Abstract
The aim of this study was to quantitatively assess non-calcified coronary artery plaques and to determine their predictive value for the detection of coronary artery disease (CAD). A total of 179 patients underwent a calcium screening examination and a contrast-enhanced multidetector-row computed tomography angiography (MDCT) of the coronary arteries for various indications. The traditional calcium scores were evaluated and all examinations were reviewed for the presence of non-calcified plaques with an attenuation of 0–130 Hounsfield units (HU). The number, mean attenuation, and volume of these non-calcified plaques were recorded. All patients also underwent conventional catheter angiography. Coronary calcium was detected in 73% (131 of 179) of the patients. Overall incidence of purely non-calcified plaques was 30% (53 of 179). In 27% of the patients (48 of 179) no calcium was detected; however, 15% of these patients without calcifications showed non-calcified plaques (7 of 48). Significant correlations were found between the volume of calcified plaques, volume of non-calcified plaques, and total plaque volume. There were significant differences in plaque composition comparing different risk factor profiles and different stages of CAD. Volumetric assessment of non-calcified coronary artery plaques is feasible using contrast-enhanced MDCT. Screening for non-calcified plaques identifies patients with signs of CAD that are missed in a calcium screening examination.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Atherosclerotic lesions are known to be very heterogeneous, depending on the progression of this systemic disease and on the vascular territory affected [1]. It is also known that plaque composition rather than the severity of a given stenosis predicts the patient's risk for an acute cardiac event [2]. Noninvasive imaging tools to depict these heterogenous types of plaques, to differentiate various plaque components, to detect early stages of atherosclerosis, and ideally to identify patients at risk are currently being investigated [3].
Computed tomography has become an established method for non-invasive and highly-sensitive detection of coronary artery calcifications [4]. Yet, calcified plaques are probably the result of repetitive plaque rupture and healing, causing shrinkage of the vessel lumen with subsequent stenosis [5]. Earlier stages of atherosclerosis without calcifications might be more prone to rupture, resulting in acute cardiovascular events [6]; however, this theory does not stand undisputed, as an autopsy study suggested that the degree of calcification was greatest for acute and healed plaque ruptures [7]. Recently, it was shown that CT has the potential to identify early, non-calcified plaques in vivo in various vascular territories such as the carotid arteries [8] and the coronary arteries [9, 10]. Various imaging features of non-calcified and calcified plaques depicted with CT correlate with histopathologic stages of atherosclerosis defined by the American Heart Association [11], as demonstrated in a recent ex vivo study on human hearts [12].
The purpose of this study was twofold: firstly, to investigate the incidence of non-calcified plaques as detected by MDCT and to determine the predictive value of these vessel wall changes for the detection of coronary artery disease; and secondly, to prove the feasibility of volumetric analysis of these plaques, and to give an insight into the composition of coronary artery plaque burden as detected by MDCT. Correlations between calcified and non-calcified plaques, as well as correlation to specific risk factor profiles and the stage of CAD, are described.
Materials and methods
Patient population
One hundred seventy-nine patients who had undergone non-contrast-enhanced calcium screening test and contrast-enhanced MDCT angiography of their coronary arteries for various indications between January 2001 and September 2002 were enrolled in this study (123 men, 56 women; age 61±12 years). Clinical indications for the CT examinations were heterogenous, including high risk factor profiles, typical or atypical anginal complaints, and known coronary artery disease. All patients had also undergone selective catheter angiography of the coronary arteries, independent from indication for the MDCT examination. Patients underwent cardiac catheterization and MDCT within 6±10 days. All CT studies were reviewed retrospectively, and MDCT and cardiac catheterization were performed for clinical reasons; therefore, no approval by the local ethics committee was needed. Patients were divided into three subgroups according to the grade of coronary artery disease as detected by catheter angiography. Grade 1 includes non-significant stenoses (<50%), grade 2 stenoses are between 50 and 75%, and grade 3 are significant stenoses (>75%). All CT studies were reviewed retrospectively. Calcium screening test, CT angiography, or cardiac catheterization were performed for clinical reasons; thus, no approval by the local ethics committee was needed. In all patients, the following epidemiological data and risk factors were recorded: age; gender; obesity; hypertension; diabetes; nicotine abuse; and hyperlipidemia.
