Abstract.
The purpose of this study was to determine and compare the effective dose of multidetector computed tomographic angiography (MDCT) and digital subtraction angiography (DSA) studies for diagnosing a pulmonary embolus (PE). Radiation exposure was measured as computed tomography dose index (MDCT) or as dose-area product (DSA) and was subsequently expressed in the quantity effective dose. Effective doses were obtained in 27 patients who underwent MDCT and in 12 patients who underwent DSA for suspected PE. The MDCT angiography was performed on a Siemens Volume Zoom CT scanner and DSA on a Philips Integris V-3000 system according to standardized protocols. Average effective dose for MDCT angiography of the pulmonary arteries (27 patients) was 4.2 mSv (range 2.2–6.0 mSv). Pulmonary DSA gained an average effective dose (12 patients) of 7.1 mSv (range 3.3–17.3 mSv). Our results show that the effective doses in MDCT angiography studies for PE are moderate and even slightly lower in comparison with pulmonary DSA in a comparable patient group. Variations in patient dose are smaller for MDCT, probably because this procedure can be more strictly protocolized. Patient dose should not be restrictive in the discussion of CTA replacing DSA for diagnosing PE.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
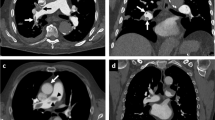
Spiral computed tomography angiography (CTA) of the pulmonary arteries is rapidly gaining acceptance as a useful diagnostic test for suspected pulmonary embolism (PE). As a noninvasive and quick procedure, it can detect or rule out PE by direct imaging of the intra-vascular clot [1, 2, 3]. In addition, CTA can provide the alternative diagnosis to explain signs and symptoms in those patients that have no PE [4, 5]. The diagnostic value of spiral CT is likely to improve with the introduction of the new multi-row detector technology. Multi-row Detector spiral CT (MDCT), when compared with conventional single-row detector spiral CT (SDCT), allows the use of much thinner imaging sections (e.g., 1 vs 3 mm) which will improve the visualization of smaller vascular detail [5, 6] (and also, as it seems, of small isolated sub segmental PE [7], currently the Achilles' heel of spiral CT [3]). Furthermore, MDCT can cover during a single breathhold the entire thorax instead of the more limited area that can be covered by SDCT, typically from the top of the diaphragm to the top of the aortic arch.
With the advent of MDCT, concern has been raised about radiation exposure. It is feared that the combination of using multiple high-resolution, high-quality thin imaging sections for a large area of coverage will lead to unacceptably high radiation dose to the patient. Rational discussion of this topic, however, is hampered by a lack of quantitative dosimetric data.
To address this issue, we calculated effective dose for spiral CT of the pulmonary arteries. This was done for the current imaging protocol on an MDCT scanner. These data were compared with the radiation exposure for the diagnostic examination that spiral CT for PE is most likely to replace, i.e., pulmonary digital subtraction angiography.
Materials and methods
Patients
For the evaluation of patient exposure all relevant CT parameters were registered from 27 consecutive pulmonary MDCT angiography examinations performed ( at the Erasmus MC in the period February to August 2000. The 27 patients (14 men, 13 women) were aged 51.8±19 years (age range 18.3–91.4 years).
Parameters necessary for an evaluation of patient dose during pulmonary digital subtraction angiography (DSA) were derived from 12 consecutive examinations performed at the LUMC in the same period. These 12 patients were aged 48±17 years (age range 17–74 years).
Imaging protocols
Multi-row detector spiral CTA of the pulmonary arteries
Patients underwent MDCT examinations on a Siemens Volume Zoom Plus 4 scanner (Siemens, Erlangen, Germany) which uses four parallel detector rows simultaneously. The Scanner software was work-in-progress releases with continuous updates from version VA20 and later. Care Dose software was not installed in this system. Scans were made using 120 kV, the tube rotation time was 0.5 s, and scan collimation was 4×1 mm. The entire thorax was imaged during a single breath hold. The scan volume was reconstructed using 1.25-mm-thick slices and a reconstruction increment of 0.6 mm. This protocol yields approximately 400 images per examination.
