Abstract
Developmental nasal midline masses in children are rare lesions. Neuroimaging is essential to characterise these lesions, to determine the exact location of the lesion and most importantly to exclude a possible intracranial extension or connection. Our objective was to evaluate CT and MRI in the diagnosis of developmental nasal midline masses. Eleven patients (mean age 4.5 years) with nasal midline masses were examined by CT and MRI. Neuroimaging was evaluated for (a) lesion location/size, (b) indirect (bifid or deformed crista galli, widened foramen caecum, defect of the cribriform plate) and direct (identification of intracranially located lesion components or signal alterations) imaging signs of intracranial extension, (c) secondary complications and (d) associated malformations. Surgical and histological findings served as gold standard. Nasal dermoid sinus cysts were diagnosed in 9 patients. One patient was diagnosed with an meningocele and another patient with a nasal glioma. Indirect CT and MRI signs correlated with the surgical results in 10 of 11 patients. Direct CT findings correlated with surgery in all patients, whereas the direct MRI signs correlated in 9 of 11 patients. In 2 patients MRI showed an intracranial signal alteration not seen on CT. Neuroimaging corrected the clinical diagnosis in 1 patient. One child presented with a meningitis. In none of the patients was an associated malformation diagnosed. Intracranial extension is equally well detected by CT and MRI using indirect imaging signs. Evaluating the direct imaging signs, MRI suspected intracranial components in 2 patients without a correlate on CT. This could represent an isolated intracranial component that got undetected on CT and surgery. In 9 patients CT and MRI matched the surgical findings. The MRI did not show any false-negative results. These results in combination with the multiplanar MRI capabilities, the different image contrasts that can be generated by MRI and the lack of radiation favour the use of MRI as primary imaging tool in these young patients in which the region of imaging is usually centred on the radiosensitive eye lenses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Developmental midline nasal masses in children are rare lesions. The incidence has been reported to be 1 in every 20,000–40,000 live births [1, 2, 3]. The most common masses include nasal dermal sinus cysts (NDSC), nasal gliomas and nasal encephaloceles. These congenital nasal masses are believed to result from a failure of embryological separation of neuroectodermal and ectodermal tissues during the development of the nose and frontobasis [3, 4]. These lesions are embryologically distinct, but all have an actual or potential intracranial extension/connection. The differential diagnosis includes abscesses, haemangiomas, fibromas, lipomas, granulomas and mucoceles [5, 6]. Neuroimaging is essential to characterise the lesion and to determine the exact location and possibly intracranial extent of the pathology. An adequate preoperative work-up is imperative to plan the appropriate therapeutic intervention and to avoid complications. Potential complications include a Molaret's type of chemical meningitis, infectious meningitis, abscess, osteomyelitis, cavernous sinus thrombosis, seizures and periorbital cellulitis [7]. Computed tomography and MRI have been proposed as valuable imaging tools in several reports [4, 6, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19]. The goal of our study was to determine the value of CT and MRI in the preoperative work-up of 11 children with midline nasal masses.
Materials and methods
We retrospectively reviewed the CT and MR imaging studies of 11 children who were referred for congenital midline nasal masses between January 1998 and July 2002 to our hospital. All patients were examined with CT or MRI to get information about the dignity of the finding as well as the exact location and possible intracranial extension of the lesion. Eight Children had simultaneous CT and MRI examinations.
Computed tomography scans were performed according to the standard institutional protocols including axial and coronal planes. The slice thickness varied between 1 and 3 mm. Intravenous or intrathecal contrast administration was not used in any study. Images were reconstructed in soft tissue and high-resolution bone algorithm.
Magnetic resonance imaging was performed on either a 2.0-T MRI unit (Tomikon S200, Bruker, Karlsruhe, Germany) or a 1.5-T MRI Unit (General Electric, Milwaukee, Wis.). T1-weighted spin-echo (SE; TR/TE/excitations: 300–450 ms/12–14 ms/4) and T2-weighted rapid acquisition with relaxation enhancement (RARE) SE (TR/TE: 3500–6000 ms/110–120 ms/2) sequences were acquired. Slice thickness varied between 2.5 and 4 mm, interslice gap between 0.5 and 0.8 mm. The field of view was adapted to the size of the patient's head. Multiplanar acquisition was performed in all children.