Multidetector-row computed tomography
All investigations were performed on a four-detector-row CT scanner (Somatom Sensation 4, Siemens, Forchheim, Germany).
Calcium screening
The following parameters were used for the calcium screening examination: 4×2.5-mm collimation; 80 kV; 300 mA; 15- to 20-s scan time. Slices were reconstructed with 3-mm slice thickness and 1.5-mm overlap. No contrast material was applied.
MDCT angiography of the coronary arteries
For CT coronary angiography, the following parameters were employed: 4×1.0-mm collimation; 0.5-s rotation time; 120 kV; 400 mA, resulting in a total scan time of approximately 35–40 s to cover the entire heart. The data sets were reconstructed with contiguous 1.25-mm-thick images using a 0.7-mm increment. Spatial resolution of the reconstructed angiographic images was 0.6×0.6×1.25 mm. One hundred twenty milliliters of non-ionic contrast media (300 mg iodine, Solutrast 300, Schering, Berlin, Germany) were applied, with a flow rate of 3 ml/s, and contrast arrival time was estimated using a test bolus. The original axial slices and thin-sliding maximum intensity projections were used for analysis of the coronary arteries and for assessment of calcified and non-calcified plaques, respectively.
Quantification of coronary plaques
Calcified plaques
The calcium screening examinations were evaluated on the CT scanner's standard postprocessing workstation with a commercial calcium screening software [13] (Siemens Wizard, Siemens, Forchheim, Germany), using a threshold of >130 HU. The Agatston score [14], volume equivalent [15], and the total calcium mass [16] were measured as described before, and were recorded for each patient.
Non-calcified plaques
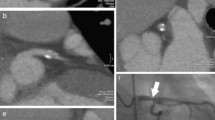
Non-calcified plaques were assessed quantitatively on an offline workstation (InSight, Neo Imagery, San Francisco, Calif.). The volumes of non-calcified plaques in the coronary artery wall were classified using thresholds of 0–130 HU. The outer border of the plaques was segmented manually, whereas the internal border between plaque area and contrast-enhanced vessel lumen was detected by the software and the plaque volume was calculated automatically (Fig. 1). The number, segmental location, and volumes of all non-calcified plaques, and the total non-calcified plaque volume burden per patient, were recorded.
Quantitative volumetry of non-calcified plaques. The quantitative volumetry was performed on an offline workstation (InSight, Neo Imagery, San Francisco, Calif.) The axial image at the height of the origin of the left coronary artery (left window) shows a large non-calcified plaque in the distal part of the left main coronary artery (arrow). Volumetry was conducted semi-quantitatively, segmenting the soft plaque borders by hand, whereas the software measured plaque volume automatically according to predefined thresholds (right window, see ellipsis for results)
According to the CT findings, the detected plaques were divided into three groups: purely calcified plaques (CP); mixed plaques (MP); and purely non-calcified plaques (NCP). Mixed plaques were defined as plaques with calcifications and non-calcified components in direct vicinity to each other. The quantification of non-calcified plaques was done only for the subgroup of patients, who presented real non-calcified plaques. In patients with mixed plaques, i.e., plaques consisting of calcified and non-calcified components, the volume of non-calcified plaque burden could not be assessed by the analysis software. The "total plaque volume", given in cubic millimeters, was defined as the sum of calcium volume equivalent and the volume of the non-calcified plaques.
