not be differentiated from gallbladder carcinoma on HASTE MR imaging.
Gallbladder distension and pericholecystic fluid collection were significant indicators for differentiating acute cholecystitis from the other diagnoses. However, the maximum wall thickness was not a significant indicator for differentiating disease entities.
The limitations of this study include the small number of gallbladder carcinomas and exclusion of secondary wall thickening. In our study, a mass replacing the gallbladder and the intraluminal polypoid mass of gallbladder carcinoma were not included. We focused on the layered pattern of thickened gallbladder wall rather than on the local staging of tumor invasion. Some investigators [5, 6] reported that dynamic MR imaging can be useful for differentiating between benign and malignant gallbladder lesions and for evaluation of its local extension. We suggested that if thickened gallbladder wall with lobulated margin and homogeneous dark signal intensity are seen on HASTE images during MR cholangiography for the evaluation of choledocholithiasis, gallbladder carcinoma is suspected and avoidance of immediate surgery and further evaluation should be recommended. We did not include secondary gallbladder wall thickening because there cannot be pathologic correlation. These conditions include heart failure, cirrhosis, hepatitis, hypoalbuminemia and renal failure [28]. Secondary wall thickening may show the type 1 pattern, suggesting subserosal edema. In addition, further investigation is needed to determine if the layered pattern that was used in this study is valuable for other sequences or gadolinium-enhanced T1-weighted image.
In conclusion, MR findings of gallbladder wall thickening are characteristic in each entity and correlate well with pathologic findings. Classification of the layered pattern used in this study may be a useful tool for interpreting thickened gallbladder wall and for arriving at a differential diagnosis between acute and chronic cholecystitis and cholecystitis and carcinoma. Careful assessment of the gallbladder wall on HASTE imaging during MR cholangiography may be helpful for surgical planning.
References
Cooperberg PL, Gibney RG (1987) Imaging of the gallbladder. Radiology 163:605–613
McIntosh DM, Penney HF (1980) Gray-scale ultrasonography as a screening procedure in the detection of gallbladder disease. Radiology 136:725–727
Teefey SA, Baron RL, Bigler SA (1991) Sonography of the gallbladder: significance of striated (layered) thickening of the gallbladder wall. Am J Roentgenol 156:945–947
Shlaer WJ, Leopold GR, Scheible FW (1981) Sonography of the thickened gallbladder wall: a nonspecific finding. Am J Roentgenol 136:337–339
Yoshimitsu K, Honda H, Kaneko K et al (1997) Dynamic MRI of the gallbladder lesions: differentiation of benign from malignant. J Magn Reson Imaging 7:696–701
Demachi H, Matsui O, Hoshiba K et al (1997) Dynamic MRI using a surface coil in chronic cholecystitis and gallbladder carcinoma: radiologic and histopathologic correlation. J Comput Assist Tomogr 21:643–651
Irie H, Honda H, Tajima T et al (1998) Optimal MR cholangiopancreatographic sequence and its clinical application. Radiology 206:379–387
Reinhold C, Taourel P, Bret PM et al (1998) Choledocholithiasis: evaluation of MR cholangiography for diagnosis. Radiology 209:435–442
Mendler MH, Philippe B, Sautereau D et al (1998) Value of MR cholangiography in the diagnosis of obstructive diseases of the biliary tree: a study of 58 cases. Am J Gastroenterol 93:2482–2490
Becker CD, Grossholz M, Becker M, Mentha G, de Peyer R, Terrier F (1997) Choledocholithiasis and bile duct stenosis: diagnostic accuracy of MR cholangiopancreatography. Radiology 205:523–530