Images were studied for [1] lesion location, size and extension [2], direct and indirect signs of intracranial extension, [3] secondary complications and [4] associated malformations. Directs signs of intracranial extension refer to the identification of intracranially located components of the lesion or signal alterations. Indirect signs refer to changes in the normal anatomy of the frontobasis or neighbouring structures (bifid or deformed crista galli, widened foramen caecum, defect of the cribriform plate) [20]. The combination of a normal-sized and shaped or closed foramen caecum, a normal shaped crista galli and an intact cribriform plate were considered to exclude intracranial extension. The concomitant malformations that were evaluated included an absent septum pellucidum, agenesis of the corpus callosum, migrational and/or architectural abnormalities, midline facial defects, hydrocephalus and any kind of malformation related to a disturbance of the ventral cerebral induction [7]. In addition images were studied for possible secondary complications including superficial infection, periorbital cellulitis, epidural/subdural abscess, meningitis, cerebral abscess or osteomyelitis [7]. All CT and MRI scans were evaluated in concensus by at least two experienced paediatric neuroradiologists (J.S., E.M., T.H.). All children were operated on by a paediatric otorhinolaryngologist (D.H.). The results of surgical exploration and histological examination served as gold standard.
Results
The patient data as well as the clinical, neuroimaging and surgical results are summarized in Tables 1 and 2. The average patient's age at the time of examination was 4.5 years (ranging from 5 months to 20 years of age). The mean age of patients presenting with a NDSC was 4.5 years. The child with the meningocele obviously presented earlier, at 5 months of age. The child with a nasal glioma was 3.5 years. Nine children were male and two female. Nine children were diagnosed with an NDSC (Figs. 1, 2), 1 child with an meningocele (Fig. 3) and 1 child with a nasal glioma (Fig. 4). All patients with an NDSC showed a nasal pit. Two children showed a nasal obstruction (patients 5 and 6). The location of the swelling varied ranging from the midline position at the nasal dorsum or nasal root to the nasal vestibulum, medial nasal canthus and medial orbital canthus. Three children had suffered from recurrent infections with purulent discharge from the nasal pit (patients 3, 7 and 8). One child presented with a meningitis (patient 9). The child with the meningocele presented at 6 months with nasal obstruction due to a "polypoid intranasal mass". Clinically, a nasal glioma was suspected. The boy with a nasal glioma presented at 3.5 years with nasal obstruction due to a soft tissue mass in the nasal vestibulum. The family history was unremarkable for midline masses in all patients. Neither clinically nor by neuroimaging were associated congenital anomalies diagnosed.
An 18-month-old boy (patient 1) with a nasal dermal sinus cyst (NDSC). A Axial CT shows a midline soft tissue mass (arrow) with widening of the foramen caecum and the nasal septum. B Axial T2-rapid acquisition with relaxation enhancement (RARE) confirms an isointense soft tissue mass within the anterior nasal septum next to the foramen caecum (arrow). C Sagittal T1-weighted spin-echo (SE) images show the isointense soft tissue mass (lower arrow) near the anterior skull base with a questionable neighbouring intracranial, extradural component (upper arrow). D Coronal T2-weighted RARE confirms the anterior skull base defect or widened foramen caecum (arrows) as well as the bifid, eroded crista galli. On surgical exploration the cranial extension of the lesion was negative for neuroectodermal components and was diagnosed as a fibrous stalk
A 20-year-old man (patient 4) with an NDSC. A, B Axial CT shows a hypodense well-demarcated lesion at the right medio-lateral margin of the nose. The lesion is extending into the adjacent nasal bone. C Axial T2-weighted RARE and D coronal T2-weighted RARE images display a strongly hyperintense cystic NDSC. No intracranial extension was seen, and the nasal septum is not widened
A 3.5-year-old child (patient 6) with a nasal glioma. a Axial T1-weighted SE images show a small isointense soft tissue nodule within the left nasal vestibulum (arrow). The adjacent anatomy is unremarkable, the nasal septum is not widened or eroded. b Axial T2-weighted RARE with fat suppression reveals the T2-hypointense signal of the nodule (arrow)
Clinical diagnosis was confirmed by neuroimaging in 10 of 11 patients. In 1 patient (patient 5) the clinical diagnosis of a nasal glioma had to be corrected to an meningocele. The final histological diagnosis matched the diagnosis by neuroimaging in all patients.