Pulmonary digital subtraction angiography
The standard protocol for pulmonary digital subtraction angiography (DSA) consists of four selective injections on a DSA system (Integris V-3000, Philips, Best, The Netherlands): Selective, unilateral studies in the anterior–posterior projectional views were supplemented with 30° contralateral oblique projections of each lung, separately. The selective angiograms were obtained using a field of view that is closely collimated around the left or right lung, respectively. The tube was positioned below the table, which is in its highest position, and the input screen of the image intensifier was almost in contact with the patient skin. A large 31- to 38-cm input screen was generally used with a 512×512 matrix. The acquisition was made with a frame rate of six frames per second and 2 -s delay to obtain multiple masks for subtraction. Image acquisition was stopped whenever opacification of the lung veins became apparent.
Assessment of patient radiation exposure
In this study, the radiation exposure of patients is expressed in the quantity effective dose. Effective dose is the weighted sum of equivalent doses in 23 radiosensitive organs and tissues. The tissue-weighting factors are defined by the International Commission on Radiological Protection (ICRP) publication 60 [8]. The effective dose can be calculated for a wide variety of exposure conditions, such as medical exposures, occupational exposures, or exposure to natural sources of radiation. A rough quantitative estimation of the radiation risk can be derived from the effective dose by multiplication with the ICRP risk coefficients for stochastic effects, i.e., for cancer and severe hereditary effects. However, the equivalent dose in organs and tissues cannot be measured for clinical examinations of patients; therefore, equivalent doses and effective dose have to be derived from suitable operational dosimetric quantities that can be easily measured, such as the CT dose index (CTDI, in mGy) [9] or the dose-area product (DAP, in Gy cm2) [10]. In this study, effective dose refers to a standard patient represented by a hermaphrodite mathematical phantom (weight 71 kg, height 1.74 m).
Multi-row detector spiral CTA of the pulmonary arteries
Effective dose was assessed by performing measurements of the CTDI free-in-air and subsequent application of effective dose conversion factors. Dose measurements yielded the actual normalized CTDI free-in-air for the Siemens Volume Zoom Plus 4 CT scanner. The measurements of CTDI were performed along the center of rotation of the scanner using a calibrated Capintec CT probe, model PC-4P, and a Keithley 35050A dosimeter. In this study we assessed effective dose by application of the dose conversion factors of the British National Radiological Protection Board [11] in combination with the CT dosimetry spreadsheet for effective dose calculations of the British ImPACT group [12]. Their CT dosimetry spreadsheet provides a practical interface for calculations with the National Radiation Protection Board (NRPB) dose conversion factors and it also provides CT scanner matching, i.e., recent CT scanners for which no NRPB dose conversion factors are available yet are matched with older scanners with known conversion factors. This CT scanner matching takes into account the differences in dose distribution due to differences in beam quality and beam shaping.
For the calculation of effective dose for the individual patients additional information was collected, i.e., the clinical tube current (mA; average, range), the actual anatomical landmarks of the scan (start and end position), and the table feed (mm/rotation).
Pulmonary digital subtraction angiography
The operator's display of the Integris V-3000 is equipped with a DAP readout and was recorded by the radiographer after each procedure. The DAP readout was corrected with an experimentally determined calibration factor [10]. Effective dose conversion factors, i.e., effective dose normalized to DAP (mSv/Gy cm2), were derived by means of Monte Carlo calculations with the PCXMC software [13]. These dose conversion factors were calculated separately for fluoroscopy and for angiography of both lungs, taking into account the specific tube voltage, beam filtration, and projection.
