Abstract
We report diffusion-weighted (DW) MR findings for acute spinal cord ischemia in a 56-year-old patient. MR imaging obtained approximately 3 h after symptom onset demonstrated an area of hyperintensity on DW images, but no conspicuous signal abnormality on T2-weighted images in the conus medullaris. DW imaging of the spinal cord can contribute to the early detection of spinal cord vascular compromise.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The time required to establish a diagnosis of spinal cord infarction from neurological deficits varies because such a diagnosis is made mainly on the basis of clinical features. Conventional MR studies have been reported to contribute to the characterization of spinal cord ischemia [1, 2]. Additionally, the usefulness of the DW imaging technique for the early detection of spinal cord infarction has been anticipated, similar to the use of brain MR imaging for the detection of cerebral ischemic attacks [3–9]. In the present case, DW images revealed a signal abnormality in the spinal cord prior to conspicuous changes on T2-weighted images during the hyperacute phase.
Case report
A 56-year-old man was transferred to the emergency room of our institution at 12:15 because of the sudden onset of a lower back pain and gait disturbance. The patient first experienced these complaints shortly after becoming aware of a mild urinary disturbance, which had developed around 12:00.
A neurological examination in the emergency room, performed at 13:00, revealed muscle weakness in the bilateral lower extremities and a reduced sensation of coldness, pinpricks and touch below the knee. Sensations of vibration and position were normal. No patellar tendon reflex or Achilles tendon reflex were noted. Cerebrospinal fluid analysis was normal.
Radiographs of the lumbar spine showed no compressive deformity of the vertebrae or intervertebral disk space narrowing. A subsequent abdominal CT study showed no abdominal aortic aneurysm or dissection.
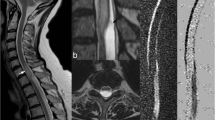
At 15:30, he was transported to the MR room for lumbar MR imaging. No conspicuous abnormal signal intensity was seen on spin-echo T1-weighted and fast spin-echo T2-weighted MR images. However, DW images revealed an area of hyperintensity in the conus medullaris. The mean apparent diffusion coefficient (ADC) measured 1.54±0.43×10−3 mm2/s in the abnormal signal region on DWI and 2.20±0.36×10−3 mm2/s in the adjacent normal-appearing region of the spinal cord (Fig. 1a–d).
A 56-year-old man with spinal cord infarction in the conus medullaris. a Sagittal diffusion-weighted MR image of the lumbar spine obtained approximately 3 h after the onset shows a focal hyperintense lesion (arrow). b ADC map shows a slight decrease of the cord intensity (arrow) in the abnormal area on the DW image. c Sagittal fast spin-echo T2-weighted MR image shows no significant signal alteration corresponding to the abnormality on the DW image. d Axial T2-weighted MR image at the level of the conus medullaris also shows no conspicuous signal abnormality. e Follow-up MR study performed 4 days after symptom onset reveals an area of hyperintensity in the swollen conus medullaris on T2-weighted image. f Axial T2-weighted MR image in follow-up study shows markedly increased intramedullary intensity compared with d
DW images were obtained on a 1.5-T scanner using a single-shot fast spin-echo (SSFSE) sequence, in which motion-probing gradients were applied in the cephalocaudal direction with b values of 0 and 400 s/mm2 [10]. Other scanning parameters for DW imaging were as follows: TR, 15,000 ms; TE, 100 ms; echo space, 6 ms; imaging matrix, 128×128; field of view, 30×30 cm; section thickness, 5 mm; NEX, 1; imaging time, 1 min and 30 s. No cardiac gating and respiratory compensation were used.
Treatment for the reduction of cord edema was started immediately after the diagnosis of spinal cord infarction, made on the basis of the clinical findings and supported by the MR imaging findings.
MR imaging performed 4 days after the onset showed spinal cord swelling on T1-weighted MR images and an area of hyperintensity in the conus medullaris on T2-weighted images (Fig. 1e,f). The bright area on DW images persisted. The mean ADC value in the lesion was 0.78±0.20×10−3 mm2/s.
A follow-up MR imaging performed approximately 1 month after symptom onset showed the resolution of the cord swelling on T1-weighted MR images. The hyperintense lesion in the conus medullaris had decreased in size on both T2-weighted and DW images. The mean ADC value in the abnormal signal area was 1.20±0.55×10−3 mm2/s.
A 3D phase-contrast MR angiography of the thoracolumbar spine showed no abnormal vascular structure. Post-contrast images were not obtained because the patient was on medication for bronchial asthma.
The muscle weakness in both legs improved after the 20th day of admission, and the patient became able to urinate voluntarily approximately 1 month after admission; the bilateral Achilles tendon reflexes had also normalized at that time.
