Abstract
The purpose of this article is to describe the association between spontaneous osteonecrosis and insufficiency stress fractures of the knee. To determine whether insufficiency stress fracture is associated with spontaneous osteonecrosis of the knee, we retrospectively reviewed the medical charts and imaging studies of all patients with spontaneous osteonecrosis of the knee, studied by MR imaging, seen in a tertiary hospital over an 8-year period. Four women (age range 66–84 years) presented spontaneous osteonecrosis of the knee associated with insufficiency stress fracture of the medial tibial plateau. One of these patients also presented a concomitant insufficiency stress fracture of the medial femoral condyle. Radiographs were diagnostic of spontaneous osteonecrosis of the medial femoral condyle in three cases, and insufficiency stress fracture of the medial tibial plateau was detected in one case. Magnetic resonance imaging allows the diagnosis of both conditions in all four cases. Spontaneous osteonecrosis of the knee may be associated with insufficiency stress fracture of the medial femoral condyle and the medial tibial plateau. This association provides additional arguments in favor of the traumatic etiology of spontaneous osteonecrosis of knee.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spontaneous osteonecrosis of the knee (SONK) is a well-described cause of acute knee pain. It occurs in older individuals, usually after the sixth decade of life [1, 2]. Women are affected three times more frequently than men [2, 3]. Pain is usually characterized by sudden onset (frequently the patient can remember the exact moment or the activity during which the symptom started) [1] and is initially severe, causing significant functional impairment; pain is frequently present at rest. There is typically no history of an acute injury. The condition is usually unilateral with lesions generally restricted to one femoral condyle or tibial plateau [1]. The medial side of the joint is the side most commonly involved, and lesions occur more often in the femoral condyle than in the tibial plateau [1, 2]. The precise pathogenesis of SONK remains unclear, and whether the disease process develops from minor unrecognized traumatic insults with associated microfractures or from primary vascular insufficiency remains a subject of debate [3].
We report four cases with SONK associated with insufficiency stress fracture of the medial tibial plateau, one of them also presenting insufficiency stress fracture of the medial femoral condyle. This association argues for a traumatic etiology of SONK.
Materials and methods
A computer registry was used to provide the names of all patients diagnosed by MR imaging of spontaneous osteonecrosis of the knee (SONK) at our institution, a teaching tertiary hospital, from may 1993 to may 2001. Cases studied were restricted to patients in whom medical charts and MR images were available for review. Patients with a history of major trauma, meniscectomy, or predisposing factors of osteonecrosis were excluded from the study.
These restrictions identified 62 cases, one of them with bilateral involvement. They were 45 women and 17 men, with a mean age of 68±8 years.
Medical charts, radiographs when available, and MR images of these patients were retrospectively reviewed looking for the association between SONK and insufficiency stress fracture. We found four cases in which SONK was associated with insufficiency fractures of the medial tibial condyle and/or tibial plateau. These four patients formed our study group.
The radiographic criteria of SONK on radiographs were based on those previously described [1, 2, 3]: slight flattening of the medial condyle, followed by the appearance of a linear or cystlike subchondral radiolucent lesion, and finally, articular collapse.
The MR images were obtained on a 1.5-T Gyroscan ACS NT, or on a 0.5-T Gyroscan II (both from Philips, Best, The Netherlands). Sagittal T1-weighted spin-echo (TR 540–600 ms/TE 15–20 ms) and coronal and axial T2*-weighted gradient-echo (TR 500–906 ms/TE 14–28 ms/30–35 ms) images were obtained in all cases.
Sagittal double-echo, T2-weighted spin-echo (TR 2000–2200 ms/TE 20 ms/80 ms), or sagittal T2* gradient-echo (TR 906 ms/TE 28 ms/35 ms) images, were also acquired in all cases.
Additional sequences included sagittal short tau inversion recovery (STIR; TR 1561 ms/TE 15 ms/160 ms) and coronal T1-weighted spin-echo (TR 631 ms/TE 20 ms) images, and coronal proton-density fat-suppressed images (TE 1756 ms/13 ms).
The MR imaging criteria that were used for the diagnosis of SONK were previously reported [4, 5]: a discrete area of low signal intensity on both T1- and T2-weighted images in the subchondral region of the affected femoral condyle or tibial plateau, surrounded by bone marrow edema changes. In cases of SONK with normal radiographs, we applied MR imaging criteria of irreversible SONK of Lecouvet et al. [6, 7] excluding those with characteristics of transient epiphyseal lesions.