Statistical analysis
Correlation and regression coefficients were calculated to test for significant correlations between calcified, non-calcified, and total plaque volumes. Dependency of calcified and non-calcified plaque numbers and plaque volumes on different grades of CAD and on indication for cardiac CT (suspected or known CAD) was tested using unpaired Wilcoxon tests. Dependency of analyzed plaque compositions as detected by CT on various risk factor profiles was assessed using a chi-square test. Continuous variables are presented as mean±standard deviation. For all statistical tests, a p value <0.05 was considered statistically significant.
Results
Predictive value of non-calcified plaques for the detection of CAD
Reviewing the calcium screening examinations and the CT angiography, the majority of patients (131 of 179, 73%) showed calcified plaques (CP) or mixed plaques (MP). In the remaining 27% (48 of 179) of the patients, no calcium was detected. In approximately one-third of all patients (53 of 179, 30%), purely non-calcified plaques (NCP) could be found, mostly together with calcified or mixed plaques at other sites of the coronary artery tree. In 41 patients, no signs of CAD were found in either the calcium scoring or the CT angiography (Fig. 2A).
Predictive value of non-calcified plaques for the detection of coronary artery disease. The figure shows the plaque distribution in A all patients (n=179) and in patients B without calcifications (n=48). Seven of 179 patients (i.e., 4%) showed non-calcified plaques only, without any calcifications detected in the calcium screening examination. cp calcified plaques, mp mixed plaques, ncp non-calcified plaques, no cad no plaques detected
Considering the 48 patients without calcifications, i.e., with a negative calcium screening, there was a considerable number (15%) of patients with non-calcified plaques among them, as detected in the contrast-enhanced CT scans (7 of 48 patients; Fig. 2B). In these 7 patients, CAD was diagnosed in the contrast-enhanced MDCT scan due to detection of non-calcified plaques, but would have been missed in the native calcium screening test. Catheter angiography of these 7 patients showed significant stenoses (>75%) in 3 cases, minor wall irregularities in 2 patients, and normal coronary artery lumen as depicted by catheter angiography in 2 cases.
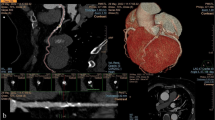
Correlation of calcified, non-calcified, and total plaque volume
The volume of non-calcified plaques did increase significantly with increasing total plaque volume (p=0.0105); however, the correlation was not very strong (r=0.3822; Fig. 3A). There also was a volume increase of non-calcified plaques in correlation to the calcium volume score, but it was not statistically significant (p=0.1583), and correlation was weak (r=0.2164; Fig. 3B). The percentage of non-calcified plaques decreased significantly with increasing total plaque volume (r=−0.5095, p=0.0004), i.e., in patients with high total plaque burden, the greater part of this plaque burden consisted of calcifications mainly (Fig. 3C). The volume score of calcified plaques showed a very strong correlation to total plaque volume (r=0.9849, r2=0.9700, p<0.0001; Fig. 3D). In small total plaque volumes, non-calcified plaques were over-represented, as shown by an intercept of +35 at the intersection of the regression line with the y-axis (p<0.0001; Fig. 3D, arrow).
Results of quantitative plaque assessment. A Correlation between volume of non-calcified plaques and total plaque volume. B Correlation between volume of non-calcified plaques and calcium volume score. C Percentage of non-calcified plaque volume vs total plaque volume. D Correlation between calcium volume score and total plaque volume
Dependency of plaque numbers on severity of CAD
For statistical analysis, an unpaired Wilcoxon test was performed, considering the number (mean and standard deviation) of calcified plaques (CP), mixed plaques (MP), and non-calcified plaques (NCP) per patient depending on the severity grade of CAD. The numbers of CAD grades 1 and 2 (6 and 8 patients, stenoses <75%) were pooled vs grade 3 (39 patients, stenoses >75%), to compensate for the small patient numbers in the first two groups. The mean number of calcified plaques increased significantly from grades 1 and 2 to grade 3, whereas the mean number of mixed and non-calcified plaques did not increase with statistical significance depending on the severity of CAD (Table 1).