Evaluating the individual indirect imaging signs (Table 2), CT and MRI were concordant in all patients. In 1 patient (patient 3) an erosion of a bifid crista galli that was displayed by CT was not seen on MRI. The bifid anatomy was, however, depicted equally good by both CT and MRI. By combining the indirect imaging signs, CT and MRI equally well predicted intracranial extension (10 of 11). In 1 patient (patient 1), both CT and MRI predicted intracranial extension which could not be confirmed at surgery.
Evaluating the direct imaging signs (Table 2), CT and MRI correlated with the surgical findings in 9 of 11 patients. The MRI showed, however, an intracranial, extradural signal alteration, indicating intracranial lesion location/extension, in 2 patients (patients 1 and 2) without a corresponding correlate on CT. In the first patient indirect imaging signs also indicated intracranial extension; in the second patient the indirect imaging signs did not support an intracranial lesion location/extension. In both patients the fistula was macroscopically followed by a fibrous stalk superiorly that was delivered and resected up to the foramen caecum. Microscopic analysis of the resected tissue confirmed the macroscopic findings. Because no direct intracranial extension was found, no intracranial surgical exploration was performed. Additional imaging findings included an eroded nasal bone in 3 patients (patients 1, 3 and 4), and a widened nasal septum in 2 patients (patients 1 and 3).
Discussion
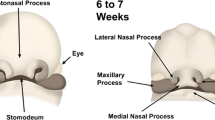
The complex embryological development of the nose with a close relation, interaction and finally separation of the neuroectoderm, mesoderm and surface ectoderm has been extensively studied, and many embryogenetic theories have been proposed [4, 5, 6, 7, 8, 18, 19, 21].
Despite the fact that currently no final consensus concerning the normal nasal development has been achieved, NDSC, nasal gliomas and encephaloceles are believed to share similar embryogenetic origins [7, 18, 19, 20, 21]. A failure of the normal separation of the different germ cell layers is considered to be causative. Consequently, all patients with developmental nasal masses must be considered as potentially having an intracranial extension [7, 18, 19, 20, 21]. Because surgical extirpation is considered to be the only method of managing patients with these lesions [2, 4, 19, 22, 23], a careful examination and radiological imaging is essential to determine the correct surgical procedure and to avoid complications.
Evaluating the current literature, no consensus exists as to which imaging modality is considered to be most advantageous. Both CT and MRI are considered to be essential, but to our knowledge, no final recommendation has been issued. From the surgical point of view, one of the most important questions to be answered is whether an intracranial extension is present. The chosen surgical approach will depend on this information.