The MR imaging criteria for the diagnosis of stress fractures were based on those described in previous studies [8, 9]: (a) bandlike areas of very low signal intensity in the medullary space, which usually extend to the cortex; and (b) surrounding alteration in signal intensity in the marrow space with ill-defined low signal intensity on T1-weighted images and high signal intensity on T2-weighted images, which represents medullary edema and hemorrhage.
Results
The clinical history and summary of the imaging studies of the four patients are shown in Table 1. They were four elderly women who presented with severe acute knee pain. Pain appeared suddenly in all cases. It was severe and localized in the medial aspect of the knee, causing significant functional impairment in all cases. Pain at rest was present in three of the four patients. Physical examination showed tenderness over the involved area, with small or moderate effusion in all cases. The synovial fluid was examined in two patients being non-inflammatory.
The SONK was diagnosed on radiographs in three patients (cases 1, 3, and 4), showing a slight flattening and increased density of the weight-bearing aspect of the medial femoral condyle (Fig. 1a).
An 85-year-old woman with a 3-week history of spontaneous left knee pain. a Initial radiograph shows slight flattening and sclerosis of the medial femoral condyle. Sagittal b T1-weighted and c T2-weighted MR images through medial compartment obtained weeks after a show a subchondral area of low signal intensity in the weight-bearing area of femoral condyle, and an irregular horizontal band of low signal intensity in the medullary cavity of tibial plateau. Ill-defined bone marrow low signal intensity on T1-weighted images and high signal intensity on T2-weighted images adjacent to both lesions are also noted
Insufficiency stress fracture was radiographically diagnosed in one case (case 2; Fig. 2a). In cases 2 and 4 follow-up radiographs were available. In case 2, follow-up radiographs disclosed a faint sclerotic band in the subchondral region of the medial tibial plateau (Fig. 2f). In case 4, the necrotic lesion of the medial femoral condyle evolved to articular collapse, but the insufficiency stress fracture was not identified on follow-up radiographs.
A 66-year-old woman with a 6-week history of spontaneous left knee pain. a Initial radiograph demonstrates a focal linear area of sclerosis in the cancellous bone of the medial tibial plateau (arrowheads), corresponding to an insufficiency stress fracture. The patient was treated conservatively with rest and anti-inflammatory drugs without improvement. For this reason an MR examination was performed. b,c Coronal T1-weighted MR images through medial compartment obtained 8 weeks after a. In the more anterior section ( b), a thin line of low signal intensity (arrows) is seen within the cancellous bone of tibial plateau. A slightly more posterior section ( c) demonstrates ill-defined region of decreased signal intensity in femoral condyle (arrowheads) with better-delineated subchondral low signal intensity area (white arrows). Ill-defined low signal areas are seen in the subarticular of the medial tibial plateau, between the fracture line and the subchondral bone plate. d, e Sagittal T2-weighted MR images through medial compartment shows that the subchondral lesion of femoral condyle has low signal intensity, whereas surrounding bone marrow has high signal intensity. The lineal area of low signal intensity (arrowheads) is less conspicuous. Note tear of the posterior horn of the medial meniscus. f Radiograph obtained 1 week after that in b–e. The fracture line of medial tibial plateau is seen as a faint linear sclerotic area (arrow)
The MR images were obtained 4, 14, 20, and 22 weeks after the onset of pain, and allowed a diagnosis of both conditions (Figs. 1b, c, 2b–e, 3a, b). The interval between initial radiographs and MR examination was 1, 6, 6, and 8 weeks retrospectively.
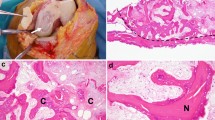
A 74-year-old woman with an 8-week history of spontaneous right knee pain. a, b Sagittal T1-weighted MR images through medial compartment reveal an irregular horizontal band of low signal intensity at femoral condyle (arrows), and several curvilinear low-signal intensity zones at tibial plateau (arrowheads), surrounded by more diffuse areas of bone marrow increased signal intensity suggestive of edema. A low-signal intensity subchondral area is seen at weight-bearing aspect of femoral condyle. c, d Coronal fat-suppressed proton-density-weighted MR images through medial compartment show linear low signal intensity areas at femoral condyle (arrows) and tibial plateau (arrowheads) with diffuse increased signal intensity of surrounding bone marrow. Note femoral subchondral area of low signal intensity with increased signal intensity of surrounding bone marrow, and focal epiphyseal contour depression (long arrow)
The SONK and insufficiency fractures was surrounded by intensity changes of bone marrow edema in all cases, but in case 2 the insufficiency stress fracture was associated with minimal bone marrow signal intensity changes (Fig. 2b–e), probably due to the long interval between the onset of pain and MR examination (14 weeks).