Dependency of calcium scores and plaque volumes on severity of CAD
Table 2 shows quantitative values (mean and standard deviations) of calcifications (Agatston score, volume equivalent, calcium mass) and volumes of non-calcified plaques depending on the grade of CAD. Statistical analysis was performed using an unpaired Wilcoxon test (again, numbers of CAD grades 1 and 2 were pooled vs grade 3). Agatston score, volume equivalent, and absolute mass of calcified plaques as well as total non-calcified plaque volume increased significantly from grades 1 and 2 to grade 3.
Dependency of CT findings on cardiovascular risk factors
Risk factor profiles including gender, obesity, hypertension, diabetes, nicotine abuse, and hyperlipidemia were compared for different groups of pathologic CT findings [1=no pathology; 2=calcified and mixed plaques (cp and mp); 3=cp, mp, and non-calcified plaques (ncp); 4=ncp only; 5=all patients; Table 3]. Statistical analysis was performed using a chi-square test. The only risk factor that showed statistical significant increase was hyperlipidemia in the group of patients with calcified, mixed, and non-calcified plaques (p=0.0265). Pooling all patients with any pathologic CT finding vs patients without any pathology at CT indicated a significantly higher proportion of smokers in the pathology group (p=0.0490).
Discussion
Plaque morphology in CT
Screening examinations for coronary calcium, using EBCT or recently MDCT, have been widely accepted as a sensitive method to detect atherosclerosis of the coronary arteries in patients at risk or in patients with atypical chest pain. The negative predictive value of a negative calcium screening test has been reported to be in the range of 93–97% [17, 18]. Therefore, finding no coronary calcifications would exclude the presence of a significant CAD with a high probability; however, with the advent of contrast-enhanced CT of the coronary arteries, non-calcified vessel wall lesions become visible, and other stages of the disease, such as lipid-rich type-IV or type-Va plaques, become visible [11]. The density of these non-calcified lesions has been reported by independent groups and in various vascular territories to be between 0 and 130 HU, according to the content of lipid and fibrotic tissue, as proven by histopathology or intravascular ultrasound [8, 12, 19]. Non-calcified plaques with densities below 50 HU contain a higher amount of lipids, whereas mainly fibrotic lesions typically show densities between 50 and 130 HU. Density of lipid body tissue has been reported to be in the range of −250 to −50 HU [20]. The reasons for the higher densities of lipid-rich plaques as measured in the coronary artery wall are multiple. Firstly, the spatial resolution of MDCT is still limited; therefore, with a voxel size of 0.6×0.6×1.25 mm in four-detector-row CT, even a large lipid core of 500 μm will contribute to a maximum of 25–50% of the voxel, other components depicted will be a mixture of smooth muscle cells, endothelial cells, fibrotic tissue, and others. Secondly, the lipid core of atherosclerotic lipid-rich plaques consists of cholesterol lipids mainly, not of triglycerides as in body fat. The lowest Hounsfield units measured in our cohort in a lipid-rich plaque was 28±17 HU. The high standard deviations found may be due to the variety of tissue components combined in a single voxel; therefore, a reliable differentiation of fibrotic and lipid-rich plaques may not be possible using MDCT, due to an overlap of the densities measured and the complexity of the lesions. The densities measured can only give an evidence of the largest proportion of soft tissue components within the plaque.