Our results showed that the direct imaging signs for intracranial extension in CT matched the final surgical/histological findings in all patients. Considering the direct imaging signs, MRI appeared false positive in 2 children with NDSC. A subtle intracranial, extradural signal alteration was encountered on MRI that was not confirmed on surgical exploration (Fig. 1). This does not, however, necessarily indicate that CT is more accurate than MRI in excluding intracranial lesion components. Especially as in one of these 2 patients, the indirect CT and MRI imaging signs also suspected intracranial extension. More likely, these subtle extradural MRI signal abnormalities remained undetected by CT due to its lower soft tissue contrast. We speculate that intra- and extracranial lesion components can be simultaneously present despite an intact or unremarkable bony frontobasis. Two considerations are mentioned to underline this postulation. First of all, as stated previously, these lesions represent a spectrum of malformations along a common pathway of interaction and separation of the different germinal cell layers. Taking this into account, malformations with connected intra- and extracranial components and cases with solitary, either intracranial or extracranial, located lesions are theoretically expected to represent the extremes of this spectrum. Consequently, presentations should also be expected combining features of both extremes, which is the simultaneous appearance of an intracranial and extracranial component without a direct connection through the skull base. Secondly, the reliability of the so-called gold standard has to be reviewed in light of our first consideration. An intracranial extension is usually believed to be excluded if the cephalic end of the surgically removed extracranial nasal specimen or fibrous stalk is tested negative for ectodermal or neurogenic elements on multiple histological sections [24, 25]. Obviously, these results cannot exclude non-connected coexisting intracranial components; therefore, the consequences of these considerations are that the false-positive MRI findings in the first 2 patients with NDSC are maybe not false-positive findings but could represent definite pathology which got undetected by CT due to its lower soft tissue contrast resolution and by histology because this area was simply not explored. The clinical importance of these subtle extradural MRI findings are still to be studied, but it would mean that children should be followed-up after surgical removal of the extracranial mass to exclude a possible progression of intracranial MRI signal alterations.
At least three previous reports have evaluated the significance of indirect imaging signs concerning lesion extension. Pensler et al. reported 10 patients in whom an enlarged foramen caecum was taken as evidence of intracranial extension, with 7 of them having a bifid crista galli [24]. At craniotomy, however, none of the patients were found to have intracranial lesions. They concluded that abnormalities of the bony frontobasis alone should not be taken as an indication of intracranial extension without additional supportive evidence. Barkovich et al. [6] correlated the size of the foramen caecum and abnormality of the shape or bifidity of the crista galli in a healthy control group with a group of children with NDSCs. They concluded that these findings are only helpful when positive. Barkovich et al. [6] also discussed that the progressing ossification of the ethmoid bone and crista galli, as well as the accompanying fatty metamorphosis of the bone marrow, are known to mislead CT and MRI mimicking false-positive indirect imaging findings [20]. The age at which these modifications take place unfortunately match the age at which most of these lesions usually present. Bloom et al. [19] studied 10 patients with NDSC. They concluded that CT demonstrating an intracranial mass, bifid crista galli and widened foramen caecum is diagnostic for an intracranial extension in NDSC, whereas a normal size and appearance of the foramen caecum and crista galli appear to rule out intracranial extension; however, isolated widening if the foramen caecum and bifid crist galli are only suggestive for intracranial extension. They recommend that all cases of positive or indeterminate CT scan require an MRI, especially as they had no false-positive or false-negative MRIs in their series. Moreover, they recommend MRI as initial imaging for all children with the diagnosis of NDSC [19].
In our experience, the high-resolution CT bone algorithm reconstruction facilitates the evaluation of the foramen caecum, the crista galli and cribriform plate compared with MRI. This limitation is, however, compensated by distinct advantages of MRI, which include direct sagittal imaging planes and the possibility to generate multiple tissue contrasts (e.g. T1- vs T2-weighted sequences). Direct sagittal planes can allow the visualisation of the entire lesion including the intracranial communication [10]. The different signal intensities can be used to differentiate the dignity of the lesion. For example, T1- and T2-hyperintense components within a lesion indicate fatty inclusions as in an NDSC (Fig. 2), whereas a lesion that is T1- and T2-isointense to the cerebral grey matter is most likely a nasal glioma (Fig. 4). For example, T1- and T2-hyperintense intralesional signals indicate fatty inclusions as in an NDSC (patient 4). A lesion with a T1- and T2-signal isointense to grey matter indicative of a nasal glioma (patient 6). Moreover, additional MR angiographic sequences can help to differentiate nasal gliomas from capillary haemangiomas. This differentiation can be difficult on clinical inspection as Hoeger et al. reported previously [21]. In addition, partial-volume effects with the adjacent dense ossified frontobasis can hide small extradural lesions in CT. Because the bony frontobasis is hypointense in MRI, small extradural, intracranial lesions near the skull are more easily identified on MRI. Finally, advances in MRI hard- and software allows to image the frontobasis with a progressive spatial resolution that allows to examine the foramen caecum, crista galli and cribrifom plate in a detail similar to high-resolution CT. In our study, the indirect CT and MRI imaging findings matched in all patients. No lesions were seen by CT that was not seen by MRI, and vice versa. The question concerning intracranial extension was based on the indirect imaging signs, answered similarly by CT and MRI. Consequently, our study could not support the hypothesis that CT is more advantagous than MRI in the evaluation of developmental nasal midline masses.
