Abstract
The aim of this study was to determine if a saline solution flush following low dose contrast material bolus improves parenchymal and vascular enhancement during abdominal multiple detector-row computed tomography (MDCT). Forty-one patients (24 men and 17 women; mean age 49 years, age range 27–86 years) underwent abdominal MDCT (collimation 4×5 mm, 15-mm table increment, reconstruction interval 5 mm, gantry rotation period 0.8 s) with a single- as well as with a double syringe power injector. Indication for examination were benign and malignant tumors and inflammatory diseases. Patients received 100 ml nonionic contrast material (300 mgI/ml) alone or pushed with 20 ml saline solution. Mean enhancement values for both protocols were measured in the liver, the spleen, the pancreas, the renal cortex, the portal vein, the inferior vena cava and the abdominal aorta. Double syringe power-injector protocol led to significantly higher parenchymal and vascular enhancement than single syringe power-injector protocol (p<0.05). The improvement in mean enhancement of the liver was 9±9 HU, of the spleen 8±10 HU, of the pancreas 7±9 HU, and of the renal cortex 8±20 HU. The improvement in mean enhancement of the portal vein was 10±17 HU of the inferior vena cava 8±13 HU and of the abdominal aorta 10±17 HU. The use of a double syringe power injector with saline flush following contrast material bolus significantly improves parenchymal and vascular enhancement during contrast-enhanced abdominal MDCT with low iodine doses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The advent of helical CT technology and the development of nonionic contrast material have had a significant impact on abdominal CT imaging. Using helical CT, the entire abdomen can be scanned in a single breath-hold, allowing a more consistent level of parenchymal and vascular enhancement throughout acquisition compared with conventional CT. With multiple-detector-row helical CT (MDCT) a further improvement in abdominal CT was achieved due to higher temporal and longitudinal spatial resolution compared to single-detector-row helical CT [1].
It is generally agreed that bolus injection of intravenous contrast material is advantageous with respect to increasing the visibility of hypovascular tumors by maximizing the difference in enhancement between the tumor and organ parenchyma [2, 3, 4]. Nonionic contrast material is preferably used, because it is better tolerated by patients [5, 6, 7].
Nonionic contrast materials have optimized scanning protocols and contrast enhancement; nevertheless, their high cost forces the radiologist to search for ways to decrease contrast material dose. In addition, dose reduction is also advantageous in patients with renal insufficiency and/or patients who require additional contrast material for other radiological examinations in close temporal proximity to abdominal CT. On the other hand, reduction of contrast material dose in abdominal CT results in a decrease of hepatic enhancement, which potentially decreases detection of hypovascular or hypervascular hepatic lesions; therefore, several authors have established lower limits to which contrast material could be reduced [8, 9, 10].
Although a saline solution flush after contrast material administration is well established in MR imaging, it has not yet been used in routine CT imaging. Flushing with saline solution avoids pooling of contrast material in the arm veins and in the injection system leading to better utilization of the contrast material bolus [11].
The purpose of this study was to assess whether a saline solution flush after a low-dose contrast material bolus of 30 g iodine dose improves parenchymal and vascular enhancement during abdominal MDCT compared with abdominal MDCT with the same contrast material dose without flushing.