Predictive value of non-calcified plaques for the detection of CAD
In our cohort of 179 patients, combining a non-contrast-enhanced calcium screening with a contrast-enhanced coronary angiography, 7 patients (4%) were identified with non-calcified plaques only, i.e., no calcifications were found in the calcium screening test. In these 7 patients, catheter angiography showed minor (stenoses <50%, 4 patients) or major (stenoses >75%, 2 patients) vessel lumen changes, but 1 patient had normal vessel lumen in catheter angiography and the presence of coronary atherosclerosis would have been missed by the gold-standard modality (Fig. 4). This specific subgroup of 7 patients showed an overall higher risk factor profile, with a higher percentage of nicotine abuse (83%), obesity (67%), hypertension (67%), and diabetes (50%; all 179 patients: 46, 28, 55, and 21%, respectively). Also, a lower mean age (55±10 vs 61±12 years) and a lower number of male patients (43 vs 68%) was characteristic for this cohort. Due to the small patient number in this subgroup, these differences were not statistically significant. Still, the non-contrast-enhanced calcium screening examination would have missed CAD in these patients, only after performing a CT angiography the correct diagnosis was made. Further characterization of such patients at risk for non-calcified plaques is essential for correct indication of contrast-enhanced MDCT angiography.
Example of a correct diagnosis made by multidetector-row computed tomography (MDCT) angiography. A 38-year-old man with a high cardiovascular risk factor profile and atypical angina underwent a calcium screening test, an MDCT coronary angiography, and conventional cardiac catheterization. The calcium screening examination was negative. No calcifications were found in the A coronary arteries (arrow), but after administration of contrast, a non-calcified plaque was detected in the B left main coronary artery (arrow). C Catheter angiography did not show any significant stenoses in this area, most probably due to "positive remodeling" effects (arrow)
Coronary plaque composition
In this study, we have shown that the volume of non-calcified plaques shows a positive correlation to total plaque burden and calcium burden, i.e., not surprisingly, non-calcified plaque burden increased with total plaque burden and with increasing calcium volume score; however, this increase of non-calcified plaque volume in correlation to the calcium volume score was not statistically significant, whereas there was a very strong correlation between total plaque volume and calcium volume score. These findings support the theory that the number and volume of non-calcified plaques are relatively high in patients with a low total plaque burden, as these non-calcified plaques may represent earlier stages of the disease, and therefore, many non-calcified lesions can be found. With constant progression of the disease, wall lesions tend to calcify; therefore, the total amount of calcium increases constantly with the progression of the disease, whereas new non-calcified lesions develop continuously, reflecting the activity of the disease [21]. This finding is also supported by the fact that the percentage of non-calcified plaque volume decreased with increasing total plaque volume, i.e., in patients with a high total plaque load, this high plaque load consists of calcified lesions mainly. This might explain that the total number of calcified plaques increased significantly with the severity of CAD, whereas the total number of non-calcified plaques did not increase significantly with higher grades of CAD, as shown in Table 1. It is known that in earlier stages of coronary atherosclerosis, the phenomenon of "positive (vascular) remodeling" maintains a constant vessel lumen [22, 23]. Various studies report that cardiac events were not inevitably associated with luminal narrowing detected by angiography [24, 25]. In later stages of the disease, significant stenoses will typically be associated with a higher amount of calcified and fibro-calcified plaques [26].
Limitations
Despite considerable recent improvement, multi-detector row CT still suffers from a limited spatial resolution. It is therefore difficult to visualize the coronary artery wall especially at distal segments of the coronary arteries, hampering a precise measurement of plaque volume. In this study, measurements were therefore limited to proximal and middle segments of the main vessels. In cases of heavily calcified coronary arteries, measurements of non-calcified plaques in direct neighborhood to calcifications will lead to an underestimation of the real non-calcified plaque volume, due to beam-hardening artifacts surrounding the calcifications, leading to higher Hounsfield units in the direct vicinity. That is why only purely non-calcified plaques have been assessed quantitatively, limiting the number of patients that underwent quantitative plaque volume analysis to 53 individuals. Also, the patient collective examined in this study and the indications for undergoing MDCT of the heart are somewhat heterogenous; however, the primary purpose of this study was to include a large cohort of patients, to assess the presence, predictive value, and quantitative assessability of non-calcified vessel wall changes in general. In future studies, precisely circumscribed patient cohorts with characteristic risk factor profiles or characteristic clinical presentations will have to be included, and differences in the presence and predictive value of various vessel wall lesions between these predefined patient groups, as detected by CT, will have to be described.
