Abstract
The study was performed to compare whole-body short time inversion recovery (STIR) MR imaging and 99mTc-methylene diphosphonate planar scintigraphy in the examination of children with suspected multifocal skeletal malignant lesions. Sixteen patients with known or suspected malignant skeletal disease underwent both whole-body STIR MR imaging and bone scintigraphy. The lesions were described and numbered according to scintigraphic evaluation criteria. Thus, 16 regions were analyzed in each patient for the comparison between the two modalities. Histology was proven in the primary malignant regions. Follow-up MRIs were registered. Scintigraphy and MRI follow-up were evaluated as gold standard. A total of 139 different lesions was observed by both modalities. Baseline whole-body MRI revealed 119 bone lesions in 256 possible sites (46.5%); scintigraphy revealed only 58 lesions (22.6%). Congruence was observed in only four patients (25%). According to the location of the lesion, correlation was observed in 39/139 lesions (28%). In all, 57.5% of the lesions were detected only by MRI and 14.5% of the lesions were detected only by scintigraphy. Whole-body MRI was more sensitive (P<0.001). Of all lesions numbered which could be separated in the initial MRI, whole-body MRI detected 178 lesions in the patients. The results suggest that whole-body MRI using a STIR sequence is an effective radiation free method for examination of children with suspected multifocal bone lesions. MRI showed more lesions than conventional 99mTc-methylene diphosphonate scintigraphy. Therefore, whole-body MRI may be feasible as a screening modality for metastatic and skip lesions in osteosarcoma, PNET, Ewing sarcoma and Langerhans cell histiocytosis in children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In patients with primary malignant bone tumors or neoplasia potentially metastasizing to the bones, the diagnosis of bone metastasis is crucial to determine the prognosis and to optimize therapy. On radiographs, metastases to the bone only become apparent after the loss of more than 50% of bone mineral content at the location of the disease. So far, the standard method for initial staging is 99mTc-phosphonate-based skeletal scintigraphy. However, this method detects bone metastases only in a relatively advanced stage of tumor infiltration when osteoblastic host reaction to tumor deposits has already occurred [1]. Imaging techniques such as magnetic resonance imaging (MRI) and positron emission tomography (PET) can identify bone metastases or primary tumors at an earlier stage [2, 3]. Recent developments in MRI sequence development with implementation of fast turbo sequences into the clinical routine and a general decrease in imaging costs have led to an increased interest in MRI as a potential tool for whole-body screening. In adults, MRI using short time inversion recovery (STIR) sequences has been found to be more sensitive for the detection of bone metastases than scintigraphy [4]. The aim of our study was to compare whole-body STIR MRI and 99mTc-methylene diphosphonate planar scintigraphy in children and adolescents with malignant bone lesions.
Materials and methods
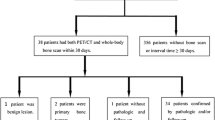
Out of a series of 44 children and adolescents referred for whole-body MR imaging only in 16 patients with histologically proven malignant lesions (nine boys and seven girls; age 4 months to 24 years; median 9 years 7 months), a whole-body MRI using a STIR sequence and a 99mTc-methylene diphosphonate planar scintigraphy were performed with a time interval of 5 weeks maximum between scintigraphy and MRI. In the remaining 28 patients, the time interval between the both modalities was over 5 weeks or only one of the two methods was performed. Informed written consent was obtained from all patients or their carers. In five patients, MRI was the first investigation (27.1%). In six patients, MRI and scintigraphy follow-up investigations were also available for analysis. Each of the 16 patients had known or suspected malignant bone lesions: five patients with Ewing sarcoma, two patients with osteosarcoma, two patients with PNET, one patient with rhabdomyosarcoma, one patient with synovial carcinoma, two patients with Langerhans cell histiocytosis, one patient with renal clear cell carcinoma, one patient with acute leukemia, and one patient with non-Hodgkin lymphoma.
