Abstract
The aim of this study was to assess the frequency and severity of respiration-induced curvilinear respiration artifacts (RICA) on co-registered positron emission tomography/computed tomography (PET/CT) images acquired on a combined PET/CT scanner before and after modifying the respiration protocol for CT scanning, with retrospective analysis of two groups of 100 patients each, before and after implementing a respiration protocol with breath-hold (BH) in the normal expiration position for the acquisition of the CT images. The CT data were used as attenuation map and for image co-registration. A ranking of co-registered PET/CT and PET images (including maximum intensity projection) was done by two observers in consensus using a scale from 0 to 3. Zero indicated that no RICA was visible and 1, 2, and 3 described artifact with increasing severity. A significant difference in RICA occurrence was found between the two groups (p<0.0001). There was a 45% decrease of artifact frequency when using the normal expiration protocol and a 68% decrease of grade-2 and grade-3 artifacts (p=0.004). The results of this study suggest that BH during the normal expiration position for CT scanning can be recommended to reduce the occurrence and the severity of RICA on PET/CT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Combined positron emission tomography/computed tomography (PET/CT) cameras have been recently introduced into clinical routine imaging. These devices allow for the fast and correct co-registration of anatomical and functional information in the same imaging session. Motion presents a challenge in the thoracic cage, and several studies have evaluated the influence of respiration on the quality of image co-registration [1, 2, 3, 4, 5]. It has been described that the acquisition of CT data during shallow tidal breathing (STB) can induce artifacts with a typical curvilinear shape cranial to both diaphragms on coronal PET and PET/CT images [6, 7]; therefore, we started to acquire CT data during breath-hold (BH) in the normal expiration position. This led to a better co-registration accuracy of thoracic lesions than CT scanning during STB [8]. Furthermore, there was an improvement in the quality of the attenuation correction map for the PET data.
The aim of this study was to evaluate the influence of BH during CT acquisition on the prevalence and intensity of respiration induced curvilinear artifacts (RICA) in a routine clinical setting.
Patients and methods
In order to assess image quality regarding the occurrence of RICA, we retrospectively reviewed the first 100 consecutive patients and the 100 most recent cases. The analysis of patient data was performed in accordance with the ethical guidelines of the institutional review board. The first 100 patients performed STB during CT acquisition (54 men and 46 women; mean age 56.0±16.5 years, age range 17–87 years). The 100 most recent cases were matched to the first group by age and gender (55 men and 45 women; mean age 54.5±15.6 years, age range 14–80 years) and were instructed to hold the breath in the normal expiration position during CT scanning. Breath hold was introduced approximately 3 months after the installation of the combined PET/CT scanner. The BH position was defined as the level reached when the patient exhaled without forcing expiration and then held the breath in this position. All patients were scanned for an oncologic disease and only PET examinations from adult patients were considered for this evaluation. Examinations of patients scanned in prone position, which is performed only for radiotherapy planning or in breast cancer patients, were not included for this study.
Imaging
All patient examinations were done on an integrated PET/CT device (Discovery LS, General Electric, Milwaukee, Wis.), which combines a full-ring PET camera with a multislice helical CT. The PET camera of this combined scanner has a 14.6-cm axial field of view (FOV) and a transaxial resolution of 4.8 mm full width at half-maximum at the center of the FOV. Patients fasted for at least 4 h prior to scanning which started approximately 45 min after the injection of 300–400 MBq of 18F-fluorodeoxyglucose (FDG). They were placed in the scanner in supine position and usually had their arms up when pathologies of the thorax or abdomen were scanned and their arms down if the pathology was at the head and neck level. The PET scans were acquired in 2D mode using an acquisition time of 4 min for the emission scan per cradle position with a one-slice overlap at the borders of the FOV to avoid artifacts. In all patients the CT scan was acquired with the built-in multislice detector CT scanner using the following parameters: 140 kV; 40 mAs; and a pitch of approximately 6 with a 512×512 matrix size. The CT acquisition from the head to the pelvic floor was done in 22.5 s and was acquired before the PET scan. The CT data were used for attenuation correction of the PET data as previously described and for image co-registration with the attenuation corrected final PET image [9].
