Abstract
To evaluate serum levels of IL6 in patients with Kawasaki disease and compare it with CRP, and to assess the role of these biomarkers in predicting coronary changes and resistance to the first-line therapy of this disease in a subset of Indian population. A single centre prospective observational study was conducted amongst all Kawasaki disease patients for a period of 18 months from January 2017 at Institute of Child Health, Kolkata. Serum IL6 and CRP were compared at diagnosis and after 48 h of administering IVIG in patients who developed coronary changes with those who did not and also among the responders and non-responders to IVIG, the first-line therapy given to these patients. Out of total 72 patients of KD [mean age of presentation: 24 months, M:F = 1.22:1], 30% (n = 22) had coronary artery involvement (CALs), and 15% (n = 11) were IVIG non-responders. Mean IL6 prior to IVIG in those with CALs was 143.60 pg/ml, which was about three times higher than in those without CALs (mean = 52.90 pg/ml), the difference being significant (p < 0.01). Mean CRP values also were significantly raised in patients with CALs (p < 0.01) whereas post-IVIG levels of mean serum IL6 was found to be 108.15 pg/ml in non-responders which was about 17 times raised than that in the responders (mean IL6 = 6.22),the difference again was statistically significant (p < 0.001).Also, ROC analysis revealed a sensitivity and specificity of 81.0% and 82.0%, respectively, for IL6; 72% and 74%, respectively, for CRP for predicting CALs. This study also shows a sensitivity of 72% and specificity of 68% for IL6 in predicting IVIG resistance whereas that of CRP being 90% sensitive and 36% specific. These results suggest that higher levels of IL-6 and CRP at diagnosis are associated with occurrence of CALs and IVIG resistance in KD patients. Using the cutoff for IL6 and CRP from our study, chances of developing CALs and IVIG resistance can be predicted, which might prevent the development of future complications like aneurysms in such patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kawasaki disease is a febrile vasculitis affecting mainly the young children, characterised by a constellation of symptoms that has special predilection for the coronaries [1]. Since its first description by Dr. Tomisaku Kawasaki back in 1967, despite extensive research, the aetiology of KD remains enigmatic till date [1, 2]. Multiple postulates regarding the etiopathogenesis have been suggested time and again, one of them being the abnormal activation of the immune system and secretion of cytokines [3]. Interleukin 6 is one such inflammatory cytokine produced in response to activation of monocytes and macrophages in the acute phase of KD, on which studies are lacking from our country [4]. This is a proinflammatory cytokine that incites other inflammatory markers, C-reactive protein being one of them.
The inflammatory changes that result in coronary arteriopathy occur in a step-by-step fashion as described by necrotizing arteritis, subacute/chronic vasculitis and finally luminal myofibroblastic proliferation (LMP), producing a spectrum of coronary changes ranging from mild, reversible dilations to severe stenosis and giant aneurysms [5]. Various studies have been done from different countries to predict the risk factors for occurrences of these coronary artery lesions(CALs) which led to the formulation of many scoring systems comprising of different parameters like age, serum albumin, sodium, CRP, etc., but none of them apply universally [6].
It was also seen that around 17% KD patients did not respond to the first dose of IVIG and various predictors of resistance, hence, have been suggested and incorporated into the scoring systems [7]. Due to lack of universal acceptance of any one of these scoring systems, prediction of resistant KD cases becomes more difficult. Thus, we need to investigate new novel markers which might help us predict resistance and probability of developing CALs with more accuracy. Hence, we studied the pattern of IL6 in relation to the coronary changes and treatment responses, which may help us in predicting prognosis and targeting new treatment strategies.
Methods
This is a prospective observational study conducted at Institute of Child Health, Kolkata, a tertiary referral hospital in eastern India. Children admitted between January 2017 and June 2018 with complete, incomplete and atypical KD were included and followed up from a period of 1 to 18 months after their discharge depending on time of the disease onset and study period, in the rheumatology OPD of our Institute. Complete, incomplete and atypical KD were diagnosed by fulfilling the classification criteria defined by the AHA 2004 guidelines, and subsequently, by the AHA 2017 guidelines [5]. Paired venous blood samples for interleukin 6 (IL6) and C-reactive protein (CRP) together with other necessary investigations, were drawn and evaluated at the biochemistry department at diagnosis and 48 h after administering IVIG. The serum concentrations of CRP were quantitatively determined by particle-enhanced turbidimetry on the Roche Integra 400 Plus© biochemistry analyzer. Linearity was till 200 mg/L. Biological reference interval was < 5 mg/L and serum IL6 was measured on the Roche cobas e411© immunoassay analyser with a linearity till 5000 pg/ml and biological reference interval of < 7 pg/ml.
2D Echocardiography was done at diagnosis, after 2 weeks of IVIG and at 6-week follow-up by an experienced paediatric cardiologist at our Institute. The coronary artery lesions (CALs) and positive echocardiography findings for diagnosis of incomplete KD, as defined by the AHA 2004, and subsequently 2017 guidelines, were followed [5]. Patients, who had CALs at diagnosis, were followed up with echocardiography every 3–5 days to review for any evidence of further progression.
The responder group included patients who received a single dose of IVIG (2 g/kg) treatment and had no reappearance of fever 48 h after IVIG, while the non-responder group included patients who had persistent or recrudescent fever after 48 h of IVIG and needed a second dose of IVIG or Infliximab [6].