Results
The mean tube charge for MDCT angiography was 124±13 mAs per rotation (range 90–160 mAs). Pitch varied from 6 to 8, resulting in a table speed of 12–16 mm/s. The Z-axis coverage varied with patient physique and ranged from 13 to 36 cm (mean 22.6±6.0 cm). The measured normalized CTDI free-in-air for the MDCT angiography of the pulmonary arteries was 0.20 mGy/mAs (tube voltage 120 kVp, rotation time 0.5 s, collimation 4×1 mm), where the tube charge (mAs) is the rotation time (s) multiplied by the actual tube current (mA). The CTDI is expressed as absorbed dose to air.
The number of images per examination used in the dosimetric analysis of pulmonary DSA was 183 (range 157–237), based on the average taken from 12 actual patient studies. The average fluoroscopy time was 8 min (range 3–33 min).
The effective doses of the examinations under consideration are provided in the Table 1 for MDCT and in Table 2 for pulmonary DSA. Average effective dose for MDCT angiography of the pulmonary arteries (27 patients) was 4.2 mSv (range 2.2–6.0 mSv). Pulmonary DSA gained an average effective dose (12 patients) of 7.1 mSv (range 3.3–17.3 mSv).
Discussion and conclusion
Assessment of new modalities for X-ray imaging should involve diagnostic accuracy as well as patient dose. This study concentrates on patient dose during MDCT angiographic examinations for PE since this aspect has been somewhat neglected until now. Uncertainty about patient exposure gives room for the view that MDCT angiographic studies, compared with DSA, for PE, must result in unacceptably high radiation dose. This concern is often expressed, but our results indicate that this is not correct. The lack of published data on this subject can also provide problems for medical ethics committees. They might decline studies that use CTA because of the supposed high patient dose. This study puts the patient dose during MDCT angiographic examinations for PE in perspective and in case of biomedical research the medical ethics committees should regard the level of risk for this procedure as minor to intermediate (see also [14]). The requirements for societal benefit of such examinations that are formulated by the ICRP are that the research will be directly aimed at the cure or prevention of disease.
It is illustrative to compare the effective dose from MDCT angiography for PA with other exposures that are summarized in the UNSCEAR 2000 report [15]. This UNSCEAR report gives for example 12 mSv as a typical value for the effective dose from all types of angiographic procedures. Typical effective doses for lung perfusion scintigraphy (99mTc) are 1.1 and 0.2–0.4 mSv for lung ventilation scintigraphy (99mTc or 81mKr). Average worldwide exposure to natural radiation sources, expressed as an annual effective dose, is 2.4 mSv/y, with a typical range due to regional differences of 1–10 mSv/y. The radiation exposure of 4.2 mSv from MDCT angiography for diagnosing PA is well within this range of exposures. Being only slightly higher than the annual background and well below the exposure from conventional angiographic (DSA) procedures, the patient dose is, besides patient size and/or body mass index (BMI), also influenced by variations in study protocols and differences in CT scanners and DSA equipment. In our study BMI was not collected. Variations in milliamperes and effective dose are also a result of small adjustments to the scan protocol by our technicians. They check patient size and ability for breathhold. These more or less individualized scan protocols result in better images, reduction in motion artifacts, and dose differences [16, 17]. Especially in DSA there may be considerable variability among centers in the protocols used. Radiation dose may be lower than in our institution, e.g., whenever less projectional views are generally obtained, or whenever lower frame rates are used. On the other hand, increased radiation dose will be encountered whenever additional superselective injections will be made or when higher frame rates are used, e.g., on cardiac angiography systems. The relatively small number of patients in this study could be considered a limitation. The variation in effective dose in our DSA group was high; however, since the introduction of MDCT the necessity to perform DSA studies for diagnosing PE is limited to a very small number of patients in whom MDCT is inconclusive or not possible. Limited time made us decide to use only the patients in the period described. We do not believe the data would be significantly different in larger patient groups.