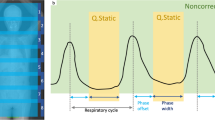
The BH protocol is shown in Fig. 1. The CT acquisition started at the head level, and at the same time, the instruction by the staff to stop breathing in the normal expiration position was given to the patient. This means that the patients inhaled normally when the CT scan started and then exhaled normally and held their breath in this expiration position. During the normal inhalation and exhalation the CT scan reached the upper thoracic inlet. Then, while the patient was on BH in the expiration position, the CT scan covered the lung to the upper abdomen. As soon as the abdomen was reached, the radiographer instructed the patient to continue normal shallow breathing. With this respiration protocol a patient had to hold the breath in the normal expiration position for approximately 10–15 s. This respiration task was explained but not trained before a patient was placed on the scanner.
The breath hold protocol for CT imaging. a The CT scan is done before the positron emission tomography (PET) scan and starts at the head level. At the same time the radiographer gives an instruction to hold the breath in the normal expiration position. b During the approximately 5 s until the patient reaches the breath hold position, the CT scan has reached the upper thoracic inlet and will continue to scan the thorax for a further 10 s. c As soon as the upper abdomen is reached the patient is instructed to continue shallow tidal breathing. d During the next 8 s the CT scan will cover the abdomen to reach the pelvic floor. The whole CT scan takes approximately 22 s
Analysis
The presence of RICA was visually assessed on the PET image, the co-registered PET/CT, and the maximum intensity projection (MIP) image. This MIP image allows for 3D display of a PET study and is routinely displayed using the implemented scanner software. On the black-and-white PET and MIP images dark areas corresponded to regions with an increased tracer uptake and bright areas to regions with low FDG uptake (white background). The assessment of the presence of a RICA and artifact intensity was performed by two experienced nuclear medicine physicians and disagreement was solved by consensus. Because the date of the examination was written on the images, the readers were not blinded to the respiration protocol used for CT acquisition. The scoring was done by looking first at the MIP image in an anterior–posterior view and then inspecting the PET images and the co-registered PET/CT images in coronal, sagittal, and transversal planes as displayed on the same screen. A numerical scale from 0 to 3 was used to rank the intensity of RICA. Zero indicated that no artifact was visible neither in the attenuation-corrected PET scan nor in the co-registered PET/CT image (Fig. 2a). An intensity of 1–3 described the presence of artifacts with increasing severity. The presence of a curvilinear white stripe over one or two diaphragmatic domes, which mimicked a decreased tracer uptake in the lower lung, was described as a grade-1 artifact. In the corresponding PET/CT image no relevant mismatch of PET and CT data was visible (Fig. 2b). A grade-2 artifact was defined as a clearly visible white stripe, which was always present above both diaphragmatic domes, and a corresponding mismatch of the upper edge of the liver and the adjacent lung in the co-registered PET/CT image (Fig. 2c). In grade-2 artifacts a decreased FDG uptake was often visible in the inferior myocardial wall and heart apex, when compared with the anterior wall of the heart and heart base (Fig. 2c). In these cases a bright stripe between the heart and the upper abdomen was always visible. Grade-3 artifact was defined as a wide bright stripe over the whole diaphragm with a severe decrease of FDG activity in parts of the myocardium and upper abdominal organs. In the corresponding PET/CT images a large mismatch of the upper abdominal organs and heart was visible (Fig. 2d). It has to be noted that a mismatch between PET and CT is usually more evident in posterior areas between lung and abdomen, because the diaphragmatic movements are larger in this region.