Conclusion
Several reports suggest that luminal narrowing as detected by conventional angiography is not unconditionally able to predict future cardiac events, and new imaging modalities are desirable to detect changes of the coronary arterial wall itself for early prevention of coronary events. Intravascular ultrasound is useful for the depiction of the coronary artery wall; however, it is an invasive technique and therefore not suitable for asymptomatic patients or as a screening tool. Examining coronary artery plaques by contrast-enhanced MDCT has the possibility of non-invasively detecting complex plaque morphology and of detecting earlier stages of coronary atherosclerosis as compared with a non-contrast-enhanced coronary calcium screening test. However, contrast-enhanced MDCT applies a higher amount of ionizing radiation to the patient; therefore, further technical improvement is desirable to decrease the radiation dose applied to the patient, such as ECG-controlled tube current modulation, which was shown to reduce the radiation dose applied by 48 and 45% for male and female patients, respectively [27].
This study demonstrated the ability of contrast-enhanced MDCT to quantitatively assess non-calcified vessel wall lesions of the coronary arteries in vivo. Furthermore, it could be shown that screening for these vessel wall changes will identify some patients with manifestations of CAD that would be missed in a calcium screening test; thus, in selected patient groups with characteristic risk factor profiles, an additional contrast-enhanced study should be performed, even if the calcium screening examination is negative. Further studies on larger cohorts will have to demonstrate the reproducibility of quantitative volume measurements of non-calcified plaques, e.g., for monitoring purposes under lipid-lowering therapy. Also, it has to be determined if and how the presence of non-calcified plaques influences the patient's outcome and which specific patients would most probably benefit from an additional contrast-enhanced study.
References
Fuster V, Fayad ZA, Badimon JJ (1999) Acute coronary syndromes: biology. Lancet 353 (Suppl 2):5–9
Pasterkamp G, Falk E, Woutman H, Borst C (2000) Techniques characterizing the coronary atherosclerotic plaque: influence on clinical decision making? J Am Coll Cardiol 36:13–21
Fayad ZA, Fuster V, Nikolaou K, Becker C (2002) Computed tomography and magnetic resonance imaging for noninvasive coronary angiography and plaque imaging: current and potential future concepts. Circulation 106:2026–2034
Becker CR, Knez A, Jakobs TF, Aydemir S, Becker A, Schoepf UJ et al. (1999) Detection and quantification of coronary artery calcification with electron-beam and conventional CT. Eur Radiol 9:620–624
Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM (2000) Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol 20:1262–1275
Virmani R, Burke AP, Farb A (2001) Sudden cardiac death. Cardiovasc Pathol 10:211–218
Burke AP, Taylor A, Farb A, Malcom GT, Virmani R (2000) Coronary calcification: insights from sudden coronary death victims. Z Kardiol 89 (Suppl 2):49–53
Oliver TB, Lammie GA, Wright AR, Wardlaw J, Patel SG, Peek R et al. (1999) Atherosclerotic plaque at the carotid bifurcation: CT angiographic appearance with histopathologic correlation. Am J Neuroradiol 20:897–901
Becker CR, Knez A, Leber A, Treede H, Haberl R, Reiser MF (2001) Angiography with multi-slice spiral CT: detecting plaque before it causes symptoms. MMW Fortschr Med 143:30–32
Becker CR, Knez A, Ohnesorge B, Schoepf UJ, Reiser MF (2000) Imaging of noncalcified coronary plaques using helical CT with retrospective ECG gating. Am J Roentgenol 175:423–424
Stary HC (2000) Natural history and histological classification of atherosclerotic lesions: an update. Arterioscler Thromb Vasc Biol 20:1177–1178