MR imaging technique
MR imaging was performed on a 1.5 T Gyroscan ACS II system (Philips Medical System, Eindhoven, The Netherlands) using two different coil systems (head–neck coil, body coil). Patients were examined in the supine position. Patients under 6 years of age (n=5) were sedated using chloral hydrate or balanced anaesthesia. After administration of the sedative, continuous quantitative monitoring of oxygen saturation, heart rate, respiratory rate, and blood pressure were recorded during the MR examination. The examination was divided into five steps from the head to the feet (head–neck; chest and upper arms; abdomen, pelvis and forearms; tighs and knees; and lower leg and feet). Coronal images were acquired using a turbo STIR sequence (TR/TE 2700 ms/17 ms, TI 160 ms, 10–22 slices) during quiet respiration. The slice thickness was adapted to the anatomical region between 5 mm and 10 mm depending on the anatomical area of interest. The interslice gap was 10% of the slice thickness.
Scintigraphy
Conventional whole-body scintigraphy was performed on a multispec-2-camera (Siemens, Erlangen, Germany). After injection of 99mTc-methylene diphosphonate according to body weight (176–740 MBq; median 468.4 MBq), a large field-of-view (FOV) camera with parallel hole high-resolution collimators was used. Perfusion phase was acquired immediately after tracer application; blood pool phase 5 min and accumulation phase up to 3 h later. Data were analyzed using an ICON Comp. system manufactured by Siemens.
Analysis
Examination times for whole-body MRI were assessed from image data. Consensus analysis of the MRI was performed retrospectively by two experienced pediatric radiologists without knowledge of the results from the scintigraphic investigation (H.J.M., S.V.). The examinations were rated for contrast and image quality. In MRI, a lesion was classified as positive in the case of focal or circumscribed intermediate to higher signal intensity on the STIR images in comparison to skeletal muscle. Diffuse hyperintensities, especially in the lower legs, feet and spine, were proved critically and excluded in order to avoid false positive findings. Bone scintigrams were evaluated by an experienced specialist in nuclear medicine (D.G.) who was blinded for the MR findings. Criterion for stating a lesion was tracer accumulation. The lesions were described in their localization and size and numbered according to the scintigraphic evaluation or the whole-body MR imaging. For comparison of both modalities 16 regions were analyzed in each patient: skull and head–neck region, cervical spine, thoracic spine, lumbar spine, pelvis including sacrum, rib cage including sternum and shoulder girdle, upper arms (2), forearms (2), thighs (2), lower leg (2), feet (2). Therefore, in total 256 regions could be evaluated for the 16 patients at the date of the initial examination.
The histology was proven only for the primary lesions. In patients without synchrone follow-up with MRI and scintigraphy examinations, the follow-up MRI was registered and re-evaluated as the gold standard. Lesions which were detected once more were than scored as true lesions.
Results
All examinations were considered diagnostic. The image quality of both modalities was sufficient in all patients, and examinations were tolerated well by all patients. The duration of the MR examination was between 15 min and 45 min (median 29.45 min), including patient positioning. Short examination times were only reached in babies with two or three different regions covering the whole-body. Radionuclide scintigraphy required latency of 3 h following the tracer injection.
A total of 139 lesions was observed in total of both modalities. In two of the 16 patients (12.5%) neither MRI nor scintigraphy could detect any bone lesion (one patient with renal clear cell carcinoma and one patient with synovial carcinoma who was scanned after tumor extraction). Exact congruence of both modalities was observed only in 4/16 patients (25%). Discrepancies were found in 12 patients (75%). Baseline MR imaging revealed 119 bone lesions in the 256 sites that were analyzed in the 16 patients, while scintigraphy revealed only 58 lesions. Congruence of both methods according to the localization of positive lesions was observed in 28% of all lesions (39/139 lesions). A total of 57.5% of the lesions were detected only by MR imaging (80/139 lesions); 14.5% of the lesions were detected only by scintigraphy (20/139 lesions). Statistical analysis using the McNemar test revealed significant differences in the detection rate of both modalities (P<0.001). Whole-body MRI was more sensitive and showed more lesions, especially in the region of the pelvis (32 lesions versus 16 lesions) and the lower legs (34 lesions versus nine lesions). Similar results between both modalities were observed in the regions of the skull (10 lesions versus 11 lesions) and the spine (14 lesions versus 10 lesions; for examples, see Figs 1, 2, 3). Scintigraphy showed in one patient a lesion in the forearm, whereas MRI was negative. Because of its peripheral location in the FOV, this region was not imaged completely. In the ribcage and in the upper arms, MRI was superior to scintigraphy (18 versus eight lesions; ten versus five lesions). In one patient with only six scintigraphic detectable lesions, 14 lesions were accessed as positive by the initial MR investigation. In the follow-up study 9 months later, all these lesions were positive in the scintigram. Additional findings in the whole-body MRI were pleural effusions and affections of the paranasal sinuses. Pulmonary metastases could be detected in one patient by whole-body MR imaging which were confirmed with the findings in CT. Hepatic metastases could not be detected in our patients by whole-body MR imaging, but in none of our patients did CT or MRI reveal metastases of the abdomen.