With the rapidly increasing use of multidetector CT and especially the angiography and multi-phase applications, further investigation is needed to determine the magnitude of radiation dose in these studies. The opportunity to establish strict examination protocols for CTA helps to reduce effective dose and helps to achieve more consistent image quality.
References
Van Rossum AB, Pattynama PMT, Tjin A, Ton ER, Treurniet F, Arndt JW, Van Eck B, Kieft GJ (1996) Spiral CT angiography for pulmonary embolism: validation in 149 patients. Radiology 201:467–470
Remy-Jardin M, Remy J, Deschildre F, Artaud D, Beregi JP, Hossein-Foucher C, Marchandise X, Duhamel A (1996) Diagnosis of pulmonary embolism with spiral CT: comparison with pulmonary angiography and scintigraphy. Radiology 200:699–706
Rathbun SW, Raskob GE, Whitsett TL (2000) Sensitivity and specificity of helical computed tomography in the diagnosis of pulmonary embolism: a systematical review. Ann Intern Med 132:227–232
Van Rossum AB, Pattynama PMT, Mallens WC, Heyermans HGM, Hermans J (1998) Can helical CT replace scintigraphy in the diagnostic process in suspected pulmonary embolism? A retrospective–projective cohort study focusing on total diagnostic yield. Eur Radiol 8:90–96
Remy-Jardin M, Remy J, Baghaie F, Fribourg M, Artaud D, Duhamel A (2000) Clinical value of thin collimation in the diagnostic workup of pulmonary embolism. Am J Roentgenol 75:407A1 1
Ghaye B, Szapiro D,Mastora I, Delannoy V, Duhamel A, Remy J, Remy-Jardin M (2001) Peripheral pulmonary arteries: How far in the lung does multi-detector row spiral CT allow analysis? Radiology 219:629–636
Baile EM, King GG, Muller NL, D'Yachkova Y, Coche EE, Pare PD, Mayo JR (2000) Spiral computed tomography is comparable to angiography for the diagnosis of pulmonary embolism. Am J Respir Crit Care Med 161:1010–1015
ICRP (1991) 1990 recommendations of the International Commission on Radiological Protection. Publication 60. Pergamon, Oxford
Shope TB, Gagne RM, Johnson GC (1981) A method for describing the doses delivered by transmission X-ray computed tomography. Med Phys 8:488–495
Shrimpton PC, Wall BF (1982) An evaluation of the Diamentor transmission ionisation chamber in indicating exposure-area product (R cm2) during diagnostic radiological examinations. Phys Med Biol 27:871–878
Jones DG, Shrimpton PC (1991) Normalised organ doses for X-ray computed tomography calculated using Monte Carlo techniques. NRPB-SR250, Chilton
St. George's Hospital (2001) ImPACT CT Patient Dosimetry Calculator, version 0.99e, ImPACT, London
Servomaa A, Tapiovaara M (1998) Organ dose calculation in medical X-ray examinations by the program PCXMC. Radiat Prot Dosim 80:213–219
ICRP (1993) Radiological protection in biomedical research, a report by the International Commission on Radiological Protection. Publication 62. Pergamon, Oxford
UNSCEAR (2000) 2000 report, sources and effects of ionizing radiation, vol I: sources. United Nations Scientific Committee on the Effects of Atomic Radiation
Wilting JE, Zwartkruis A, van Leeuwen MS, Timmer J, Kamphuis AG, Feldberg M (2001) A rational approach to dose reduction in CT: individualized scan protocols. Eur Radiol 11:2627–2632
Huda W, Scalzetti EM, Levin G (2000) Technique factors and image quality as function of patient weight at abdominal CT. Radiology 217:430–435
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kuiper, J.W., Geleijns, J., Matheijssen, N.A.A. et al. Radiation exposure of multi-row detector spiral computed tomography of the pulmonary arteries: comparison with digital subtraction pulmonary angiography. Eur Radiol 13, 1496–1500 (2003). https://doi.org/10.1007/s00330-002-1753-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-002-1753-z