Materials and methods
Patients
All patients who underwent abdominal CT between August and September 2001, and who had undergone a prior abdominal CT at our institution, were enrolled in this prospective study. As of August 2001, all CT studies were performed using a newly installed double-syringe power injector. Prior to this date, all studies were performed using standard single-syringe power injector. Our initial study population consisted of 53 patients who had undergone two abdominal CT studies, one without and one with saline flushing of the veins after contrast material injection. Informed consent for study protocol and dose of intravenous contrast material was obtained from all patients before each CT examination and the study was approved by our institutional review board. All patients fasted before the CT examinations. Patients with congestive heart disease (n=7) or ongoing chemotherapy during or between the examinations (n=5) were excluded from the study to avoid errors in measurement of contrast material enhancement due to change of cardiac output and progression or regression of fatty infiltration of the liver, respectively. The final study population consisted of 41 patients (24 men and 17 women; mean age 49 years, age range 27–86 years). The mean interval between the CT examinations was 153±93 days (range 6–372 days). There was no significant difference in body weight between the examinations (65.1±10.9 kg compared with 64.7±10.9 kg, p=0.13). Indication for abdominal CT were neoplasms of the gastrointestinal tract (n=13), primary liver tumors (n=10), neoplasms of the genitourinary tract (n=4), adenoma of the gallbladder (n=1), cholecystitis (n=1), choledocholithiasis (n=2), liposarcoma (n=1), Crohn’s disease (n=1), tuberculosis of the bone (n=1), abscess of the liver (n=2), pancreatitis (n=4), and diverticulitis (n=1).
Acquisition protocol
All CT scans were obtained with a LightSpeed QXi Scanner (GE, Milwaukee, Wis.) by using a 0.8-s gantry rotation period, an x-ray tube voltage of 120 kV, and a current of 200–230 mA. Scan pairs covered the diaphragm to the aortic bifurcation. An antecubital or proximal antebrachial vein was punctured with an 18-G intravenous catheter immediately before injecting contrast material in all examinations. Before the contrast material was administered, saline injections had been administered by hand with the patient’s arm in scanning position to ensure the successful cannulation of the vein. All acquisitions were performed with (a) 4×5-mm collimation, (b) 15-mm table increment (c) 5-mm section thickness, and (d) 5-mm reconstruction interval. The volume coverage was 24.9±3.8 cm. As standard dose for routine follow-up CT in patients without clinical evidence of recurrent disease at our department, a volume of 100 ml contrast material (Iomeron, 300 mgI/ml, Gerot, Vienna, Austria) was injected with a flow rate of 2.5 ml/s using a single-syringe power injector (Envision CT, Medrad, Indianova, USA), while with the double-syringe power injector (Injectron CT2, MedTron, Saarbruecken, Germany) the same dose of contrast material followed by a 20 ml saline solution flush was injected. All scans were performed with a 70-s delay after initiation of contrast material injection.
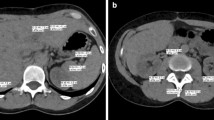
Quantitative evaluation of enhancement
Images of single-syringe power-injector protocol and double-syringe power-injector protocol were loaded on a workstation (MagicView 1100, Siemens, Erlangen, Germany) and viewed side by side on two monitors in random order. Monitor setting did not show patient data; consequently, the observer was blinded to the study date and thus to the power injector used. Loading processes and measurements were performed by different authors. Region of interest (ROI) measurements were performed for both protocols on corresponding slices in liver, spleen, pancreas, renal cortex, portal vein, inferior vena cava, and abdominal aorta aligned to anatomical landmarks to obtain mean contrast enhancement. The ROI settings in parenchymal organs were placed in areas without pathologic lesions that showed visually homogenous contrast material enhancement with exclusion of visible blood vessels. An attempt was made to maintain a constant ROI of approximately 1–2 cm2 in parenchymal organs and an ROI including nearly the whole vessel diameter, respectively. Table 1 shows the number of ROIs and the locations of ROI setting for the parenchymal organs and the vessels.
In 2 patients the liver was not measured because of fatty infiltration, which was defined as visually less enhancement of the liver compared with the enhancement of the spleen. In an additional 2 patients the spleen was not measured because of splenectomy, and in 4 patients the pancreas was not measured because of pancreatitis. The renal cortex, the portal vein, the inferior vena cava, and the aorta were measured in all patients.
Data analysis
Mean enhancement and standard deviation (mean±SD) of liver, spleen, pancreas, renal cortex, portal vein, inferior vena cava, and aorta were calculated per patient by averaging the single measurement values of each organ and vessel to compare the magnitude of parenchymal and vascular enhancement between both protocols. Furthermore, the mean enhancement of the superior and inferior liver segments and of the superior and inferior pole of the spleen and the kidneys were calculated per patient to compare the homogeneity of contrast enhancement between both protocols.