In none of our patients was an associated malformation encountered. This is in concordance with the findings of Bloom et al. [19] who demonstrated a 0% incidence of associated intracranial anomalies. Previous reports described the incidence of associated anomalies in the range between 5 and 41% [7]. The NDSCs are reported in conjunction with other anomalies in up to 41% of the cases [26], meningo-encephaloceles often show associated brain anomalies as well as ocular anomalies [6, 27]. The NDSCs often become infected; 11% of patients with a NDSC present with superficial bacterial infections. In our series 3 children had suffered from recurrent superficial infections of the NDSC. Frontal lobe abscesses occur in 33% of patients with an intracranial connection [8]. In our series, only one child suffered from a severe complicating meningitis (patient 9; meningitis). The superior soft tissue resolution of MRI compared with CT is known to be very advantageous in diagnosing these complications.
One of the most important advantages of MRI compared with CT is the lack of ionizing radiation for imaging. This is especially important in this usually young patient population in which the radiosensitive eye lenses are exactly within the field of imaging. This lack of radiation is especially important in children who need follow-up imaging.
Conclusion
Developmental midline nasal anomalies are rare lesions that result from a failure of embryological separation of neuroectodermal and ectodermal tissue. Neuroimaging is essential in determining the dignity of the lesion and their possible intracranial extension. Direct and indirect imaging findings will guide surgical intervention. Our study showed that CT and MRI are equally sensitive in the detection of the extracranial mass; MRI can, however, show intracranial, extradural signal abnormalities without a coexisting bony abnormality of the frontobasis and without a corresponding CT finding. The exact meaning of these signal changes has to be determined in future studies. Both CT and MRI seem equally sensitive in the detection of indirect imaging findings despite the fact that CT delineates the bony frontobasis in more detail. Ongoing advances in hard- and software have increased the spatial resolution of MRI continuously allowing to study the bony frontobasis with similar precision to that of high-resolution CT. The major advantages of MRI include the multiplanar imaging planes, different tissue contrasts and most importantly the lack of ionizing radiation in this young patient population in which the pathology is located at the level of the orbits/eye lenses. We believe that the advantages of MRI outweigh the disadvantages and consequently should be used as primary imaging tool in the work-up of developmental nasal midline masses. Future studies with high-resolution pre- and postcontrast MRI studies with fat-suppression techniques are expected to further increase the diagnostic accuracy.