Interestingly, one patient presented insufficiency stress fractures of both the medial tibial plateau and medial femoral condyle (Fig. 3a, b).
Discussion
Spontaneous osteonecrosis of the knee is a well-recognized cause of acute knee pain in the elderly population. The precise pathogenesis of this condition remains unclear, although two main theories have been proposed: primary vascular insufficiency leading to bone infarction; or a minor, unrecognized traumatic insult producing microfractures in the subchondral bone and subsequent osteonecrosis [2, 3].
The usual sudden onset of symptoms that characterizes SONK, its occurrence in elderly patients, in whom osteoporosis is frequent, and its characteristic predilection for the area of maximum weight-bearing of the medial femoral condyle or tibial plateau, strongly suggest a traumatic lesion as the most likely underlying cause of SONK [1, 4].
Of interest, several reports supporting this hypothesis have been recently presented. In this sense we found significant differences between idiopathic and secondary osteonecrosis of the knee, especially with regard to clinical presentation and location, extent, and MR imaging appearance of the lesions [10]. Contrary to what has been described in idiopathic forms, secondary osteonecrosis generally occurs in younger patients and frequently has an insidious onset with mild or vague pain, the lateral compartment of the knee is often involved, and lesions are generally larger than lesions arising spontaneously. In the great majority of cases they involved femoral condyles and/or tibial plateaus [10]. Bilateral distribution and multifocal involvement is also seen in these forms. It is remarkable that in this series the demarcation rim, which is considered specific and pathognomonic of avascular osteonecrosis, was observed in most of the patients with secondary osteonecrosis, but in none of those with spontaneous osteonecrosis [10]. We, according to other authors [5, 11, 12], hypothesize that these differences are probably due to a difference in the pathogenic mechanism.
The fact that patients with secondary osteonecrosis have more extensive lesions that generally occur in the lateral compartment, and that other joints may be affected, argues for a generalized "metabolic" etiology as opposed to a more local "mechanical" cause in the SONK.
According to our results, a recent histopathological study of a series of 14 cases of SONK surgically treated also suggested that the primary event leading to SONK is a subchondral insufficiency fracture, and that the localized osteonecrosis seen in association with this disease is the result of a fracture [5]. These authors report histological differences between the classic wedge-shaped infarct of secondary osteonecrosis, and necrotic lesions of SONK, which are situated between a linear fracture close to the articular surface and the articular surface [5].
These same authors have been reported another case presenting insufficiency stress fracture of both the medial femoral condyle and the femoral head, which radiographically resembled osteonecrosis [11]. These authors reviewed the histopathological differences between insufficiency stress fracture and SONK, and concluded that SONK is the result of subchondral insufficiency stress fracture of the medial femoral condyle [11].
Stress fractures of the knee in older patients are considered as insufficiency type fractures caused by normal stress applied to insufficient bone, oftenly osteoporotic.
In most patients no increase of physical activity is referred as an identifiable precipitating factor [12, 13]. Typically, these fractures involve the medial tibial plateau [13]. Medial femoral condyle or lateral tibial plateau are rarely recognized as site of involvement [12, 13]. Despite SONK, pain at rest and at night is uncommon in stress fractures [12, 13]; however, these two entities frequently cannot be differentiated from each other based only on clinical, plain radiography, and bone scan findings [14, 15]. The MR imaging is usually adequate to discriminate between osteonecrosis and stress fractures [16].
To our knowledge, only three cases of SONK associated with stress fracture of the tibial plateau [14, 15] have been previously reported. LeGars et al. described a series of 13 cases with stress fracture of the medial tibial plateau, and one of them, an 85-year-old woman with previous history of long-term glucocorticoid intake, presented concomitant SONK [14].
Recently, Sokoloff et al. reported two cases in whom SONK was associated with stress fracture of the medial tibial plateau [15]. All these three cases were elderly women (mean age 71 years) presenting knee pain, and two of them presented joint osteoarthritic changes [14, 15]. Tear of the medial meniscus was reported in the two cases of the Solokoff series [15]. In the series reported by Le Gars et al., the great majority of cases showed MR signs of medial meniscus rupture, although there is no specific mention of the presence of medial meniscal tear in the aforementioned patient [14].
Herein we report four more cases of SONK associated with stress fracture. One of our patients (case 3) developed SONK with concomitant stress fractures of both the medial tibial plateau and femoral condyle. To our knowledge, neither the association of SONK with stress fracture of the medial femoral condyle nor the occurrence of simultaneous stress fracture of the medial femoral condyle and medial tibial plateau have been reported previously.