An attenuation value of 60 HU was assumed as average unenhanced hepatic attenuation to estimate the enhancement of the liver for both protocols by subtracting 60 HU from the mean attenuation value after contrast material administration. A hepatic enhancement of 50 HU was defined to be adequate [12].
We performed the Kolmogorov-Smirnov test for assessing normal distribution and the Levene’s test for assessing homogeneity of variances of the attenuation values. The significance of differences in mean enhancement values between both protocols was tested using the Student’s t test for paired samples. Two-tailed values were used and probability values of less than 0.05 were considered significant.
Results
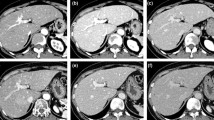
Saline solution flush following contrast material bolus led to statistically significantly higher parenchymal and vascular enhancement. The mean parenchymal enhancement was 8±12 HU higher with double-syringe power-injector protocol. Table 2 shows the attenuations values of both protocols and the differences in attenuation between both protocols for the parenchymal organs and the vessels. Figure 1 shows the relation of mean parenchymal and vascular attenuation between both protocols.
Relation of mean parenchymal and vascular enhancement (mean±SD) after contrast material administration for single-syringe power injector (triangles) and double-syringe power injector (squares). Double-syringe power-injector protocol produced statistically significantly higher enhancement values than single power-injection protocol (p<0.05)
There was no significant difference in mean enhancement along the z-axis for the parenchymal organs for both protocols. With the single-syringe power-injector protocol, the mean enhancement of the superior liver segments was 106±12 HU, of the inferior liver segments 105±11 HU (p=0.123). The corresponding enhancement values were 105±12 and 106±12 HU for the superior and inferior pole of the spleen (p=0.199) and 150±27 and 151±26 HU for the superior and inferior pole of the kidneys (p=0.451). With the double-syringe power-injector protocol, the corresponding enhancement values were 114±15 and 113±13 HU for the liver (p=0.128), 112±13 and 114±15 HU for the spleen (0.120), and 159±26 and 160±31 HU for the kidneys (p=0.316; Fig. 2).
Mean enhancement (mean±SD) of the superior pole (s) and inferior pole (i) of the liver, spleen and renal cortex for single-syringe power injector (triangles) and double-syringe power injector (squares). Note that there is no statistically significant difference in mean enhancement between superior and inferior pole of the organs (p<0.05)
Based on the assumption that the average attenuation of unenhanced hepatic parenchyma in our patient group was 60 HU (as attenuation values of normal liver parenchyma are approximately 50–70 HU), average enhancement after contrast material administration was greater with saline flushing (54±14 HU) than without flushing (45±11 HU). Sixty-one percent of patients showed adequate hepatic enhancement when flushing with saline compared with 32% without flushing with saline.
Discussion
Previous investigations have provided information about the effect of different doses of intravenous contrast material in helical CT of the abdomen and especially of the liver and about the minimum volume of intravenous contrast material required for abdominal CT [9, 10, 12, 13, 14, 15, 16, 17, 18]. Bluemke et al. [8], extrapolating from rabbit data, determined that a dose of 429 mgI/kg (using Iohexol 300) is the lowest dose to produce a hepatic enhancement of 30 HU, which is a low threshold of acceptability. This translates to 30 g iodine dose for a 70 kg person. On the other hand, Brink et al. [12] considered a maximum hepatic enhancement of more than 50 HU to be adequate. This enhancement was achieved with an iodine dose of 38 g in 70% of heavy patients (>83 kg) and with an iodine dose of 26 g in 70% of thin patients (<83 kg). Conversely, Freeny et al. [9] reported that a reduction of iodine dose from 45–48 to 30–32 g results in an average decrease of hepatic enhancement by 18 HU or 27%, which potentially decreases detection of focal hypovascular hepatic lesions. Megibow et al. [10] achieved hepatic enhancement above the standard of 30 HU over baseline with a standard dose of 1.5 ml/kg (using Iopromide 300). For a weight of 70 kg, this corresponds to an iodine dose of 31.5 g.
