Abstract
The enhancing area surrounding breast carcinoma on MR mammography is correlated with findings from pathological examination. We studied 194 patients with breast cancer who underwent preoperative MR mammography. Of all malignant lesions presenting with an enhancing surrounding area on MR mammography, morphologic features including long spicules, a ductal pattern, diffuse enhancement or nodules were evaluated and compared with histopathological examination. A double breast coil was used; we performed a 3D FLASH sequence with contiguous coronal slices of 2 mm, before and after injection of 0.2 mmol/kg GD-DTPA, and subtraction images were obtained. In total, 297 malignant lesions were detected at MR mammography and 101 of them had one or more types of enhancing surrounding area. In 49 of the 53 cancers with long spicules and in 49 of the 55 cancers with surrounding ductal pattern of enhancement, pathological examination showed in situ and/or invasive carcinoma. Multiple nodules adjacent to the carcinoma were seen in 20 patients and corresponded with six cases of invasive and ten cases of ductal in situ carcinoma. A diffuse enhancing area next to a mass was seen in ten patients and consisted of carcinoma in all cases: seven in situ and three invasive carcinomas. Enhancing areas including long spicules, a ductal pattern, noduli, or diffuse enhancement surrounding a carcinoma corresponded with in situ or invasive extension of the carcinoma in 92.5, 89, 80 and 100% of cases, respectively.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Accurate assessment of tumor size and detection of intraductal spread are necessary when selecting patients for breast-conserving surgery [1]. Moreover, tumor size is critical for decisions regarding prognosis and the use of adjuvant systemic therapy. Ductal carcinoma in situ (DCIS) around an invasive cancer represents a high risk of local recurrence [2]. Mammography often underestimates tumor size and DCIS around the invasive mass [3]. On ultrasound, intraductal carcinoma is often underestimated [4]. MR mammography has the highest accuracy in assessment of tumor extent [5–7]. A drawback of this technique is the low specificity; benign lesions and normal glandular tissue around a cancer may also enhance and can lead to overestimation of tumor size. Therefore, study of the histopathology of this enhancing surrounding region is important in deciding whether this region should be included in the measurement of the pathological area on MR mammography.
The purpose of our study was to compare the enhancing area surrounding breast carcinoma on MR mammography with findings on pathological examination and to study the assessment of tumor size and extent.
Materials and methods
Patients
In total, 194 consecutive patients with breast cancer diagnosed on clinical examination, mammography, and/or ultrasound who underwent preoperative MR mammography were included in this study. Exclusion criteria were pregnancy, prior breast surgery for malignancy in the same breast, neoadjuvant chemotherapy, and patient age older than 80 years. The study was performed in two hospitals. All patients signed an informed consent form.
Imaging protocol
In both hospitals, patients were imaged with a dedicated breast coil and a three-dimensional fast low-angle shot (3D FLASH) sequence. Sixty-four coronal images were obtained before and after 0.2 mmol/kg GD-DTPA administration and subtraction images were acquired. In center A, we performed one measurement before contrast injection, followed by six measurements after contrast injection. In center B, two measurements were performed after contrast injection. The percentage of maximal enhancement and type of curve were obtained in both centers, moment of maximal enhancement could only be achieved in center A. To evaluate the curve in the enhancing surrounding structures we chose a region of interest (ROI) in a nodule or in the thickest part of a spicule, with ductal or focal enhancement, and we used a ROI that was small enough to avoid underestimation caused by inclusion of nonenhancing environment.
Imaging in center A was performed on a 1.5-T Magnetom 63 SP system and a 1.5-T Symphony Quantum system (Siemens, Erlangen, Germany). Parameters were, respectively, repetition time (TR) of 12.0 and 13.0 ms, echo time (TE) of 5.0 and 6.3 ms, time to acquisition (TA) of 1.27 and 1.15 min, field of view (FOV) of 320 mm, rec FOV 4/8 with an 87% phase resolution (matrix of 112×256) and FOV 320 mm, 50% FOV, and 80% phase resolution (matrix 102×256). On both systems a flip angle of 25° was used and 64 coronal sections of 2.0 mm slice thickness (SL) were acquired. On the Symphony Quantum system an additional sequence with fat saturation with TR 32.0 ms, TE 6.3 ms, TA 6.07 min, SL 3.0 mm, FOV 160–320, and matrix 205×512 was performed.