Lopera JE, Soto JA, Múnera F (2001) Malignant hilar and perihilar biliary obstruction: Use of MR cholangiography to define the extent of biliary ductal involvement and plan percutaneous interventions. Radiology 220:90–96
Fulcher AS, Turner MA, Capps GW, Zfass AM, Baker KM (1998) Half-Fourier RARE MR cholangiopancreatography: experience in 300 subjects. Radiology 207:21–32
Park MS, Yu JS, Kim YH et al (1998) Acute cholecystitis: comparison of MR cholangiography and US. Radiology 209:781–785
Hakansson K, Leander P, Ekberg O, Hakansson HO (2000) MR imaging in clinically suspected acute cholecystitis. A comparison with ultrasonography. Acta Radiol 41:322–328
Regan F, Schaefer DC, Smith DP, Petronis JD, Bohlman ME, Magnuson TH (1998) The diagnostic utility of HASTE MRI in the evaluation of acute cholecystitis. Half-Fourier acquisition single-shot turbo SE. J Comput Assist Tomogr 22:638–642
Kim MJ, Oh YT, Park YN et al (1999) Gallbladder adenomyomatosis: findings on MRI. Abdom Imaging 24:410–413
Yoshimitsu K, Honda H, Jimi M et al (1999) MR diagnosis of adenomyomatosis of the gallbladder and differentiation from gallbladder carcinoma: importance of showing Rokitansky-Aschoff sinuses. Am J Roentgenol 172:1535–1540
Engel JM, Deitch EA, Sikkema W (1979) Gallbladder wall thickness: sonographic accuracy and relation to disease. Am J Roentgenol 134:907–909
Dinkel H, Kraus S, Heimbucher J et al (2000) Sonography for selecting candidates for laparoscopic cholecystectomy: a prospective study. Am J Roentgenol 174:1433–1439
Imai Y, Kressel HY, Saul SH et al (1990) Colorectal tumors: an in vitro study of high-resolution MR imaging. Radiology 177:695–701
Lichtenstein JE (2000) Adenomyomatosis and cholesterolosis: the “hyperplastic cholecystoses”. In: Gore RM, Marc SL (eds) Textbook of gastrointestinal radiology, 2nd edn. Saunders, Philadelphia, pp 1353–1359
Cotran RS, Kumar V, Robbins SL (1989) Pathologic bases of disease, 4th edn. Saunders, Philadelphia, p 971
Ahmad MM, Macon WL (1983) Gangrene of the gallbladder. Am Surg 49:155–158
Singer JA, McKeen RV (1994) Laparoscopic cholecystectomy for acute or gangrenous cholecystitis. Am Surg 60:326–328
Chun KA, Ha HK, Yu ES et al (1997) Xanthogranulomatous cholecystitis: CT features with emphasis on differentiation from gallbladder carcinoma. Radiology 203:93–97
Parra JA, Acinas O, Bueno J, Guezmes A, Fernandez MA, Farinas MC (2000) Xanthogranulomatous cholecystitis: clinical, sonographic, and CT findings in 26 patients. Am J Roentgenol 174:979–983
Furuta A, Ishibashi T, Takahashi S, Sakamoto K (1996) MR imaging of xanthogranulomatous cholecystitis. Radiat Med 14:315–319
Shuto R, Kiyosue H, Komatsu E et al (2004) CT and MR imaging findings of xanthogranulomatous cholecystitis: correlation with pathologic findings. Eur Radiol 14:440–446
Hatakenaka M, Adachi T, Matsuyama A, Mori M, Yoshikawa Y (2003) Xanthogranulomatous cholecystitis:importance of chemical-shift gradient-echo MR imaging. Eur Radiol 315–319:2233–2235
Levy AD, Murakata LA, Rohrmann CA Jr (2001) Gallbladder carcinoma: radiologic–pathologic correlation. RadioGraphics 21:295–314
Acknowledgements
We thank Bonnie Hami, M.A. (Department of Radiology, University Hospitals of Cleveland, Cleveland, OH), for her editorial assistance in the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jung, S.E., Lee, J.M., Lee, K. et al. Gallbladder wall thickening: MR imaging and pathologic correlation with emphasis on layered pattern. Eur Radiol 15, 694–701 (2005). https://doi.org/10.1007/s00330-004-2539-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-004-2539-2