A 7-month-old boy with Langerhans cell histiocytosis and extensive bone lesion in the pelvis. a Findings of whole-body MRI could be confirmed as a lesion in the left os ilium with high signal intensity on short time inversion recovery sequence (arrows). A further circumscribed lesion with intermediate signal intensity was observed in the left femur. Additional findings were pleural effusion and the large soft tissue mass in the pelvis. b Bone scintigraphy shows only the lesion in the left pelvis
A 12-year-old girl with multifocal Ewing sarcoma of the left os pubis. Initial coronal Turbo STIR whole-body MR images showed lesions in the os ilium at both sides, lesions of the proximal femur, and the proximal tibia (arrows), whereas bone scintigraphy showed only the primary lesion. Further lesions in the initial MRI involved the scapula, the skull (temporomandibular joint), the humerus, and the spine
Discussion
In our study, whole-body MR imaging showed a higher number of bone lesions than standard skeletal scintigraphy in children and young adults with malignancies; a finding which is in accordance with the results of Daldrup-Link et al. [1]. They suggested as the pathological basis for the discrepancy in detection rates an initial accumulation of hematogenously seeded tumor cells in the intramedullary compartment only visible in MRI, with subsequently reactive osteoblastic responses then detectable by standard skeletal scintigraphy as well. Additionally, the tumor infiltration of the bone marrow space can be detected by MRI at a very early stage before metabolic or structural changes of trabecular or cortical bone are depicted on bone scans or radiographs or CT scans [5]. Radionuclide scintigraphy is very sensitive and provides a rapid overview of the entire skeletal system. Despite the widely accepted sensitivity of scintigraphy, it lacks diagnostic specificity, and in many cases additional imaging is necessary for further characterization of suspicious regions [4]. Based on tracer uptake in areas of osteoblastic and/or osteoclastic activity, skeletal Tc-scintigraphy is considered as the clinical reference standard for detection of bone lesions. Scintigraphic activity at the growth plates in children can be seen and has to be classified as normal. Sometimes the differentiation between growth plate and marrow lesions is difficult. Bone marrow scintigraphy with gallium (67Ga) has been used, especially for the evaluation of bone marrow infiltration in patients with lymphoma. It is well known that 67Ga-scintigraphy shows a higher sensitivity for the detection of bone marrow lesions than skeletal scintigraphy [6], but the radiation exposure on bone marrow scintigraphy is considered as to be too high for routine staging in children. In addition, the sensitivity of 67Ga-scintigraphy to lymphoma depends on the type of lymphoma [7]. 18F-Fluorodeoxyglucose (FDG) PET has a higher sensitivity than standard skeletal scintigraphy for the detection of bone malignancies in children, but PET also has a limited spatial resolution, requiring complementary CT or MR imaging to localize an area of increased glucose metabolism [1]. Furthermore, PET shows a high number of false positive lesions, which have to be monitored by other imaging modalities [3, 8]. The combination of PET and CT will be an alternative in the future to increase the accuracy. Considering costs and availability, whole-body MR imaging may be an alternative method for the evaluation of suspected multifocal bone lesions. In former times, for MRI long acquisition times have been the main limitation for metastases screening of the entire skeleton. New developments in sequence design and auxiliary equipment (e.g. rolling table platform) have led to a major reduction of acquisition times [9]. For imaging of bone marrow lesions with MRI, a combination of T1-weighted and STIR sequences provides all necessary information [1, 5, 9]. For reduction of acquisition times, we used only a turbo STIR sequence in our study according to Eustace et al. [4] and Kavanagh et al. [10]. STIR sequences are characterized by high lesion signal-to-noise ratio (SNR) and proved to be very useful for detecting inflammatory and malignant lesions [11]. However, some authors suggest that especially in children, fewer false positive lesions can be observed in conventional spin-echo images than in STIR sequences [1, 12, 13]. The specificity of the STIR images may be reduced in patients with high cellularity in the bone marrow typically found