Abstract
Primary cardiac tumors are rarely diagnosed in utero and are usually seen on prenatal echocardiography. Cardiac rhabdomyomata can be associated with tuberous sclerosis. Prenatal MRI can be performed to assess associated malformations. This case report illustrates the ability of fetal MRI to image cardiac rhabdomyata and compares it with prenatal and postnatal echocardiography.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Fetal MRI using ultrafast sequences to suppress fetal motion artifacts allows a detailed visualization of the fetus in utero. Many studies have shown that fetal MRI is particularly helpful in the evaluation of the central nervous system [1, 2]. Imaging should always include the examination and evaluation of the entire fetus because congenital malformations and syndromes often present with pathology on several levels, involving multiple organs and functional systems [1]. We report the MRI and echocardiography findings obtained in a fetus at 31 weeks of gestation in comparison with postnatal echocardiography. To our knowledge, this is the first reported case on fetal cardiac rhabdomyomata visualized by MRI.
Case report
A routine obstetrical ultrasound examination of a 30-year-old pregnant woman at 31 weeks gestation showed multiple solid masses in the fetal heart. There were two tumors within the right atrium and ventricle and two smaller masses suspected in the left ventricle. Due to the multiplicity of the tumors, the most likely diagnosis was rhabdomyomata.
The mother’s previous medical history was unremarkable and pregnancy was uneventful. Fetal MRI was performed to rule out associated cerebral malformations or tumor. The MRI was performed at 1.5 T (Magnetom Vision, Siemens, Erlangen, Germany). The patient was positioned supine and examined using a body phased-array coil. The image acquisition was performed during multiple breath-holds in end-inspiration. After acquiring standard scout views, T2-weighted single-shot turbo spin-echo sequence (HASTE; TR=∞, TE 4.8 ms, 15 slices, slice thickness 5 mm, field of view 240×320, matrix 128×256) were measured in the axial, sagittal, and coronal orientation along the fetal abdomen, thorax, and brain. The MRI revealed two intracardiac masses within the right atrium and right ventricle (Fig. 1). The masses were almost isointense to the myocardium. Abdominal and cerebral fetal MRI was within normal limits and no other abnormalities or signs of tuberous sclerosis were noted. Fetal echocardiography (Fig. 2a) delineated both tumors as hyperechoic masses and suspected two additional intracardiac tumors suggestive of intracardiac rhabdomyomata. An asymptomatic baby was born at 36 weeks of pregnancy. Echocardiography performed on the second day of life demonstrated normal-size cardiac chambers with normal function and five hyperechoic intraluminal and intramyocardial solid tumors including one additional tumor in the left atrium (Fig. 2b). No other structural abnormalities within the brain and kidneys were found on ultrasound examination.
T2-weighted single-shot turbo spin-echo sequence in an axial orientation of the fetal chest showing the heart in a four-chamber view. a Within the right ventricular cavity a mass (arrow) can be identified. b A consecutive axial slice shows a second mass adherent to the right atrial wall (arrow). Additionally, thickening of the interventricular septum can be recognized, suspicious of additional intramural rhabdomyoma
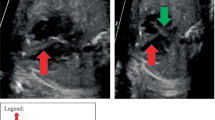
a Comparable slice position of fetal ultrasound at 31 weeks of gestation. Hyperechoic masses are well delineated in the right ventricular cavity and sessile at the right atrial wall (arrows). b Postnatal echocardiography displays the typical appearance of multiple cardiac rhabdomyomata in the right ventricle and right atrium (arrows), as well as in the interventricular septum (arrowheads)
After birth, tuberous sclerosis was confirmed by molecular genetic diagnosis. During a follow-up period of 10 months the child developed supraventricular arrhythmias including occasional couplets and transient third-degree atrioventricular block which were treated with antiarrhythmogenic drugs. Follow-up echocardiograms demonstrated normal biventricular function and constant cardiac rhabdomyomata in size and number. Abdominal and cerebral ultrasound remained normal.
Discussion
Primary cardiac tumors are rare findings in childhood with a reported incidence of 0.0017 to 0.027% [3] as well as in utero with a reported incidence of 0.009 [4] to 0.17% [5]. Beghetti and coworkers [6] reported an increase in recognition of cardiac tumors in children over a 15-year period from 0.06 to 0.32%. This was believed to be due to improved noninvasive imaging techniques and the adoption of more intensive routine screening of children with diagnosed suspected tuberous sclerosis. Rhabdomyoma is the most common cardiac tumor in the fetus and pediatric population which is followed in frequency by fibroma and teratoma [7]. Most rhabdomyomata are multiple, whereas fibroma and teratoma are most likely single. The differential diagnosis between fibroma and rhabdomyoma can be difficult, except when the tumor contains calcification, which was not the case in our patient. Teratomas are heterogenous, located in the pericardium, and fibromas are isoechogenic, round, often pedunculated [8]. Partial or complete spontaneous regression of rhabdomyomata has been reported in 60–100% and was seen in 54% during a follow-up of 5.4 years [6]; therefore, a conservative therapeutic approach is advocated to allow the rhabdomyomata to regress if they are not life threatening. The tumors are usually multiple, solid, and lobulated and an estimated 50–86% of rhabdomyoma cases are associated with tuberous sclerosis [9]. Tuberous sclerosis is a multisystemic disorder inherited as an autosomal-dominant trait and characterized by tumor-like malformations of the brain, skin, and visceral organs [10]. Cardiac rhabdomyomata in the fetus are the most frequently reported signs of tuberous sclerosis [9]. The earliest reported depiction of tumor is at approximately 20 weeks of gestation with a tumor growth spurt occurring between 22 and 32 weeks [11]. It has been reported that neonates with tuberous sclerosis may not develop any extracardiac signs until 1 year after birth [12]. Successful in utero diagnosis of intracerebral lesions indicating tuberous sclerosis by MRI [8, 13] and prenatal ultrasound [8, 14] has been reported, but there has never been a report on the diagnosis of intracardiac tumors by MRI in a fetus. Fetal echocardiography is a well-established tool for the prenatal diagnosis of structural and functional heart disease and is superior to fetal MRI in visualizing cardiac tumors. Further diagnostic imaging is usually not necessary with rhabdomyomata. Sonography shows that most rhabdomyomata are multiple and have a homogeneous echogenicity. The MRI is particularly useful for solitary tumors, because it assists in tissue characterization if different sequences are applied and helps define the relationship with normal structures.
