Abstract.
The aim of this article is to report on three patients with injuries of the peroneal nerve along the posterolateral aspect of the knee. Injuries in this area are less common than the injuries occurring at the level of the fibular head. In this article we report on three patients with posterolateral knee trauma who had peroneal nerve dysfunction. To better understand the precise location of the nerve on MR images, we performed MR imaging in five volunteers, and studied the position of the nerve on anatomic dissection (n=1) and anatomic slices (n=1). The common peroneal nerve is easily depicted on MR images and has a typical location along the posterior margin of the biceps tendon. Non-visualisation of the peroneal nerve at the posterolateral aspect of the knee, as seen on MR images, is consistent with nerve injury. Scar tissue at the posterolateral aspect of the knee indicates injury of this specific area, and involvement of the peroneal nerve is likely.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Many injuries of the peroneal nerve are related either to trauma or compression [1, 2, 3]. At the level of the fibular head the superficial position of the nerve renders it vulnerable to compression by osteophytes, bony deformity following trauma and tumours. Less typically, the nerve may also be injured in association with trauma to the posterolateral corner of the knee. In such cases the lesion is located in a more superior position relative to the position of the fibular head. Whereas electromyography is essential for functional assessment of the nerve, MR imaging may directly visualize the common peroneal nerve and adjacent structures.
In this article we present three patients with abnormalities of the peroneal nerve after knee trauma studied by MR imaging. Two anatomic specimens were evaluated to demonstrate the relationship of the peroneal nerve to the adjacent structures of the posterolateral aspect of the knee.
Materials and methods
The clinical and imaging files of three patients with a peroneal nerve palsy following knee trauma were reviewed. The three cases were retrospectively retrieved from our musculoskeletal teaching files. The MR imaging was performed employing T1-, proton-density- and T2-weighted MR images on a 1- or 1.5-T clinical system (Siemens, Erlangen, Germany). The clinical charts were reviewed by the principal investigator, whereas the imaging files were reviewed by consensus of two fellowship trained musculoskeletal radiologists. Observations made during surgery were recorded, as well as follow-up data.
Two anatomic specimens from elderly subjects were obtained from the Department of Anatomy. A fresh cadaveric knee specimen (n=1) was dissected along the posterolateral aspect of the knee and the common peroneal nerve was exposed. The anatomic relationships of the peroneal nerve relative to adjacent structures were evaluated.
The posterolateral aspect of the knee was also studied on a transverse anatomic section (n=1) of the knee obtained from the Department of Anatomy. Proton-density-weighted MR images were obtained in five volunteers in the sagittal and transverse plane on a 1.5-T clinical system (Vision, Siemens, Erlangen, Germany). The MR imaging parameters were as follows: TR 2900 ms/TE 15 ms; two signals averaged; section thickness 3 mm; matrix size 252×512; field of view 150×240 mm. The anatomic criteria evaluated included the position of the nerve relative to adjacent ligaments and tendons, size and signal intensity on MR images.
Results
Anatomic and imaging findings
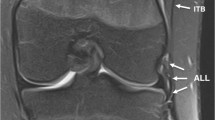
During anatomic dissection the peroneal nerve was demonstrated upon sectioning the superficial fascia. The nerve was located in close proximity to the posterior margin of the tendon of the biceps femoris muscle (Fig. 1). On MR images of volunteers the common peroneal nerve was seen as a few hypointense nerve bundles embedded in fatty tissue (Fig. 2). The nerve could be depicted in all imaging planes. On transverse anatomic sections the posterior location of the common peroneal nerve relative to the biceps tendon and muscle was demonstrated (Figs. 3, 4).
Case reports
Case 1
An 18-year-old man developed a right-sided dropfoot related to knee injury during a motorcycle trauma. Results of electromyography indicated a complete transsection of the peroneal nerve. The MR imaging performed 1 month after injury demonstrated severe injury to the posterolateral corner of the knee including avulsion of the biceps tendon from the fibular head, as well as a tear of the lateral collateral ligament. Posteriorly to the biceps tendon, an area of poorly defined intermediate signal intensity was depicted (Fig. 5). The peroneal nerve, which is normally easily demonstrated in this region, could not be visualized. At surgery a complete transsection of the peroneal nerve was demonstrated. Remnants of the peroneal nerve and the torn biceps tendon were embedded in a fibrous mass of scar tissue. The proximal portion of the peroneal nerve showed severe atrophy rendering nerve reconstruction impossible.