Ranking of respiration-induced curvilinear respiration artifacts (RICA). a A 67-year-old man with non-Hodgkin’s lymphoma and a mesenteric bulk (asterisk). The maximum intensity projection (MIP) image (left) and a coronal slice in PET (middle) and co-registered PET/CT images (right) at the heart level. In this example no RICA is visible, and this case was graded 0 indicating a perfect match between CT and PET. b A 57-year-old patient with laryngeal cancer (asterisk) and left cervical lymph node involvement. The MIP image is shown on the left. A coronal slice of a PET (middle) and co-registered PET/CT images (right) at the heart level reveal the presence of a curvilinear bright stripe along the left diaphragmatic dome and a bright spot between heart and right diaphragmatic dome (arrows). This case was ranked as grade-1 artifact. In this patient the match between CT and PET images is still visibly acceptable, but when using the CT data for attenuation correction, PET emission data along the diaphragmatic domes are already overcorrected. c A 70-year-old patient with bronchogenic cancer and bilateral mediastinal/peribronchial lymph node involvement (asterisks). In the MIP image (left) there is a bright stripe along the diaphragmatic dome and between the heart and abdomen, which is better visible in the coronal PET and co-registered PET/CT images (arrows, middle image). This patient was ranked a moderate artifact with a grade-2 intensity. The bright stripe between the heart and abdomen is not explained by fatty tissue. In other cases with high 18F-fluorodeoxyglucose (FDG) myocardial uptake there was a clear discrepancy of visible FDG uptake intensity between the inferior and anterior wall. In such cases there is usually some minor mismatch between CT and PET images visible mainly at the tip of the myocardium and the posterior border between liver and lung. d A 56-year-old woman with two echinococcus liver lesions (short arrows). In the MIP image (left) there is only a narrow bright stripe along the right diaphragmatic dome visible; however, this case was ranked a grade-3 artifact, because there is a severe mismatch visible in the combined PET/CT study between lung and liver with the echinococcal cysts being falsely located in the lung parenchyma. The three images on the right represent an identical coronal slice behind the heart level in a CT, PET, and co-registered PET/CT image revealing the mismatch of the echinococcus cyst (long arrows)
Fischer’s exact test was used to compare nominal variables between the two groups. In particular, the frequency of the visual presence of RICA and the frequency of moderate and severe artifacts (grades 2 and 3) was analyzed.
Results
Four patients performing STB and one performing BH had to be excluded due to the following reasons: paravenous injection leading to artifactual obscuration of the lung–liver interface (n=2); poststenotic middle-lobe pneumonia secondary to lung cancer and concomitant liver metastases (n=1); diffuse liver metastases in a melanoma patient with suspected diaphragmatic paralysis (n=1); and a patient with mesothelioma (n=1), all impairing assessment of RICA.
In the STB group 25 patients presented no RICA. Within the 75 studies showing an artifact, it was mild in 53 cases, moderate in 20 cases, and severe in 2 cases (Table 1). In the BH group, 59 patients showed no artifact. In the 41 cases with visible artifacts it was mild in 34 cases, moderate in 6 cases, and severe in 1case (Table 1).
There was an overall 45% decrease of artifact frequency from 75 to 41% of patients performing BH. Fischer’s exact test showed a significant difference in artifact frequency between the two groups (p<0.0001). A 68% decrease of severe RICA (grades 2 and 3) was found from 22% in STB patients to 7% in patients performing BH (p=0.004).
No significant artifact severity difference was found between the two groups when comparing only patients with grade-2 and grade-3 RICA with patients showing a grade-1 artifact (p=0.18).
Discussion
This study shows that the introduction of the BH respiration protocol reduces the frequency of RICA, especially, those with moderate and severe intensity. The BH respiration protocol is feasible in clinical work, and most patients can cooperate during the PET/CT study without problems. However, complying with the breathing protocol can be difficult for some patients and depends on many factors, such as the position in the camera, the disease state of the patient, and the CT scan acquisition time (part- or whole-body); therefore, it is important to meticulously prepare the PET/CT examination. The CT acquisition protocol used in our department was adapted to reduce the time of BH: the instruction to begin BH is given to the patient at the time when the CT scan is started. The CT scan takes a few seconds to cover the head and neck, a region which barely moves during a normal respiration cycle. The CT scan reaches the upper thoracic inlet when the patient reaches the normal expiration BH position (Fig. 1) and during the next 10 s the thorax will be scanned. This protocol improves the control of the CT acquisition at the thoracic level, including the upper abdomen. When reaching the upper abdomen, the patient can continue with STB. It has been previously shown, that the influence of the respiration protocol on the co-registration quality of lower abdominal structures is less important [10].