In center B examinations were performed on a 1-T Magnetom Impact Expert MRI machine (Siemens) and a 3D FLASH sequence with selective water excitation was used with TR 24.0 ms, TE 7.0 ms, TA 3.34 min, flip angle 30°, FOV 160–320 mm, rec FOV 4/8, 70% phase resolution (177×512 matrix), and SL of 3.2 mm.
All MR mammograms were interpreted by an experienced radiologist with knowledge of the patient’s history, clinical examination results, and mammography and ultrasound examination findings.
MR mammography: image interpretation
“Enhancing area surrounding breast carcinoma” contains: enhancing long spicules, a ductal pattern, noduli, or diffuse enhancement surrounding a carcinoma. The first carcinoma detected was called the primary lesion, lesions subsequently identified were called second or subsequent foci, and lesions only seen on MR were called additional foci.
MR mammography–pathology comparison
The radiologist and the gynecologist who performed the operation later, discussed MR mammography examinations preoperatively and therapy was planned taking into account the diameter of the mass and of the surrounding enhancing area. The largest diameter was looked for and measured. Tumorectomy and lumpectomy specimens were anatomically oriented and a drawing was made by the surgeon to show the origin of the specimen; they were then serially sectioned and slices were radiographed. Mastectomy specimens were sectioned at a 5-mm interval. The radiologist and pathologist jointly evaluated tissue slices and MR images. The morphology of the enhancing area surrounding the carcinoma, as seen on MR images, was correlated with the area around the tumor on pathological examination. The extent of lesions on MR mammography was compared with the diameter of the total lesion on pathological examination. In tumorectomy specimens, the in situ component was considered extensive (extensive intraductal component, EIC+) if in the histological cross-section more than 25% of the tumor area consisted of DCIS and if DCIS was present in the surrounding breast tissue outside the margins of the invasive tumor. In lumpectomy specimens, the in situ component was considered extensive if at least 15 ductulobular units around the invasive tumor were involved [8].
The carcinoma was considered multifocal if two or more separate lesions were at a distance of less than 4 cm from each other and multicentric if two or more separate lesions were at a distance of more than 4 cm from each other or in two different quadrants.
Of all malignant lesions presenting with an enhancing surrounding area on MR mammography, morphologic features such as long spicules (>1 cm), a ductal pattern, diffuse enhancement, or nodules were sought, described, and compared with findings on pathological examination by calculating the positive predictive value (PPV).
Diameters of lesions with and without the enhancing surrounding area were measured on MR mammography and compared with the greatest diameter of the lesion on pathological examination. A Spearman Rank correlation coefficient was used. Measurement of the enhancing lesion was considered “exact” if overestimation or underestimation was less than 2 mm.
Results
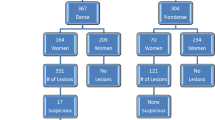
In 194 patients with breast cancer, 297 malignant lesions were detected on MR mammography. In 101 of these 297 (34%) carcinomas, one or more types of enhancing surrounding area were seen. Table 1 shows histopathological diagnosis of the 101 masses with surrounding enhancement. Of these 101 lesions, 81 were primary tumors, 10 were second or subsequent foci, and 10 were additional lesions. Of 81 patients with a primary carcinoma with enhancing surrounding area, 16 had multifocal, 7 had multicentric, and 4 had bilateral carcinomas. In 92 enhancing areas, comparative studies between histopathology and MR mammography were achieved by the radiologist and pathologist. In 81 of these 92 cases (88%) histopathological examination of the surrounding area revealed carcinoma around the cancer, in 2 cases the surrounding enhancement corresponded with lobular in situ carcinoma, in 1 case lymphovascular invasion was present, and in 8 only benign pathology or normal glandular tissue was seen. In 9 of the 101 carcinomas, the surrounding area seen on MR as spiculae, ductal pattern, or small nodules could not be exactly correlated with a histopathological finding, but the maximal diameter on MR (=diameter of the lesion+enhancing surrounding area) was equal to the maximum diameter of the tumor on histopathology. In three of these nine cases, the tumor was a pure DCIS, six other cases were invasive cancers. Taking these 9 cases into account, in 90 (81+9) of the 101 (89.1%) masses with enhancing surroundings, the surroundings correlated with malignant extension. Table 2 shows the pathological findings in different types of areas surrounding these masses.
In 49 of 53 cancers with long spiculae (92.5%) (Fig. 1), pathological examination revealed in situ and/or invasive carcinoma in these spiculae, 14 were EIC+ tumors. In four cases the spicules contained only benign lesions.