Discussion
DW imaging of the spinal cord has been expected to enable the detection of spinal vascular compromise at an earlier stage than conventional MR studies. On conventional MR images, spinal cord ischemic lesions are demonstrated as areas of hyperintensity on T2-weighted images and cord swelling on T1-weighted images, although no signal abnormalities have been observed in the first 3 h after onset of clinical symptoms in the past literature [2]. Although several investigators have reported that DW imaging can depict spinal cord infarctions as hyperintense intramedullary signal abnormalities [4–9], their DW images were obtained at earliest 4 h after symptom onset [6]. In our case, the DW imaging of the spine was performed approximately 3 h after the onset. This is the earliest DW imaging acquisition time ever reported in the context of spinal cord ischemia. Even during the hyperacute phase, DW imaging conspicuously demonstrated an ischemic lesion in the spinal cord, despite the inconspicuous abnormality on T2-weighted images. The delayed alteration of the cord signal on follow-up T2-weighted MR images verified the implications of the abnormal DW imaging findings obtained during the initial MR study. Our observation reinforces the theoretical expectation that DW imaging could advance the time of detection of cytotoxic edema in hyperacute spinal cord ischemia, compared to conventional T2-weighted imaging [11].
We believe that the DW imaging results contributed to an early treatment in the present case, possibly leading to the subsequent clinical improvement. However, we should consider the possibility of false negative DW image in spinal cord ischemia, because a shortest time interval between symptom onset and positive DW image is still unknown. In addition, we should also be aware that a spinal cord lesion, which could lead to hyperintensity on DW image, may be other entities such as myelitis, neoplasms, multiple sclerosis and myelomalacia, although those have not been fully investigated using DW imaging.
As to DW imaging technique, we employed the SSFSE sequence described by Tsuchiya et al. [10]. This technique can be used for emergency DW study because it has an acceptable imaging time without requiring cardiac gating or respiratory compensation technique.
References
Yuh WTC, Marsh EE III, Wang AK, Russell JW, Chiang F, Koci TM, Ryals TJ (1992) MR imaging of spinal cord and vertebral body infarction. Am J Neuroradiol 13:145–154
Weidauer S, Nichtweiss M, Lanfermann H, Zanella FE (2002) Spinal cord infarction: MR imaging and clinical features in 16 cases. Neuroradiology 44:851–857
Moseley ME, Kucharczyk J, Mintrovitch J, Cohen Y, Kurhanewicz J, Derugin N, Asgari H, Norman D (1990) Diffusion-weighted MR imaging of acute stroke: correlation with T2-weighted and magnetic susceptibility-enhanced MR imaging in cats. Am J Neuroradiol 11:423–429
Stepper F, Lövblad KO (2001) Anterior spinal artery stroke demonstrated by echo-planar DWI. Eur Radiol 11:2607–2610
Fujikawa A, Tsuchiya K, Koppera P, Aoki C, Hachiya J (2003) Spinal cord infarction demonstrated on diffusion-weighted MR imaging with a single-shot fast spin-echo sequence. J Comput Assist Tomogr 27:415–419
Weidauer S, Dettmann E, Krakow K, Lanfermann H (2002) Diffusion-weighted MRI of spinal cord infarction. Description of two cases and review of the literature. Nervenarzt 73:999–1003
Loher TJ, Bassetti CL, Lövblad KO, Stepper FP, Sturzenegger M, Kiefer C, Nedeltchev K, Arnold M, Remonda L, Schroth G (2003) Diffusion-weighted MRI in acute spinal cord ischaemia. Neuroradiology 45:557–561
Sagiuchi T, Iida H, Tachibana S, Kusumi M, Kan S, Fujii K (2003) Case report: diffusion-weighted MRI in anterior spinal artery stroke of the cervical spinal cord. J Comput Assist Tomogr 27:410–414
Reich P, Muller-Schunk S, Liebetrau M, Scheuerer W, Bruckmann H, Hamann GF (2003) Combined cerebellar and bilateral cervical posterior spinal artery stroke demonstrated on MRI. Cerebrovasc Dis 15:143–147
Tsuchiya K, Katase S, Fujikawa A, Hachiya J, Kanazawa H, Yodo K (2003) Diffusion-weighted MRI of the cervical spinal cord using a single-shot fast spin-echo technique: findings in normal subjects and in myelomalacia. Neuroradiology 45:90–94
Sevick RG, Kanda F, Mintorovitch J, Arieff AI, Kucharczyk J, Tsuruda JS, Norman D, Moseley ME (1992) Cytotoxic brain edema: assessment with diffusion-weighted MR imaging. Radiology 185:687–690
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fujikawa, A., Tsuchiya, K., Takeuchi, S. et al. Diffusion-weighted MR imaging in acute spinal cord ischemia. Eur Radiol 14, 2076–2078 (2004). https://doi.org/10.1007/s00330-004-2284-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-004-2284-6