Becker CR, Nikolaou K, Muders M, Babaryka G, Crispin A, Schoepf UJ et al. (2003) Ex-vivo coronary atherosclerotic plaque characterization with multi-detector-row CT. Eur Radiol DOI 10.1007/s00330-003-1889-5
Becker CR, Knez A, Leber A, Hong C, Treede H, Wildhirt S et al. (2000) Initial experiences with multi-slice detector spiral CT in diagnosis of arteriosclerosis of coronary vessels. Radiologe 40:118–122
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Detrano F (1990) Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 15:827–832
Callister TQ, Cooil B, Raya SP, Lippolis NJ, Russo DJ, Raggi P (1998) Coronary artery disease: improved reproducibility of calcium scoring with an electron-beam CT volumetric method. Radiology 208:807–814
Hong C, Becker CR, Schoepf UJ, Ohnesorge B, Bruening R, Reiser MF (2002) Coronary artery calcium: absolute quantification in nonenhanced and contrast-enhanced multi-detector row CT studies. Radiology 223:474–480
Georgiou D, Budoff MJ, Kaufer E, Kennedy JM, Lu B, Brundage BH (2001) Screening patients with chest pain in the emergency department using electron beam tomography: a follow-up study. J Am Coll Cardiol 38:105–110
Lamont DH, Budoff MJ, Shavelle DM, Shavelle R, Brundage BH, Hagar JM (2002) Coronary calcium scanning adds incremental value to patients with positive stress tests. Am Heart J 143:861–867
Kopp AF, Schroeder S, Baumbach A, Kuettner A, Georg C, Ohnesorge B et al. (2001) Non-invasive characterisation of coronary lesion morphology and composition by multislice CT: first results in comparison with intracoronary ultrasound. Eur Radiol 11:1607–1611
Taguchi R, Takasu J, Itani Y, Yamamoto R, Yokoyama K, Watanabe S et al. (2001) Pericardial fat accumulation in men as a risk factor for coronary artery disease. Atherosclerosis 157:203–209
Stary HC, Chandler AB, Glagov S, Guyton JR, Insull W Jr, Rosenfeld ME et al. (1994) A definition of initial, fatty streak, and intermediate lesions of atherosclerosis: a report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Circulation 89:2462–2478
Glagov S, Weisenberg E, Zarins CK, Stankunavicius R, Kolettis GJ (1987) Compensatory enlargement of human atherosclerotic coronary arteries. N Engl J Med 316:1371–1375
Losordo DW, Rosenfield K, Kaufman J, Pieczek A, Isner JM (1994) Focal compensatory enlargement of human arteries in response to progressive atherosclerosis: in-vivo documentation using intravascular ultrasound. Circulation 89:2570–2577
Little WC, Constantinescu M, Applegate RJ, Kutcher MA, Burrows MT, Kahl FR et al. (1988) Can coronary angiography predict the site of a subsequent myocardial infarction in patients with mild-to-moderate coronary artery disease? Circulation 78:1157–1166
Giroud D, Li JM, Urban P, Meier B, Rutishauer W (1992) Relation of the site of acute myocardial infarction to the most severe coronary arterial stenosis at prior angiography. Am J Cardiol 69:729–732
Stary HC, Chandler AB, Dinsmore RE, Fuster V, Glagov S, Insull W Jr et al. (1995) A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis: a report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Arterioscler Thromb Vasc Biol 15:1512–1531
Jakobs TF, Becker CR, Ohnesorge B, Flohr T, Suess C, Schoepf UJ et al. (2002) Multislice helical CT of the heart with retrospective ECG gating: reduction of radiation exposure by ECG-controlled tube current modulation. Eur Radiol 12:1081–1086
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nikolaou, K., Sagmeister, S., Knez, A. et al. Multidetector-row computed tomography of the coronary arteries: predictive value and quantitative assessment of non-calcified vessel-wall changes. Eur Radiol 13, 2505–2512 (2003). https://doi.org/10.1007/s00330-003-2053-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-003-2053-y