A 46--year-old woman. MR: large mass of 38 mm surrounded by spicules and ductal enhancement reaching from the posterior part of the breast up to the nipple (a coronal subtraction image; b,c sagittal reconstruction image). Histopathology (HP) findings: invasive ductal carcinoma of 45 mm, surrounded by low-grade DCIS reaching from the posterior up to the nipple, with multiple small foci of infiltrative carcinoma and lymphovascular invasion. d A ductus lactiferous near the nipple, surrounded by a focus of invasive carcinoma and lymphovascular invasion
Pathological examination of the lesions presenting as a surrounding ductal pattern (Fig. 2) of enhancement on MR mammography revealed the presence of DCIS (n=31), invasive cancer (n=6), or both (n=12) in 49 of 55 cases (89%); 23 of them were EIC+ tumors. Lymphovascular invasion around a carcinoma was detected in one patient. Benign lesions surrounding the carcinoma were seen in five cases.
A 32-year-old woman. MR: mass of 32 mm, with area of ductal enhancement of 30 mm adjacent to it (arrow). HP: invasive ductal carcinoma, EIC+. DCIS did not extent far beyond the mass of the invasive cancer, total diameter of the carcinoma was 27 mm. Area of ductal enhancement corresponded to area of adenosis
Multiple nodules (Fig. 3) adjacent to the lesion were seen in 20 cases, in 16 of them the nodules proved to be malignant (80%). Pathological examination revealed six cases of invasive carcinoma within these nodules and ten cases with DCIS, seven of them with an EIC+ tumor. In two cancers with enhancing nodules around them, lobular carcinoma in situ was found around the tumor.
A 66-year-old woman. MR: mass of 28 mm, surrounded by ductal enhancement (arrow) and nodules (arrowhead), total diameter 65 mm. HP: invasive ductal carcinoma of 30 mm, surrounded by low-grade DCIS, total diameter 60 mm. Shows micropapillary, low-grade DCIS, extending far beyond the margin of the invasive carcinoma
A diffuse enhancing area (Fig. 4) adjacent to a mass was seen in ten cases and consisted of carcinoma in all cases (100%), seven were pure DCIS, three showed also invasive carcinoma, and in five cases it was an EIC+ tumor.
A 25--year-old woman. MR: mass of 32 mm, adjacent to it a diffuse enhancing area (arrowhead), total diameter is 55 mm. HP: invasive ductal carcinoma of 50 mm, infiltrative growth pattern on one side and expansive growth pattern on other side, surrounded by high-grade DCIS and lymphovascular invasion
Of all types of enhancing surrounding areas, 23.9% (n=33) corresponded with strands or small foci of invasive carcinoma surrounding the tumor and 16.7% (n=23) with invasive carcinoma and DCIS. Only six of the small foci of invasive carcinoma surrounding the main carcinoma presented as nodules, while most of them presented as ductal enhancement, as a diffuse enhancing area, or as spicules. The surrounding area contained only DCIS in 49.3% (n=68). In 35.5% the enhancing surrounding area corresponded with DCIS in EIC+ tumors.
The diameter of the total pathological area ranged from 6 to 180 mm (mean size 39.4 mm) on pathological examination. Figure 5 shows the diameters of the total lesions measured on MR mammography compared with the total diameters on histological examination. The Spearman Rank correlation coefficient r was 0.789 (p<0.0001). On MR mammography, if only the part of the lesion without the enhancing surroundings were taken into account, the Spearman Rank correlation coefficient was only 0.485 (Fig. 6). MR mammography overestimated the size of the total lesion in 29 cancers (Fig. 7), was correct in 48 cancers, and underestimated it in 22 cases. In two other patients exact measurement on MR was not possible due to diffuse enhancement of normal breast tissue. The mean overestimation was 19.8 mm, ranging from 3 to 75 mm. The mean underestimation was 19.2 mm, ranging from 3 to 114 mm. Seventeen lesions showed an overestimation of more than 1 cm, 11 of them of more than 2 cm. Overestimation of more than 1 cm was caused by enhancement of normal glandular tissue in five cases and fibrocystic disease or adenosis in eight cases. In three other cases a radial scar, fat necrosis, and desmoplastic reaction were the cause of the enhancement and in one case lymphovascular invasion was seen. In nine overestimated cancers, core biopsy was performed before MR examination and in these cancers mean overestimation was 26.6 mm, compared to 10.5 mm in the cancers in which puncture was performed after MR examination (p=0.17237).
