Abstract.
There is a potential hazard during examinations of patients with attached or implanted long conductors, e.g. ECG leads: an MR exam of the lumbar spine of a patient was performed in a 1.5-T scanner under ECG monitoring using equipment marked as MR compatible. Standard cabling of 370-cm length was guided without loops from the electrodes through the caudal opening of the magnet bore. During a sagittal T1-weighted turbo-spin-echo scan suddenly a flame of approximately 3 cm arose from the patient's shirt, close to the position of the electrodes. The supervising anaesthesiologist extinguished the flames with his hands. A subsequent physical examination revealed second- to third-degree burns. The analysis of the incident revealed that high voltages can be induced in straight conductors without loops as ECG cables by coupling with the electric component of the HF field. Local heating or sparking can cause an open flame at the position of the electrodes. This danger exists even with ECG equipment that is specifically marked as MR compatible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During MR examinations on patients, the main danger of the HF field is usually attributed to the induction of currents by the magnetic component B1 of the HF field in conductive loops. In early surveys on safety issues there were several reports of first- to third-degree burns resulting from MR exams which were attributed to heating caused by induction [1, 2, 3].
The literature on ECG monitoring during MRI contains little information other than the guideline to avoid loops in the leads and conductive loops formed by conductors with skin contact at two places [2, 4]. Also, safety guidelines of manufacturers of MR compatible physiological monitoring equipment require that all cables should be positioned straight inside the MR bore, without loops, and not touching the patient. In general practice ECG monitoring is considered safe if the setup is MR compatible and the electrodes are fixed in a proper way.
Recently, the effect of the HF field on long conductive structures has been investigated more systematically in guide wires [5, 6, 7], trans-oesophageal stimulation electrodes [8], pacemaker electrodes [9] and electrodes for deep brain stimulation [10, 11]. It was shown that long conductors couple with the electric component E1 of the HF field created in the transmit coil. High voltages can be induced near the wire ends and cause local heating.
Our observations demonstrate that coupling with the electric field is relevant even with ECG equipment marked as MR compatible and may lead to hazardous situations.
Case description
A 57-year-old male patient (75-kg body weight) received a postoperative MR exam of the pelvis and the lumbar spine. The MR measurements were performed in a 1.5-T Gyroscan Intera scanner equipped with Master gradients (30 mT/m, 150 mT/m ms−1) (Philips, Best, The Netherlands). The patient was positioned in the MR scanner on the standard synergy spine coil, a flat phased-array coil with five elements for spinal examinations. Due to the patient's poor condition, ECG monitoring had to be performed. The built-in ECG-triggering system of the scanner was not used. Instead, ECG monitoring was performed using a "Tesla plus" system (type EFTES03D, Mammendorfer Institut für Physik und Medizin (MIPM), Mammendorf, Germany). This monitor is an element of the MR compatible anaesthesia setup "NMR" with components from Draeger (Lübeck, Germany) and MIPM (Mammendorf, Germany). Three MR compatible Ag/AgCl gelled ECG electrodes (Conmed Corp., Utica, N.Y.) were fixed onto the right upper hemithorax. The ECG signals were guided through standard cabling that was delivered with the monitor and marked as MR compatible. The cable consisted of a 96-cm-long three-wire ECG cable (type EFMRZ030A, MIPM, Mammendorf, Germany), which was twisted in the central portion of 80 cm. It was connected to a 276-cm-long shielded extension cable (type EFMRZ041, MIPM, Mammendorf, Germany; approved for 0.2/0.5/1.5-T MR scanners). The resistance of the ECG cable was 2.5 ohm/cm, giving a total of 240 ohm, and the resistance of the extension cable was 3 ohm/cm, giving a total of 828 ohm. All cabling was guided without loops through the caudal opening of the magnet bore. As suggested by the user manual for the equipment, this cable was plugged into the monitor, which was positioned on a nonmagnetic trolley approximately 2 m away from the magnet where the magnetic stray field was below 20 mT. It was connected to a 230-V AC wall outlet with ground contact within the HF shielded room.
The examination commenced with MR scans of the pelvis. The pelvis of the patient was positioned in the isocenter of the magnet. Following a localizer sequence [turbo field echo; TR/TE/flip angle=7.6 ms/4.6 ms/25°, a total of 11 sections in three orientations,15 mm thick, field of view (FOV) 520 mm, scan duration 11 s], an axial T1-weighted scan [turbo spin echo; TR/TE/flip angle=600 ms/8 ms/90°, FOV 450 mm, acquired matrix 168×336 pixel, 30 sections 7 mm thick, gap 1 mm, echo train length (ETL) 3, one 60-mm-thick transverse saturation slab, scan duration 3 min 27 s), and an axial sagittal proton-density-weighted scan (SE; TR/TE/flip angle=1296 ms/15 ms/90°, FOV 450 mm, acquired matrix 256×512, 30 sections 7 mm thick, gap 1 mm, scan duration 3 min 30 s) were performed. The patient was then repositioned with the lumbar spine in the magnet's isocenter, shifting the patient caudally approximately 20 cm. A second localizer was acquired [fast-field echo (FFE); TR/TE/flip angle=21 ms/3.4 ms/45°), three sections in three orientations each, 10 mm thick, scan duration 24 s). Based on this scan, a sagittal T1-weighted scan was started (TSE; TR/TE/flip angle=3500 ms/120 ms/90°, FOV 460 mm, acquired matrix 288×384, 13 sections 4 mm thick, gap 0.5 mm, ETL=17, one 80-mm-thick coronal saturation slab, scan duration 3 min 54 s). In all sequences the built-in bird-cage body coil was used for transmission. The maximum B1 field for excitation and refocusing pulses was 27.5 µT. The specific absorption rates (SAR) of the five scans as indicated by the sequence monitor were 0.3, 2.8, 2.4, 0.5 and 3.0 W/kg body weight. For acquisition of the resonance signals the body coil was used in the first three scans, and the synergy spine coil for the last two scans.