in children. Sometimes, STIR sequences show high signal intensity adjacent to the growth plate which has to be critical proven. These signal changes are caused by normal proliferative processes near the growth plate and have to be differentiated from lesions according to malignancies or inflammatory processes. Thus, symmetric and diffuse findings of increased signal intensity may be evaluated as false positive lesions. A further cause for false positive findings especially in the region of the lower legs may be subclinical minor bone bruises which often can be observed in small children and which can generate high signals in the STIR sequence. Knowledge about these variants and about the distribution of normal hematopoietic marrow in children is crucial for correct evaluation of image findings [14]. On STIR images, hematopoietic marrow shows a minimal brighter signal intensity than skeletal muscle. Tumor infiltrations, on the other hand, are always hyperintense against the dark background [15]. Further possibilities to reduce the specificity of STIR sequences are fluid-containing lesions, such as simple cysts and hemangiomas. Thus, interpretation of hyperintensity has to be done with caution.
In some studies, bone scintigraphy seemed to be more sensitive than whole-body MRI in the assessment of the ribs, scapulae, and skull [5, 6] caused by possible partial-volume effects in MRI. Our data do not confirm these findings. Whole-body MRI showed a similar number of lesions in the head–neck region as in scintigraphy and depicted more lesions in the chest wall including the ribs and shoulder girdle. Smaller bones (e.g. hand and feet) are described as a further problematic region but in our study group, MRI detected several lesions in the feet which were negative in the scintigram. According to data of the literature [5, 15–17] MRI was clearly superior to bone scanning and provided important information about tumor morphology, tumor extension, and possible complications for the extremities and pelvis.
Limitations of the technique used in our study are the inability to detect submillimeter lesions and to image the entire body in large patients. Using slices between 5 mm and 10 mm thick and an interslice gap of 10% like in our study some smaller lesions can be overlooked. Additional limitations are the duration and costs of the investigation. The need for repositioning the patient during the change of the coil system (head–neck to body coil) and the reposition from head-first to feet-first position do contribute significantly to the total scan time. Using the moving tabletop time can be saved. Further developments like rolling table platforms open possibilities for whole-body MRI [9, 16]. Meanwhile, a total body scan is possible in less than 15 min. Hargaden et al. [17] described many applications for whole-body MRI (skeletal metastatic disease, detection of occult primary malignancies, detection of multiple myeloma, staging of malignancies, diagnosis of polymyositis) and discuss the method as an alternative to autopsy. Engelhard et al. [18] showed that whole-body MRI with automatic table movement can be used as a screening tool for patients with breast cancer for recording bony metastases quickly, non-invasively and with a high degree of reliability. The disadvantage of whole-body MRI is the higher cost, but comparing the costs of whole-body MRI and bone scintigraphy, one has to consider that findings in nuclear medicine studies often require additional examinations for clarification [1, 5]. A disadvantage of our study was the heterogeneity of the study population with a wide spectrum of rare primary malignancies. Further studies are necessary in children and adolescents with more homogenous tumor groups. Such studies may require a multicenter approach.
Conclusion
The concept of whole-body MR imaging is not new, but long acquisition times and poor image quality characterized by extensive artifacts have limited its clinical impact. Although only from a small group of children and adolescents suffering malignancies, our results suggest that whole-body MRI using a STIR-sequence can be applied as a screening modality for the detection of skip lesions and metastases in children with malignancies. If identified lesions cannot be reliably characterized in a whole-body examination, further dedicated examinations are necessary. Additionally, MRI has the potential to detect several non-tumor related pathologies, thus offering an alternative method to planar scintigraphy.