In 35 tumors, the time–intensity curves of the surrounding areas were measured. Kinetic results are summarized in Table 3. Most of the perilesional enhancing areas showed more than 100% enhancement, both in benign and in malignant lesions. Benign lesions enhanced even slightly more. Ten of the 30 malignant extensions showed a wash-out, but 17 of them showed a continuous enhancement. None of the benign enhancing areas showed a wash-out.
Discussion
In this study population, 101 of 297 (34%) malignant lesions had an enhancing surrounding area. Exact pathological correlation was possible in 92 cases. The present study revealed that enhancement around a cancer corresponded in 89.1% of cases with malignant pathology. This means that histopathological examination of all enhancing areas around a mass must be performed. Of all types of enhancing surrounding areas, 23.9% corresponded with invasive carcinoma, 16.7% with invasive and DCIS, and 49.3% with DCIS, including 35.5% EIC+ tumors. These findings are in concordance with a study of Mumtaz et al. where 42 of 53 cancers showed accompanying DCIS, 19 of which were EIC+. In their study, MRI showed an adjacent area of diffuse or linear enhancement around a mass in EIC+ tumors and the extent of enhancement correlated well with the extent of EIC [9]. Detection of ductal carcinoma around a mass is important as EIC+ carcinomas have a high recurrence rate [2]. On mammography, the majority of DCIS can be recognized as suspicious microcalcifications, but are often underestimated [10, 11]. On ultrasound, intraductal spread can be recognized as duct dilatation with or without intraductal contents, as a tubular structure, or as an area of architectural distortion [4]. Detection by MR mammography is lower for DCIS than for invasive carcinoma and sensitivities of 40–100% are described [12]. On the other hand, MRI is more accurate in determining the extent of a tumor than conventional imaging [12].
In our study, the surrounding enhancing area on MRI was exclusively due to enhancement of benign lesions or normal glandular tissue in only eight cases. In two more patients the enhancing area corresponded with LCIS and in one other lymphovascular invasion was seen around the carcinoma. Moreover, overestimation of more than 1 cm was seen in 17 cancers in our study, mostly due to fibrocystic disease or adenosis, or to normal glandular tissue. Mumtaz et al. also reported false-positive enhancement adjacent to 5 of 19 EIC+ tumors, in which histology showed atypical epithelial hyperplasia and sclerosing adenosis, the latter enhancing consistently [9]. A study by Satake et al. of 46 patients showed that MR mammography detected intraductal spread of breast cancer in 91% of cases, but tumor extension could not be evaluated in four cases because of strong enhancement of fibrocystic disease or normal glandular tissue [4]. In their study, lymphocytic infiltration and fibrosis associated with a tumor showed enhancement around the cancer as well. They suggested that morphologic characteristics of enhancement, such as segmental or linear distribution, could be helpful in differentiating between intraductal spread and benign lesions. Gilles et al. also reported that fibrocystic disease around intraductal carcinoma can be a source of overestimation [13].
Others proposed that evaluation of enhancement kinetics can help in differentiating between benign and malignant lesions [14]. With the present study, we cannot confirm this, because a limitation of our study is the small number of dynamic studies (n=35) and maximal enhancement measurement (n=28). This is due to different imaging techniques used in both cooperating centers. In center B the moment of maximal enhancement was not known and kinetic features of surrounding enhancing lesions were not assessed in all carcinomas. Another reason for the rather small number of dynamic studies is that some spiculae or ductal structures were too thin to obtain a good ROI, and partial volume effects of the unenhanced area might otherwise have been included in the ROI. Choi et al. reported on a new subtraction algorithm that can potentially replace the time–intensity profile analysis on user-selected ROI, which could solve this problem [15]. A combination of MR with fluorodeoxyglucose positron emission tomography (FDG-PET) could possibly decrease the false-positive results, as Walter et al. reported a high specificity of this technique in 42 breast lesions [16].
Conclusion
Enhancing areas including long spicules, a ductal pattern, noduli, or diffuse enhancement surrounding a carcinoma correlated with in situ or invasive extension of the carcinoma in 92.5, 89, 80 and 100%, respectively, of this study population. If breast-conserving treatment is planned, the preoperative MR mammography should be discussed carefully between the radiologist and the surgeon as he/she needs to know the presence and extent of the enhancing region surrounding a carcinoma. However, an enhancing surrounding area can be caused by benign pathology in a minority of cases and thus pathological diagnosis is necessary before performing an extensive wider excision or mastectomy.