An anaesthesiologist was present in the examination room during the scans, to supervise the patient who required intensive care.
The MR scans were performed as described following the normal procedure. During the last scan the patient suddenly cried for help, and the anaesthesiologist noticed a flame of approximately 3 cm arising from the shirt at the right upper chest, close to the position of the ECG electrodes. From the head opening the anaesthesiologist bent towards the patient into the magnet bore and extinguished the flames with his hands. The scan was immediately discontinued and the patient pulled out of the magnet bore.
The subsequent physical examination of the patient revealed second- to third-degree burns at the position of the ECG electrodes. In addition, it was noticed that the patient was perspiring, and thus had a galvanic contact to the supporting cushion.
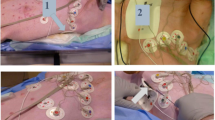
Particles of molten plastic were found on the blanket and on the shirt of the patient. Over the right upper thorax a large hole was burned into the shirt (Fig. 1).
At the position of the electrodes there was scab on the skin; slightly above was an extended erythroderma. The patient complained about severe pain. The wound was immediately covered with a sterile bandage.
A closer inspection of the ECG leads revealed that the plastic clips at the connection of the ECG lead and the electrodes were deformed and partially molten, especially the uppermost positioned electrode, depicted on the left in Fig. 2. The plastic foils of the electrodes were stained with soot; however, they were not molten or perforated and remained intact (Fig. 3). Skin burns were found at the position of the electrodes (Fig. 4).
The ECG monitor was intact and showed no indication of being affected by high voltage or current.
In the course of the following weeks, the patient recovered well from his underlying condition and this incident and could be discharged after 8 weeks.
Discussion
While the exact sequence of events leading to the fire in this specific case is not fully understood, the analysis shows that a number of conditions may have led to the hazardous behaviour. We assume that coupling took place not with alternating B1, the magnetic component of the exciting electromagnetic field in the transmitting body coil, but with E1, its electric component. Induction in the ECG cabling caused by E1 led to a high-voltage built up at the position of the electrodes. Due to galvanic or capacitive coupling, current could flow through the patient. The energy was dissipated to heat mostly at the position of the highest impedance, which was either at the contact of electrodes to skin or at the contact of the lead to the electrodes, i.e. at the contact clips. It is known that energy dissipation may lead to burns if current through a closed current loop is led through a high impedance, e.g. formed by a skin–skin contact [12]. The galvanic resistance between electrode and skin can be 500–6000 ohms, depending on skin preparation [13]. The observed burns at the electrode–skin contact may be due to energy dissipation at this position; however, the fact that the electrodes were unaltered, while the plastic clips were partially molten, hints to larger energy dissipation at the lead–electrode contact. The galvanic resistance of the uninterrupted contact of clip and electrode was between 5 and 500 ohms and depended on motion. When the leads are correctly connected to the monitor, heat dissipation is low. An improper grounding or connection to the monitor causes heat dissipation at the electrode, so that temperature increases with time. It may affect the skin, but the temperature remains probably too low to inflame cloth; however, preliminary experiments have shown that voltages induced into the ECG cabling by the applied TSE sequences are sufficiently high to induce sparking between the contact clip and an appropriate counterpart, e.g. the graphite mine of a pencil. Especially if the conducting edge of the clip has loose contact with the electrode, i.e. the clip is not firmly fixed so that the galvanic contact is frequently interrupted due to patient movement, sparks between clip and electrode emerge. Sparking is significant with an open-ended cable that is not grounded, but sparks could also be detected with a cable properly connected to the monitor. The findings described in this report indicate a significant heating at the contact of lead and electrode, presumably caused by a loose contact with induction of sparks. The heat released by the sparks deformed the clips, and the sparks inflamed the surrounding cloth.
The fact that heat dissipation and/or sparking took place at the patient's side of the conductor, while the monitor was not affected by high voltage, is in accordance with similar findings in phantom experiments with guide wires [7].
We assume that the burn at the position of a pulse oximetry sensor reported earlier [1] has been caused by a similar chain of events as in the present case. Probably the sensor cable was made of a conducting material, and high voltage had built up at the finger sensor, induced by the electric component of the radio-frequency field, in contrast to the explanation proposed in the report, that a high current had been induced by the magnetic field in a suspected loop.