A potential disadvantage of the BH protocol is that the lower lung parts are not optimally filled with air leading to interpretation problems in patients with diffuse parenchymal lung disease or small focal lesions. One possible approach to overcome this problem is to acquire a second CT scan for the lung in the same imaging session. A CT scan from the head to the pelvic floor generates an effective dose of approximately 4 mSv due to the high pitch and low milliampere product of the acquisition protocol used for PET/CT at our institution; therefore, it would be possible to acquire a second CT scan from the lung in maximum inspiration position without excessively increasing the patient dose.
The use of the BH respiration protocol for CT acquisition of combined PET/CT scans is clinically feasible. It improves co-registration quality and avoids RICA when using CT data for attenuation correction; therefore, we recommend the use of this protocol in patients undergoing combined PET/CT scans.
References
Nehmeh SA, Erdi YE, Ling CC, Rosenzweig KE, Squire OD, Braban LE, Ford E, Sidhu K, Mageras GS, Larson SM, Humm JL (2002) Effect of respiratory gating on reducing lung motion artifacts in PET imaging of lung cancer. Med Phys 29:366–371
Visvikis D, Costa DC, Croasdale I, Lonn AH, Bomanji J, Gacinovic S, Ell PJ (2003) CT-based attenuation correction in the calculation of semi-quantitative indices of [(18)F] FDG uptake in PET. Eur J Nucl Med Mol Imaging 30:344–353
Beyer T, Antoch G, Blodgett T, Freudenberg LF, Akhurst T, Mueller S (2003) Dual-modality PET/CT imaging: the effect of respiratory motion on combined image quality in clinical oncology. Eur J Nucl Med Mol Imaging 30:588–596
Nakamoto Y, Tatsumi M, Cohade C, Osman M, Marshall LT, Wahl RL (2003) Accuracy of image fusion of normal upper abdominal organs visualized with PET/CT. Eur J Nucl Med Mol Imaging 30:597–602
Osman MM, Cohade C, Nakamoto Y, Marshall LT, Leal JP, Wahl RL (2003) Clinically significant inaccurate localization of lesions with PET/CT: frequency in 300 patients. J Nucl Med 44:240–243
Goerres GW, Kamel E, Heidelberg TN, Schwitter MR, Burger C, Schulthess GK von (2002) PET/CT image co-registration in the thorax: influence of respiration. Eur J Nucl Med Mol Imaging 29:351–360
Goerres GW, Burger C, Kamel E, Seifert B, Kaim AH, Buck A, Buehler TC, Schulthess GK von (2003) Respiration-induced attenuation artifact at PET/CT: technical considerations. Radiology 226:906–910
Goerres GW, Kamel E, Seifert B, Burger C, Buck A, Hany TF, Schulthess GK von (2002) Accuracy of image co-registration of pulmonary lesions in patients with non-small cell lung cancer using an integrated PET/CT system. J Nucl Med 43:1469–1475
Burger C, Goerres G, Schoenes S, Buck A, Lonn AHR, Schulthess GK von (2002) PET attenuation coefficients from CT images: experimental evaluation of the transformation of CT into PET 511 keV attenuation coefficients. Eur J Nucl Med Mol Imaging 29:922–927
Goerres GW, Burger C, Schwitter MW, Heidelberg TN, Seifert B, Schulthess GW von (2003) PET/CT of the abdomen: optimizing the patient breathing pattern. Eur Radiol 13:734–739
Acknowledgements
This work was supported by an award of the research and education fund of the European Association of Radiology, the European Respiratory Society, and the Nuklearmedizinische Stiftung für Wissenschaft und Forschung, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Juan, R., Seifert, B., Berthold, T. et al. Clinical evaluation of a breathing protocol for PET/CT. Eur Radiol 14, 1118–1123 (2004). https://doi.org/10.1007/s00330-003-2174-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-003-2174-3