References
Ghossein NA, Alpert S, Barba J, Pressman P, Stacey P, Lorenz E, Shulman M, Sadarangani GJ (1992) Breast cancer. Importance of adequate surgical excision prior to radiotherapy in the local control of breast cancer in patients treated conservatively. Arch Surg 127:411–415
Holland R, Connolly JL, Gelman R, Mravunac M, Hendriks JH, Verbeek AL, Schnitt SJ, Silver B, Boyages J, Harris JR (1990) The presence of an extensive intraductal component following a limited excision correlates with prominent residual disease in the remainder of the breast. J Clin Oncol 8:113–118
Pain J, Ebbs S, Hern R, Lowe S, Bradbeer J (1992) Assessment of breast cancer size: a comparison of methods. Eur J Surg Oncol 18:44–48
Satake H, Shimamoto K, Sawaki A, Niimi R, Ando Y, Ishiguchi T, Ishigaki T, Yamakawa K, Nagasaka T, Funahashi H (2000) Role of ultrasonography in the detection of intraductal spread of breast cancer: correlation with pathologic findings, mammography and MR imaging. Eur Radiol 10:1726–1732
Davis PL, Staiger MJ, Harris KB, Ganott MA, Klementaviciene J, McCarty KS Jr, Tobon H (1996) Breast cancer measurements with magnetic resonance imaging, ultrasonography, and mammography. Breast Cancer Res Treat 37:1–9
Kristoffersen Wiberg M, Aspelin P, Sylvan M, Bone B (2003) Comparison of lesion size estimated by dynamic MR imaging, mammography and histopathology in breast neoplasms. Eur Radiol 13:1207–1212
Wasser K, Sinn H, Fink C, Klein S, Junkermann H, Ludemann H, Zuna I, Delorme S (2003) Accuracy of tumor size measurement in breast cancer using MRI is influenced by histological regression induced by neoadjuvant chemotherapy. Eur Radiol 13:1213–1223
European Organization for Research and Treatment of Cancer (EORTC) breast cancer cooperative group (2000) EORTC manual for clinical research and treatment in breast cancer. EORTC breast cancer cooperative group, 4th edn. Excerpta Medica, Almere, The Netherlands
Mumtaz H, Hall-Craggs M, Davidson T, Walmsley K, Thurell W, Kissin M, Taylor I (1997) Staging of symptomatic primary breast cancer with MR imaging. Am J Roentgenol 169:417–424
Stomper PC, Connolly JL, Meyer JE, Harris JR (1989) Clinically occult ductal carcinoma in situ detected with mammography: analysis of 100 cases with radiologic–pathologic correlation. Radiology 172:235–241
Holland R, Hendriks JHCL, Verbeek A, Mravunac M, Schuurmans Stekhoven J (1990) Extent, distribution and mammographic/histopathologic correlations of breast ductal carcinoma in situ. Lancet 335:519–522
Orel SG, Schnall MD (2001) MR Imaging of the breast for detection, diagnosis and staging of breast cancer. Radiology 220:13–30
Gilles R, Zafrani B, Guinebretière JM, Meunier M, Lucidarme O, Tardivon A, Rochard F, Vanel D, Neuenschwander S, Arriagada R (1995) Ductal carcinoma in situ: MR imaging-histopathologic correlation. Radiology 196:415–419
Baum F, Fischer U, Vosshenrich R, Grabbe E (2002) Classification of hypervascularized lesions in CE MR imaging of the breast. Eur Radiol 12:1087–1092
Choi B, Kim HH, Kim EN, Kim BS, Han JY, Yoo SS, Park SH (2002) New subtraction algorithms for evaluation of lesions on dynamic contrast enhanced MR mammography. Eur Radiol 12:3018–3022
Walter C, Scheidhauer K, Scharl A, Goering U, Theissen P, Kugel H, Krahe T, Pi U (2003) Clinical and diagnostic value of preoperative MR mammography and FDG-PET in suspicious breast lesions. Eur Radiol 13:1651–1656
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Van Goethem, M., Schelfout, K., Kersschot, E. et al. Enhancing area surrounding breast carcinoma on MR mammography: comparison with pathological examination. Eur Radiol 14, 1363–1370 (2004). https://doi.org/10.1007/s00330-004-2295-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-004-2295-3