This case shows that the danger of inducing high voltages in long conductors, such as leads, guides or sensors, is often underestimated. While in the majority of examinations no heating is observed, there are specific conditions in which induction may occur resulting in significant heat production. The exact conditions for this are difficult to predict, as they depend on the field distribution in the exciting coil, the impedance of the conductor that acts as an antenna, the coupling of the antenna to the field and the actual wavelength of the alternating current at the larmor frequency, which again depends on the dielectricity of the surrounding media. Extreme values may be reached if the conductor acts as a Hertz dipole in resonance with the exciting HF field. In preliminary experiments after the incident, heating and sparking were observed even with a setup not specifically tuned to resonance. As it is difficult to predict resonance conditions when a person is in the bore, we cannot exclude that even stronger effects occurred with the patient in position. The relative dielectricity ranges from approximately 1 for air surrounding a conductor to 80 if a conductor is immersed in water. The wavelength at 1.5 T may thus lie between 4.7 and 0.5 m, depending on whether the path of the conductor is surrounded by air or tissue. Depending on the termination of the conductor, a standing wave may be formed in a straight conductor of half a wavelength.
Further parameters are the spatial extension of the exciting field (more induction occurs in a body coil than in a smaller coil), the E1 strength (it depends on B1, the construction of the transmitting coil, and the presence of other capacities within the magnet bore, e.g. receive coils) and the duty cycle (induction is highest with 180° pulses, i.e. with TSE sequences).
The risk of high-voltage induction can be reduced with small excitation fields (head coil or surface coils for excitation), small pulse angles (gradient-echo sequences with low pulse angles), short conductors (shorter than 1/2 wavelength in the surrounding medium, i.e. shorter than 2.35 m in the air, and shorter than 25 cm for conductors in the body, assuming similar dielectricity of body tissue and water), high impedance of conductor, positioning with maximum distance from coil leads (exciting and receiving coils). In contrast to the external ECG unit used in the case described here, the built-in trigger unit of the scanner seems to be safe. Its lead is shorter and has a higher resistance of 60 k ohms. No sparking could be induced under identical conditions using the built-in unit with this lead.
The incident demonstrates that the use of ECG cables and similar long conductors as stimulation electrodes or guide wires imply hazards, the conditions of which are not fully known; therefore, when using long conductors special care must been taken even with procedures that seem to be safe and worked without problems on a routine base: already slight changes in the setup may lead to dangerous situations. Further investigation is required to be able to define specific limits of all relevant parameters, which must be observed for safe MR examinations with implanted or extracorporeal long conductors.
References
Shellock FG, Slimp GL (1989) Severe burn of the finger caused by using a pulse oximeter during MR imaging (Letter). AJR 153:1105
Kanal E, Shellock FG (1990) Burns associated with clinical MR examinations (Letter). Radiology 175:585
Kanal E, Shellock FG, Talagala L (1990) Safety considerations in MR imaging. Radiology 176:593–606
Kanal E, Shellock FG (1992) Patient monitoring during clinical MR imaging. Radiology 185:623–629
Maier SE, Wildermuth S, Darrow RD, Watkins RD, Debatin JF, Dumoulin CL (1995) Safety of MR tracking catheters (Abstract). Proc Soc Magn Reson 3:497
Ladd ME, Quick HH, Boesiger P, McKinnon GC (1998) RF heating of actively visualized catheters and guidewires (Abstract). Proc Intl Soc Mag Reson Med 8:473
Nitz WR, Oppelt A, Renz W, Manke C, Lenhart M, Link J (2001) On the heating of linear conductive structures as guide wires and catheters in interventional MRI. J Magn Reson Imaging 13:105–114
Hofman MBM, de Cock CC, van der Linden JC et al. (1996) Transesophageal cardiac pacing during magnetic resonance imaging: feasibility and safety considerations. Magn Reson Med 35:413–422
Achenbach S, Moshage W, Diem B, Bieberle T, Schibgilla V, Bachmann K (1997) Effects of magnetic resonance imaging on cardiac pacemakers and electrodes. Am Heart J 134:467–473
Rezai AR, Finelli D, Nyenhuis JA et al. (2002) Neurostimulation systems for deep brain stimulation: in vitro evaluation of magnetic resonance imaging-related heating at 1.5 Tesla. J Magn Reson Imaging 15:241–250
Girnus R, Hesselmann V, Luyken K, Krug B, Nimtz G, Lackner K (2002) Interventional MRI in patients with implanted deep brain stimulation electrodes: safety aspects (Abstract). Proc Intl Soc Magn Reson Med 10:2242
Knopp MV, Essig M, Debus J, Zabel HJ, Kaick G von (1996) Unusual burns of the lower extremities caused by a closed conducting loop in a patient at MR imaging. Radiology 200:572–575
Patterson RP (1978) The electrical characteristics of some commercial ECG electrodes. J Electrocardiol 11:23–26
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kugel, H., Bremer, C., Püschel, M. et al. Hazardous situation in the MR bore: induction in ECG leads causes fire. Eur Radiol 13, 690–694 (2003). https://doi.org/10.1007/s00330-003-1841-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-003-1841-8