Summarizing these studies, the minimum dose of contrast material required for abdominal CT is approximately 26–30 g iodine. The aim of our study was to evaluate whether a 20-ml saline solution flush following a low-dose contrast material bolus (30 g iodine) improves the parenchymal and vascular enhancement during abdominal MDCT. A positive effect of saline solution flush in enhancement could compensate the decrease of enhancement, which occurs by dose reduction and thus may reduce the risk of missing hypovascular and hypervascular lesions in the abdominal organs.
We have studied the value of saline flush at low-dose CT and not at higher-dose CT for the following reasons: firstly, we hypothesized that the greatest benefit of a saline flush may be reached when using low contrast material doses, because conventional doses usually lead to adequate parenchymal attenuation even without saline flush. Secondly, we attempted to gain adequate parenchymal enhancement with the lowest possible contrast material dose to reduce the costs at our department.
To our knowledge, there are only a few studies which have investigated saline flushing in helical CT. A study reported by Hopper et al. [19] showed that using 75 ml of contrast material in thoracic CT, when pushed with saline solution, is equivalent to using 125 ml contrast material without flushing. In this investigation a single injector, in which the saline solution was loaded on top of the contrast material, was used. By contrast, we used a double-syringe power injector in our investigations with two separated interconnected injectors for contrast material and for saline solution and did not evaluate the effect of saline flush with the single syringe power injector, because loading one injector with contrast material and saline solution for each examination may be time-consuming and unfavorable in a busy department. Initially, the technologists had some minor problems with the loading procedure of the double-syringe power injector, but these problems could be solved within the first week of application.
Using a double-syringe power injector Haage et al. [20] performed a reduction from 75 to 60 ml of high concentration (370 mgI/ml) contrast material in helical CT of the thorax without significant difference in enhancement of the pulmonary trunk and the ascending aorta. Flushing with saline led to less pronounced enhancement in the superior vena cava and, thereby reducing perivenous artifacts; however, only one study evaluated the effect of a saline flush on aortic enhancement during abdominal CT. Sadick et al. [11] showed that in single detector-row-helical CT (SDCT) of the abdomen a saline solution flush of 20 ml prolongs the period of maximal aortal enhancement for 4 s, which may be useful in CTA. Parenchymal enhancement was measured for four protocols with different iodine dose and injection rate, each with saline flush after contrast material administration. Yet, this study did not evaluate the effect of a saline flush on parenchymal enhancement due to the lack of a control group without saline flush.
In our study we investigated the effect of saline flush following contrast material bolus in the same patient population by using a single-syringe power injector for the protocol without flush and a double-syringe power injector for the protocol with flush. The contrast material dose and the injection rate were kept constant for both examinations. Consequently, we avoided the measurement error that may be caused by a wide degree of individual variation. The difference in patient physiology and venous access, which may occur even when scanning the same patients at different times, could not be influenced.
All examinations were performed on the same MDCT scanner with the same scanning parameters, as using different CT scanners may result in measurement errors as reported by Levi et al. [21]. They reported significant differences in absolute Hounsfield units between most scanners even two scanners of the same manufacturer and model. We consider that as an important advantage of our study compared with other studies, where parenchymal enhancement was measured to evaluate different contrast material doses or injection rates using data of different patients and different CT scanners. The improvement of temporal resolution of MDCT enables scanning the abdomen during the peak plateau of contrast material enhancement. Consequently, we achieved a uniform contrast material enhancement of all parenchymal organs regardless of the position along the z-axis. There was no statistically significant difference in mean parenchymal enhancement of all liver segments and between the superior pole and the inferior pole of the spleen and the kidneys, respectively (Fig. 2).