References
Pratt LW (1965) Midline cysts of the nasal dorsum: embryologic origin and treatment. Laryngoscope 75:968–980
Hughes GB, Sharpino G, Hunt W, Tucker HM (1980) Management of the congenital midline nasal mass: a review. Head Neck Surg 2:222–233
Paller AS, Pesnler JM, Tomita T (1991) Nasal midline masses in infants and children. Laryngoscope 107:795–800
Harley EH (1991) Pediatric congenital nasal masses. Ear Nose Throat J 70:28–32
Morgan DW, Evans JN (1990) Developmental nasal anomalies. J Laryngol Otol 104:394–403
Barkovich AJ, Vandermarck P, Edwards MS, Cogen PH (1991) Congenital nasal masses: CT and MR imaging fetaures in 16 cases. Am J Neuroradiol 12:105–116
Zerris VA, Annino D, Heilman CB (2002) Nasofrontal dermoid sinus cyst: report of two cases. Neurosurgery 51:811–814
Paller AS, Pensler JM, Tomita T (1991) Nasal midline masses in infants and children: dermoids, encephaloceles, and gliomas. Arch Dermatol 127:362–366
Hoving EW (2000) Nasal encephaloceles. Childs Nerv Syst 16:702–706
Fornadley JA, Tami TA (1989) The use of magnetic resonance imaging in the diagnosis of the nasal dermal sinus-cyst. Otolaryngol Head Neck Surg 101:397–398
Posnick JC, Bortoluzzi P, Armstrong DC, Drake JM (1994) Intracranial nasal dermoid sinus cysts: computed tomographic scan findings and surgical results. Plast Reconstr Surg 93:745–754
Lindbichler F, Braun H, Raith J, Ranner G, Kugler C, Uggowitzer M (1997) Nasal dermoid cyst with a sinus tract extending to the frontal dura mater: MRI. Neuroradiology 39:529–531
Burrows PE, Laor T, Paltiel H, Robertson RL (1998) Diagnostic imaging in the evaluation of vascular birthmarks. Dermatol Clin 16:455–488
Rouev P, Dimov P, Shomov G (2001) A case of nasal glioma in a new-born infant. Int J Pediatr Otorhinolaryngol 58:91–94
Jartti PH, Jartti AE, Karttunen AI, Paakko EL, Herva RL, Pirila TO (2002) MR of a nasal glioma in a young infant. Acta Radiol 43:141–143
Verney Y, Zanolla G, Teixeira R, Oliveira LC (2001) Midline nasal mass in infancy: a nasal glioma case report. Eur J Pediatr Surg 11:324–327
Oddone M, Granata C, Dalmonte P, Biscaldi E, Rossi U, Toma P (2002) Nasal glioma in an infant. Pediatr Radiol 32:104–105
Schlosser RJ, Faust RA, Phillips CD, Gross CW (2002) Three-dimensional computed tomography of congenital nasal anomalies. Int J Pediatr Otorhinolaryngol 65:125–131
Bloom DC, Cavalho DS, Dory C, Brewster DF, Wickersham JK, Kearns DB (2002) Imaging and surgical approach of nasal dermoids. Int J Pediatr Otorhinolaryngol 62:111–122
Denoyelle F, Ducroz V, Roger G, Garabedian EN (1997) Nasal dermoid sinus cysts in children. Laryngoscope 107:795–800
Hoeger PH, Schaefer H, Ussmueller J, Helmke K (2001) Nasal glioma presenting as capillary haemangioma. Eur J Pediatr 160:84–87
Loke DKT, Woolford TJ (2001) Open septorhinoplasty approach for the excision of a dermoid cyst and sinus with primary dorsal reconstruction. J Laryngol Otol 115:657–659
Bilkay U, Gundogan H, Ozek C, Tokat C, Gurler T, Songur E, Cadg A (2001) Nasal dermoid sinus cysts and the role of open rhinoplasty. Ann Plast Surg 47:8–14
Pensler JM, Bauer BS, Naidich TP (1988) Craniofacial dermoids. Plast Reconstr Surg 82:953–958
Brydon HL (1992) Intracranial dermoid cysts with nasal dermal sinuses. Acta neurochir (Wien) 118:185–188
Wardinsky TD, Pagon RA, Kropp RJ, Hayden PW, Clarren SK (1991) Nasal dermoid sinus cysts: association with intracranial extension and multiple malformations. Cleft Palate Craniofac J 28:87–95
Rapport RL II, Dunn RC Jr, Alhady F (1981) Anterior encephalocele. J Neurosurg 54:213–219
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huisman, T.A.G.M., Schneider, J.F.L., Kellenberger, C.J. et al. Developmental nasal midline masses in children: neuroradiological evaluation. Eur Radiol 14, 243–249 (2004). https://doi.org/10.1007/s00330-003-2008-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-003-2008-3