The presented case demonstrates that MRI is capable of visualizing cardiac tumors in the fetal heart despite its limited spatial resolution. With the advent of fast, single-shot sequences, the motion of the fetus can be “frozen” [15] and artifacts are reduced. Currently, fetal MRI is a valuable tool to diagnose extracardiac manifestations of tuberous sclerosis in order to give as much information as possible to the parents for their decision-making process [16], and is performed as complementary, second-line diagnostic tool if additional information could influence obstetric management [17]. When fetal intracardiac rhabdomyoma is detected, cerebral MRI is required, and if there are pathognomonic lesions, a termination of pregnancy can be discussed [8]. In this setting, the investigating radiologist should be aware that a finding of signal alteration within the heart may be caused by a rhabdomyoma and that it may be associated with tuberous sclerosis. At present prenatal cardiac MRI is limited to single-shot imaging as performed in our case. Further advances in sequence technology may help to overcome present limitations and facilitate cardiac imaging by improving soft tissue contrast for better lesion detection and characterization.
References
Huisman TAGM, Martin E, Kubik-Huch R, Marincek B (2002) Fetal magnetic resonance imaging of the brain: technical considerations and normal brain development. Eur Radiol 12:1941–1951
Aggoun Y, Hunkeler N, Destephen M, Vial Y, Gudinchet F, Calame A, Payot M (1992) Cardiac rhabdomyomatosis and Bourneville’s tuberous sclerosis in the fetus: apropos of 2 cases. Arch Mal Coeur Vaiss 85:609–613
Kiaffas MG, Powell AJ, Geva T (2002) Magnetic resonance imaging evaluation of cardiac tumor characteristics in infants and children. Am J Cardiol 89:1229–1233
Yagel S, Weissmann A, Rotstein Z, Manor M, Hegsh J, Anteby E, Lipitz S, Achiron R (1997) Congenital heart defects: natural course and in utero development. Circulation 96:550–555
Pipitone S, Mongiovì M, Grillo R, Gagliano S, Sperandeo V (2002) Cardiac rhabdomyoma in intrauterine life: clinical features and natural history. A case series and review of published reports. Ital Heart J 3:48–52
Beghetti M, Gow RM, Haney I, Mawson J, Williams WG, Freedom RM (1997) Pediatric primary benign cardiac tumors: a 15-year review. Am Heart J 134:1107–1114
Kim TH, Kim YM, Han MY, Kim W, Oh M, Han K (2002) Perinatal sonographic diagnosis of cardiac fibroma with MR imaging correlation. Am J Roentgenol 178:727–729
Bonnamy L, Perrotin F, Megier P, Haddad G, Body G, Lansac J (2001) Fetal intracardiac tumor(s): prenatal diagnosis and management. Three case reports. Eur J Obstet Gynecol Reprod Biol 99:112–117
Elderkin RA, and Radford DJ (2002) Primary cardiac tumors in a pediatric population. J Paediatr Child Health 38:173–177
Geipel A, Krapp M, Gremer U, Becker R, Gembruch U (2001) Perinatal diagnosis of cardiac tumors. Ultrasound Obstet Gynecol 17:17–21
Nir A, Ekstein S, Nadjari M, Raas-Rothschild A, Rein AJJT (2001) Rhadbomyoma in the fetus: illustration of tumor growth during the second half of gestation. Pediatr Cardiol 22:515–518
Groves AM, Fagg NL, Cook AC, Allan LD (1992) Cardiac tumours in intrauterine life. Arch Dis Child 67:1198–1192
Sonigo P, Elmaleh A, Fermont L, Delezoide AL, Mirlesse V, Brunelle F (1996) Prenatal MRI diagnosis of fetal cerebral tuberous sclerosis. Pediatr Radiol 26:1–4
Sgro M, Barozzino T, Toi A, Johnson J, Sermer M, Chitayat D (1999) Prenatal detection of cerebral lesions in a fetus with tuberous sclerosis. Ultrasound Obstet Gynecol 14:356–359
Ertl-Wagner B, Lienemann A, Strauss A, Reiser MF (2002) Fetal magnetic resonance imaging: indications, technique, anatomical considerations and a review of fetal abnormalities. Eur Radiol 12:1931–1940
Girard N (2002) Fetal MR imaging. Eur Radiol 12:1869–1871
Huisman TAGM, Wisser J, Martin E, Kubik-Huch R, Marincek B (2002) Fetal magnetic resonance imaging of the central nervous system. Eur Radiol 12:1952–1961
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kivelitz, D.E., Mühler, M., Rake, A. et al. MRI of cardiac rhabdomyoma in the fetus. Eur Radiol 14, 1513–1516 (2004). https://doi.org/10.1007/s00330-003-2062-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-003-2062-x