a Transverse proton-density-weighted MR image(TR 4700 ms/TE 19 ms) of injured knee. A poorly defined area of intermediate signal intensity is seen at the normal position of the biceps tendon and peroneal nerve (asterisk). b Transverse proton-density-weighted MR image in unaffected knee of same patient. In comparison, the biceps tendon (asterisk) and peroneal nerve (arrow) can be clearly depicted on the unaffected side
Case 2
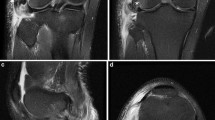
A 34-year-old man developed a right-sided dropfoot following knee trauma during a motorcycle accident. Results of electromyography indicated paralysis of the peroneal nerve at the level of the fibular head. The MR imaging was performed 3 weeks after injury and demonstrated several knee injuries including a tear of the anterior cruciate ligament, lateral collateral ligament, popliteus tendon, and biceps tendon. A poorly defined area of low to intermediate signal intensity was seen along the posterolateral aspect of the knee. The peroneal nerve and biceps tendon could not be recognized at their expected position. In addition, swelling and hyperintense signal changes of the anterolateral muscle compartment of the lower leg, characteristic of peroneal nerve denervation, was demonstrated. At surgery a tear of the peroneal nerve and a posttraumatic neuroma were demonstrated (Fig. 6). The neuroma was resected and an end-to-end anastomosis of the nerve was performed. The ligaments and tendons of the posterolateral corner were reconstructed. One year after surgery, there was still no evidence of recovery of nerve function.
A 34-year-old man with knee trauma. a Coronal T2-weighted MR image (TR 3700 ms/TE 93 ms). Hypointense scar (s) tissue with irregular outline is seen at the level of the distal aspect of the biceps tendon (B). b Transverse proton-density-weighted MR image (TR 4700 ms/TE 19 ms). Poorly defined hypointense strands are seen in the normal location of the fibular collateral ligament, biceps tendon and peroneal nerve (arrowheads). c Transverse proton-density-weighted MR image (TR 4700 ms/TE 19 ms) through the superior third of the lower leg. Hyperintense signal changes are seen in the anterolateral muscle compartment indicative of denervation (AL)
Case 3
A 32-year-old man was referred to the Department of Neurosurgery for evaluation of a dropfoot. During a motor vehicle accident he experienced a penetrating injury of the posterolateral aspect of his right knee involving a large fragment of glass. The fragment was surgically removed and an attempt was made to reconstruct the sectioned nerve. He presented for reevaluation 6 years after this initial injury. At present, evaluation by MR imaging demonstrated an oval-shaped mass measuring 1.5×2x1.5 cm and located 4 cm above the level of the fibular head. The proximal portion of the peroneal nerve terminated in this mass. More distally the peroneal nerve was not seen and was replaced by fibrous strands of low to intermediate signal intensity over a distance of 5 cm (Fig. 6).
Given the longstanding presence of injury and the large gap, no new attempt at nerve reconstruction was made.
Discussion
The common peroneal nerve is the smaller of the two terminal divisions of the sciatic nerve. It usually arises along the middle third of the thigh, and runs inferiorly and laterally along the medial margin of the biceps muscle. Then it crosses the plantaris muscle and the lateral head of the gastrocnemius muscle and passes posterolaterally to the head of the fibula. At the level of the fibular head the peroneal nerve then turns anteriorly around the fibular head. In this site the nerve is particularly susceptible to injury. The nerve then continues between the lateral side of the neck of the fibula and the peroneus longus muscle. Here the peroneal nerve divides into two branches: the superficial peroneal nerve and the deep peroneal nerve [1, 2, 3, 4]. The superficial peroneal nerve passes deep between the peroneus longus muscle and the fibula. It gradually becomes more superficial and descends the leg between the peroneus longus and brevis muscles. Finally, the superficial peroneal nerve pierces the crural fascia to end as the medial and intermediate dorsal cutaneous nerves [4, 5, 6]. There are considerable variations in the course of the deep peroneal nerve, which may be located anteriorly, anteromedially or anterolaterally relative to the anterior tibial vessels.
At the level of the knee joint the location of the peroneal nerve may be described with reference to the capsuloligamentous planes. Along the posterolateral aspect of the knee the most superficial capsuloligamentous plane corresponds to the crural fascia. When the fascia is dissected posteriorly to the biceps tendon the common peroneal nerve is exposed, as shown by our anatomic work. In this region the common peroneal nerve may be easily identified using MR imaging due to its location adjacent to the posterior margin of the biceps tendon.
These topographic details are easily visualized on MR images on which the nerve is seen to consist of a few thin nerve bundles interspersed among fatty tissue. Whereas the nerve bundles exhibit a hypointense appearance, the fatty tissue exhibits a hyperintense appearance both on T1- and T2-weighted MR images. The position of the peroneal nerve posterior to the biceps tendon and deep to the fascia represents a useful landmark for correct identification of the nerve. Although neurological investigations may confirm denervation of the peroneal nerve, the precise site of injury is more easily identified on MR images. In addition, MR imaging can provide information about the distance between the nerve ends, presence of scar tissue or posttraumatic neuroma (Fig. 7).
a Coronal and b transverse proton-density-weighted MR image (TR 2900 ms/TE 15 ms). The peroneal nerve (short arrowheads) ends in an oval-shaped mass, presumed to represent a neuroma. More distally, hypointense strands are depicted and the peroneal nerve cannot be seen (arrowheads). b The neuroma (arrowheads) is seen posterior to the biceps tendon (curved arrow) and muscle (b) in the normal position of the common peroneal nerve and deep to the superficial fascia (thick arrow)
Various conditions may cause peroneal nerve palsy including trauma [2, 3, 4, 5, 6, 7, 8], repetitive mechanical irritation [2], iatrogenic injury [9], leprosy, hereditary neuropathy, and compression by soft tissue and osseous pathologies [1, 3, 10].