In our series, less than 5% of patients with SONK present a insufficiency stress fracture of the knee. Due to the strict inclusion criteria used in our study (only patients studied by MR imaging, in whom signs of irreversible lesions were identified), our group of patients is probably not representative of the entire population affected with SONK.
The SONK and stress fracture are not uncommon conditions, and therefore the combination in these patients could have happened by chance; however, in our opinion, according to Solokoff et al. [15], this association reinforces the theory of a traumatic etiology of SONK.
Our patients were elderly women, without predisposing factors for osteonecrosis. All four patients presented knee osteoarthritic changes, showed medial meniscus tear on MR imaging, and three of them were osteopenic. Several authors have suggested that the presence of medial meniscus tears, osteoarthritis, and/or osteoporosis may be a significant contributing factor in the development of subchondral plate microfractures [4, 10, 15, 17].
The diminished load-bearing capacity of injured meniscus increases the applied forces to the subchondral plate [14, 17]. In the same way, osteoporosis and cartilage thinning seen on osteoarthritis can weaken the load-bearing capacity of subchondral bone, such that stress fracture can result from normal activity [4, 9].
In summary, our cases lend further credence to the postulate that SONK has a traumatic etiology.
References
Houpt JB, Pritzker KPH, Alpert B, Greyson ND, Gross AE (1983) Natural history of spontaneous osteonecrosis of the knee (SONK): a review. Semin Arthritis Rheum 13:212–227
Aglietti P, Insall J, Bohne WH (1983) Idiopathic osteonecrosis of the knee: aetiology, prognosis and treatment. J Bone Joint Surg (Br) 65:588–597
Pattel DV, Breazale NM, Behr CT, Warren RF, Wickiewitz TL, O'Brien SJ (1998). Osteonecrosis of the knee: current clinical concepts. Knee Surg Sports Traumatol Arthrosc 6:2–11
Blum GM, Tirman PFJ, Crues JV III (1993) Osseous and cartilaginous trauma. In: Mink JH, Reicher MA, Crues JV III, Deutsch AL (eds) MRI of the knee, 2nd edn. Raven, New York, pp 295–332
Yamamoto T, Bullough PG (2000) Spontaneous osteonecrosis of the knee: the result of subchondral insufficiency fracture. J Bone Joint Surg (Am) 82:858–866
Lecouvet FE, Vande Berg BC, Maldague B, Lebon J, Jamart J, Saleh M, Noel H, Malghem J (1998) Early irreversible osteonecrosis versus transient lesions of the femoral condyles: prognostic value of subchondral and marrow changes on MR imaging. AJR 170:71–77
Stäbler A, Glaser C, Reiser M (2000) Musculoskeletal MR: knee, Eur Radiol 10:230–241
Lee JK, Yao L (1988) Stress fractures: MR imaging. Radiology 169:217–220
Anderson MW, Greenspan A (1996) Stress fractures. Radiology 199:1–12
Narváez J, Narváez JA, Rodríguez-Moreno J, Roig-Escofet J (2000) Osteonecrosis of the knee: differences among idiopathic and secondary types. Rheumatology 39:982–989
Yamamoto T, Bullough PG (2000) Subchondral insufficiency fracture of the femoral head and medial femoral condyle. Skeletal Radiol 29:40–44
Lafforgue P, Daumen-Legré V, Clairet D, Daver L, Acquaviva PC (1996) Insufficiency fractures of the medial femoral condyle. Rev Rhum (Engl Ed) 63:262–269
Satku K, Kumar P, Chacha PB (1990) Stress fracture around the knee in elderly patients. A cause of acute pain in the knee. J Bone Joint Surg (Am) 72:918–922
LeGars L, Savy JM, Orcel P et al. (1999) Osteonecrosis-like syndrome of the medial tibial plateau can be due to a stress fracture. MR findings in 13 patients. Rev Rhum (Engl Ed) 66:323–330
Sokoloff RM, Farooki S, Resnick D (2001) Spontaneous osteonecrosis of the knee associated with ipsilateral tibial plateau stress fracture: report of two patients and review of the literature. Skeletal Radiol 30:53–56
Dieppe P (1998) Osteonecrosis: one case of sudden worsening of knee pain in osteoarthritis. In: Klippel JH, Dieppe PA (eds) Rheumatology. Mosby, London, pp 1–2
Norman A, Baker ND (1978) Spontaneous osteonecrosis of the knee and medial meniscal tears. Radiology 129:653–656
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Narváez, J.A., Narváez, J., Lama, E.D. et al. Spontaneous osteonecrosis of the knee associated with tibial plateau and femoral condyle insufficiency stress fracture. Eur Radiol 13, 1843–1848 (2003). https://doi.org/10.1007/s00330-002-1775-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-002-1775-6