References
Daldrup-Link HE, Franzius C, Link TM, Laukamp D, Sciuk J, Jürgens H, Schober O, Rummeny EJ (2001) Whole-body MR imaging for detection of bone metastases in children and young adults. Am J Roentgenol 177:229–236
Brenner W, Bohuslavizki KH, Eary JF (2003) PET imaging of osteosarcoma. J Nucl Med 44:930–942
Martin W, Delbeke W, Patton J, Sandler M (1996) Detection of malignancies with SPECT versus PET, with 2-[fluorine-18] fluoro-2-dexoy-d-glucose. Radiology 198:225–231
Eustace S, Tello R, De Carvalho V, Carey J, Wroblicka JT, Melhem ER, Yucel EK (1997) A comparison of whole-body turbo STIR MR imaging and planar 99mTc-methylene diphosphonate scintigraphy in the examination of patients with suspected skeletal metastases. Am J Roentgenol 169:1655–1661
Steinborn MM, Heuck AF, Tiling R, Bruegel M, Gauber L, Reiser MF (1999) Whole-body bone marrow MRI in patients with metastatic disease to the skeletal system. J Comput Assist Tomogr 23:123–129
Haubold-Reuter BG, Duewell S, Schilcher BR, Marincek B, v. Schulthess GK (1993) The value of bone scintigraphy, bone marrow scintigraphy and fast spin-echo magnetic resonance imaging in staging of patients with malignant solid tumours: a prospective study. Eur J Nucl Med 20:1063–1069
Iizuka-Mikami M, Nagai K, Yoshida K, Sugihara T, Suetsugu Y, Mikami M, Tamada T, Imai S, Kajihara Y, Fukunaga M (2004) Detection of bone marrow and extramedullary involvement in patients with non-Hodgkin’s lymphoma by whole-body MRI: comparison with bone and 67Ga scintigraphy. Eur Radiol 14: Feb 18 DOI 10.1007/s0030-003-2209-9
Bender H, Kirst J, Palmedo H (1997) Value of 18-fluoro-deoxyglucose positron emission tomography in the staging of recurrent breast cancer. Anticancer Res 17:1687–1692
Lauenstein TC, Freudenberg LS, Goehde SC, Ruehm SG, Goyen M, Bosk S, Debatin JF, Barkhausen J (2002) Whole-body MRI using a rolling table platform for the detection of bone metastases. Eur Radiol 12:2091–2099
Kavanagh E, Smith C, Eustace S (2003) Whole-body turbo STIR MR imaging: controversies and avenues for development. Eur Radiol 2196–2205
Algra P, Bloem J, Tissing H, Falke T, Arndt J, Verboom L (1991) Detection of vertebral metastases: comparison between MR imaging and bone scintigraphy. Radiographics 11:219–232
Fletcher B (1997) Imaging pediatric bone sarcomas. Radiol Clin N Am 35:1477–1494
Onikul E, Fletcher BD, Parham DM, Chen G (1996). Accuracy of MR imaging for estimating intraosseous extent of osteosarcoma. Am J Roentgenol 167:1211–1215
Moore S, Dawson K (1990) Red and yellow marow in the femor: age related changes in appearance at MRI. Radiology 175:219–223
Mazumdar A, Siegel MJ, Narra V, Luchtman-Jones L (2002) Whole-body fast inversion recovery MR imaging of small cell neoplasms in pediatric patients: a pilot study. Am J Roentgenol 179:1261–1266
O’Connell MJ, Hargaden, Powell T, Eustace SJ (2002) Whole-body turbo short tau inversion recovery imaging using a moving tabletop. Am J Roentgenol 179:866–868
Hargaden G, O’Connell MJ, Kavanagh E, Powell T, Ward R, Eustace S (2003) Current concepts in whole-body imaging using turbo short tau inversion recovery MR imaging. Am J Roentgenol 180:247–252
Engelhard K, Hollenbach HP, Wohlfart K, von Imhoff E, Fellner FA (2004) Comparison of whole-body MRI with automatic moving table technique and bone scintigraphy for screening bone metastases in patients with breast cancer. Eur Radiol 14:99–105
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mentzel, HJ., Kentouche, K., Sauner, D. et al. Comparison of whole-body STIR-MRI and 99mTc-methylene-diphosphonate scintigraphy in children with suspected multifocal bone lesions. Eur Radiol 14, 2297–2302 (2004). https://doi.org/10.1007/s00330-004-2390-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-004-2390-5