In the setting of knee trauma the proximity of the peroneal nerve to the posterolateral tendons and ligaments renders it vulnerable to injury in association with tears of these former structures. Whereas lesions of the lateral supporting structures of the knee are less frequent than lesions of the medial supporting structures, lateral injuries generally produce more significant functional impairment. In patients with severe injury to the lateral corner, the peroneal nerve may be involved leading to a characteristic dropfoot deformity, as shown in the patients presented. Sensory loss may extend over the anterolateral aspect of the leg and dorsum of the foot [11]. Electromyography may be useful to differentiate between a radicular lesion at the L5 level and a peripheral lesion of the peroneal nerve [1].
Magnetic resonance imaging demonstrates very clearly the peroneal nerve at the posterolateral aspect of the knee. With posterolateral knee injuries tears of the different ligaments and tendons may be demonstrated. With nerve injuries the peroneal nerve, which is normally clearly visualized, is not depicted and a poorly defined area of signal intensity may be evident in the normal position of the nerve. In addition, MR imaging may demonstrate fatty infiltration, atrophy or hypertrophy in the muscle compartments innervated by the involved nerve.
A few limitations of our report should be taken into account. Firstly, the number of cases presented is limited. Because the cases were selected retrospectively, slightly different imaging parameters were employed in the patients studied. Nevertheless, all studies were conducted on clinical systems with commonly used sequences. Short tau inversion recovery (STIR) sequences, however, were not performed. Surgical correlation was not available for the third patient, but we attempted to reduce interpretation bias by meticulous correlation with anatomic findings and analysis by consensus of two readers. Finally, only two anatomic specimens were assessed which does not take into account normal anatomic variation [12].
Conclusion
In conclusion, in patients with severe trauma to the posterolateral aspect of the knee, the peroneal nerve may be involved. The MR imaging excellently demonstrates injuries of ligaments and tendons in this region. The peroneal nerve shows a characteristic location posterior to the biceps tendon and deep to the fascia. When the peroneal nerve is not depicted in this area, or is replaced by poorly defined signal intensity, peroneal nerve rupture is likely.
References
Rondepierre P, Martini L, Wannin G, Floquet J (1990) Kyste intraneural: une cause rare de paralysie du nerf sciatique poplité externe. Rev Neurol 146:375–376
Watemberg N, Amsel S, Sadeh M, Lerman-Sagie T (2000) Common peroneal neuropathy due to surfing. J Child Neurol 16:420–421
Gallagher-Oxner K, Bagley L, Dalinka MK, Kneeland JB (1994) Case report 822. Skeletal Radiol 23:71–72
Romanes GJ (1966) Cunningham's manual of practical anatomy, Oxford University Press, London
Adkison D, Bosse M et al. (1991) Anatomical variations in the course of the superficial peroneal nerve. J Bone Joint Surg 73 A:112–114
Lawrence S, Botte M (1995) The deep peroneal nerve in foot and ankle: an anatomic study. Foot Ankle Int 16:724–728
Neundörfer, Seiberth R (1975) The accessory deep peroneal nerve. J Neurol 209:125–129
Tomaino M, Day C, Papegeorgiou C, Harner C, Fu FH (2000) Peroneal nerve palsy following knee dislocation: pathoanatomy and implications for treatment. Knee Surg Sports Traumatol Arthrosc 8:163–165
Esselman P, Tomski MA, Robinson LR, Zisfein J, Marks SJ (1993) Selective deep peroneal nerve injury associated with arthroscopic knee surgery. Muscle Nerve 16:1188–1192
Yamazaki H, Satoru S, Seki H, Narimichi M, Tomoko M, Kunio T (1999) Peroneal nerve palsy caused by intraneural ganglion. Skeletal Radiol 28:52–56
Mont M, Dellon L, Chen F, Hungerford MW, Krackow KA, Hungerford DS (1996) The operative treatment of peroneal nerve palsy. J Bone Joint Surg 78A:863–869
Loredo R, Hodler J, Pedowitz R, Yeh LR, Resnick D (1988) MRI of the common peroneal nerve: normal anatomy and evaluation of masses associated with nerve entrapment. J Comput Assist Tomogr 22:925–931
Acknowledgement. We thank F. van Roy and E. Barbaix for help with anatomic dissections, and F. De Ridder and E Gilissen for help with MR imaging studies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Trappeniers, L., De Maeseneer, M., Van Roy, P. et al. Peroneal nerve injury in three patients with knee trauma: MR imaging and correlation with anatomic findings in volunteers and anatomic specimens. Eur Radiol 13, 1722–1727 (2003). https://doi.org/10.1007/s00330-003-1833-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-003-1833-8