The results of this study indicate that a saline solution flush following the contrast material bolus improves parenchymal and vascular enhancement during abdominal MDCT. A statistically significant improvement in mean parenchymal enhancement of 8 HU was achieved by flushing a 100-ml contrast-material bolus with 20 ml saline solution. Consequently, the decrease of parenchymal enhancement resulting from contrast material dose reduction (decrease of 18 HU by reducing from 45–48 to 30–32 iodine dose as shown by Freeny et al. [9]) could partly be compensated by flushing with saline solution in clinical routine. An increased aortic enhancement of 10 HU, as achieved in our study, may improve the detection of dissection flaps, thrombotic material, and atherosclerotic soft plaques in the abdominal aorta and its branches; however, a positive effect of saline flush on vascular enhancement may be more clinically relevant in abdominal CTA. Furthermore, higher flow rates of at least 4 ml/s are necessary in CTA, so CTA data have to be analyzed separately to evaluate the potential role of saline flush to extend the time of optimal vascular enhancement.
Generally, we try to keep the radiation exposure as low as possible; therefore, we do not perform unenhanced scans in routine follow-up abdominal CT examinations. The lack of unenhanced data to calculate true enhancement is a potential limitation of our study. We assumed an average attenuation of hepatic parenchyma in our patient population of 60 HU to estimate hepatic parenchymal enhancement. Based on this assumption an increase of enhancement of ~20% could be achieved when flushing with saline. The increase would be less pronounced if an average unenhanced hepatic attenuation towards 50 HU would be assumed. Following Brink et al. [12], who considered a hepatic enhancement of 50 HU as adequate enhancement, only 61% showed adequate hepatic enhancement even when flushing with saline (compared with 32% without flushing with saline). We consider the low-dose contrast material bolus as reason for the great percentage of inadequate hepatic enhancement.
A further limitation of the study is that the saline flush series was always performed later than the series without flushing. Results might be affected due to change in hepatic parenchyma between the examinations; however, there was no significant difference in patient’s weight between the examinations and patients with ongoing chemotherapy during or between the examinations were excluded from the study to minimize risk of progression or regression of fatty infiltration of the liver. In addition, the quantitative evaluation revealed similar differences in the mean contrast enhancement of the liver, the other organs, and the vessels between the studies (approximately 8 HU). So we consider hepatic changes between the examinations unlikely.
Conclusion
The results of our study demonstrate that using a double-syringe power injector with saline flush following contrast-material bolus significantly improves parenchymal and vascular enhancement during contrast-enhanced abdominal MDCT with low iodine doses, thereby reducing the risk of missing hypovascular and hypervascular lesions in the abdominal organs.
References
Rubin GD, Shiau MC, Schmidt AJ, Fleischmann D, Logan L, Leung AN, Jeffrey RB, Napel S (1999) Computed tomographic angiography: historical perspective and new state-of-the-art using multi detector-row helical computed tomography. J Comput Assist Tomogr 23 (Suppl 1):S83–S90
Chambers TP, Baron RL, Lush RM (1994) Hepatic CT enhancement. Part II. Alterations in contrast material volume and rate of injection within the same patients. Radiology 193:518–522
Chambers TP, Baron RL, Lush RM (1994) Hepatic CT enhancement. Part I. Alterations in the volume of contrast material within the same patients. Radiology 193:513–517
Kim S, Kim JH, Han JK, Lee KH, Min BG (2000) Prediction of optimal injection protocol for tumor detection in contrast-enhanced dynamic hepatic CT using simulation of lesion-to-liver contrast difference. Comput Med Imaging Graph 24:317–327
Debatin JF, Cohan RH, Leder RA, Zakrzewski CB, Dunnick NR (1991) Selective use of low-osmolar contrast media. Invest Radiol 26:17–21
Halpern JD, Hopper KD, Arredondo MG, Trautlein JJ (1996) Patient allergies: role in selective use of nonionic contrast material. Radiology 199:359–362
Hopper KD (1996) With helical CT, is nonionic contrast a better choice than ionic contrast for rapid and large IV bolus injections? Am J Roentgenol 166:715
Bluemke DA, Fishman EK, Anderson JH (1994) Dose requirements for a nonionic contrast agent for spiral computed tomography of the liver in rabbits. Invest Radiol 29:195–200
Freeny PC, Gardner JC, von Ingersleben G, Heyano S, Nghiem HV, Winter TC (1995) Hepatic helical CT: effect of reduction of iodine dose of intravenous contrast material on hepatic contrast enhancement. Radiology 197:89–93
Megibow AJ, Jacob G, Heiken JP, Paulson EK, Hopper KD, Sica G, Saini S, Birnbaum BA, Redvanley R, Fishman EK (2001) Quantitative and qualitative evaluation of volume of low osmolality contrast medium needed for routine helical abdominal CT. Am J Roentgenol 176:583–589
Sadick M, Lehmann KJ, Diehl SJ, Wild J, Georgi M (1997) Bolus tracking and NaCl bolus in biphasic spiral CT of the abdomen. Rofo Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr 167:371–376
Brink JA, Heiken JP, Forman HP, Sagel SS, Molina PL, Brown PC (1995) Hepatic spiral CT: reduction of dose of intravenous contrast material. Radiology 197:83–88
Hanninen EL, Vogl TJ, Felfe R, Pegios W, Balzer J, Clauss W, Felix R (2000) Detection of focal liver lesions at biphasic spiral CT: randomized double-blind study of the effect of iodine concentration in contrast materials. Radiology 216:403–409
Herts BR, Paushter DM, Einstein DM, Zepp R, Friedman RA, Obuchowski N (1995) Use of contrast material for spiral CT of the abdomen: comparison of hepatic enhancement and vascular attenuation for three different contrast media at two different delay times. Am J Roentgenol 164:327–331
Kim T, Murakami T, Takahashi S, Okada A, Hori M, Narumi Y, Nakamura H (1999) Pancreatic CT imaging: effects of different injection rates and doses of contrast material. Radiology 212:219–225
Small WC, Nelson RC, Bernardino ME, Brummer LT (1994) Contrast-enhanced spiral CT of the liver: effect of different amounts and injection rates of contrast material on early contrast enhancement. Am J Roentgenol 163:87–92
Yamashita Y, Komohara Y, Takahashi M, Uchida M, Hayabuchi N, Shimizu T, Narabayashi I (2000) Abdominal helical CT: evaluation of optimal doses of intravenous contrast material: a prospective randomized study. Radiology 216:718–723
Sandstede JJ, Tschammler A, Beer M, Vogelsang C, Wittenberg G, Hahn D (2001) Optimization of automatic bolus tracking for timing of the arterial phase of helical liver CT. Eur Radiol 11:1396–1400
Hopper KD, Mosher TJ, Kasales CJ, TenHave TR, Tully DA, Weaver JS (1997) Thoracic spiral CT: delivery of contrast material pushed with injectable saline solution in a power injector. Radiology 205:269–271
Haage P, Schmitz-Rode T, Hubner D, Piroth W, Gunther RW (2000) Reduction of contrast material dose and artifacts by a saline flush using a double power injector in helical CT of the thorax. Am J Roentgenol 174:1049–1053
Levi C, Gray JE, McCullough EC, Hattery RR (1982) The unreliability of CT numbers as absolute values. Am J Roentgenol 139:443–447
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schoellnast, H., Tillich, M., Deutschmann, H.A. et al. Improvement of parenchymal and vascular enhancement using saline flush and power injection for multiple-detector-row abdominal CT. Eur Radiol 14, 659–664 (2004). https://doi.org/10.1007/s00330-003-2085-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-003-2085-3