Ethics statement
Data were collected and given for analysis to a competent biostatistician. For statistical analysis, SPSS 24.0 © software was used. Normality of data was checked before applying parametric tests. Data had been summarised as mean and standard deviation for numerical variables and counts for discrete data and percentages for categorical variables. t tests were used for a difference in mean involving independent samples or unpaired samples. Unpaired categorical data were compared by Chi-square test or Fischer’s exact test, as appropriate.
Receiver operating characteristic (ROC) curves were derived from the pre-IVIG serum CRP and IL6 levels in all KD patients. In the ROC curve, the sensitivity and specificity, for the prediction of CALs and IVIG resistance in the KD patients were calculated by combining the optimal cutoff values for each cytokine using the Youden index. The difference was considered significant at P values less than 0.05. All data analyses were performed using SPSS© version 24.0 software.
This study was approved by the Institutional Ethics Committee (IEC) (IEC Regn No. ECR/359/Inst/WB/2013) of Institute of Child Health, Kolkata in November 2016 (Ethical clearance protocol no. IEC/107a/2016 vide letter ICH/33/2016 dated 29th Nov 2016).
Results
74 patients were diagnosed with KD during this period of 18 months. 2 were excluded as they did not consent and 72 patients were finally recruited. Among the study population, 31(43.1%) patients were female and 41(56.9%) were male with a M:F ratio of 1.22:1, 79.2% belonged to the age group 1–5 years. Median age was 19 months with Inter-quartile range (IQR) of 13.75–30.5 months. Seasonality was observed in disease occurrence with maximum incidence in the months of April and May (15% of admissions) and lowest in October–November. The mean duration fever at presentation (mean ± S.D.) was 8.9167 ± 2.8222 days.
83% patients were diagnosed as complete KD and 17% were diagnosed as incomplete KD. 22 (30.6%) patients had coronary artery involvement. The most common artery to be involved was the LAD followed by RCA. Majority had small aneurysms (z score between 2.5 and 5); however, two (2.7%) had giant aneurysms involving the LAD. In the echocardiography follow-up at 2 weeks, it was seen that the giant aneurysms increased in size as measured by z scores and three patients who had small/medium aneurysms previously still had a z score > 2.5 but in decreasing trend and rest all had normal z scores (< 2) by 2 weeks. At 6 weeks, none had increasing z scores, patients with giant aneurysms (also received Infliximab) had decreased scores compared to the earlier one and rest all had normal z scores (< 2).
Regarding the treatment outcomes, 61(84.7%) patients responded to the first dose of IVIG characterised by defervescence. 11(15.3%), however, did not respond to first dose IVIG and were given second-line therapy with Infliximab.
Demographic parameters like age, sex or differences in the mean duration of fever were not statistically significant among responders and non-responders. All non-responders had coronary artery involvement.
The difference between the mean pre-IVIG CRP in the responders and non-responders was not statistically significant (p = 0.1973), although the mean post-IVIG CRP of non-responders was significantly higher (p < 0.0001), compared to responders. Similarly, mean pre-IVIG IL6 was also not found to be significantly different in responders and non-responders (p = 0.2242). But the mean post-IVIG IL6 was significantly higher in non-responders (p < 0.0001) (Table 1).
We compared both these levels in pre- and post-IVIG sera with coronary involvement and found that mean pre-IVIG CRP and IL6 in patients without any coronary artery involvement were significantly (p < 0.0001) less compared to patients with CALs (Table 2).
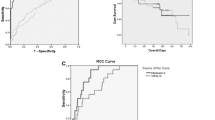
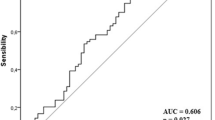
We also performed ROC curve analysis for pre-IVIG CRP and IL6 in predicting CALs and IVIG resistance and using Youden index, optimal cutoff for CRP was 40 mg/L with a sensitivity of 90%, specificity of 36.0% and area under the curve of 0.624 (95% CI 0.50–0.73) for predicting IVIG resistance (Fig. 1), and pre-IVIG serum IL6 had a sensitivity of 72% and specificity of 68% with area under the curve of 0.702 (95% CI 0.58–0.80) for predicting IVIG resistance at > 75 pg/ml cutoff value (Fig. 1) (Table 3).
For predicting CALs, pre-treatment IL6 had a sensitivity of 81.0% and specificity of 82.0% at the cutoff value of > 75 pg/ml (area under the curve 0.788, 95% CI 0.67–0.87) (Fig. 1), whereas pre-IVIG serum CRP had a sensitivity of 72.0% and specificity of 74% at 78 mg/L cutoff value (area under the curve 0.87, 95% CI 0.77–0.93) (Fig. 1)(Table 3).
Limitations of the study
-
1.
Small sample size.
-
2.
IL-6 estimation is relatively expensive.
Discussion
IL-6 is a pleotropic cytokine that is produced by a variety of cells and acts on a wide range of tissues exerting a growth inducing, growth inhibitory and differentiation-inducing effects depending on the nature of the target cells. IL-6 leads to B cell differentiation, induction of acute-phase proteins in the liver cells like CRP and various growth promoting as well as inhibiting effects on the hematopoietic stem cells and malignant cells [7]. Hence, IL-6 may play a role in the pathogenesis of many autoimmune diseases, plasma cell neoplasia and glomerulonephritis [8]. Kawasaki disease, as suggested by various researchers, is a condition characterised by dysregulated inflammation in the blood vessels as evident from the high levels of CRP, and ESR found in the acute phase. Previous studies on IL-6 in patients of Kawasaki disease have showed elevated levels of serum IL-6 in all patients in acute phase of KD and lower levels in subacute phase [9], and there was a significant difference in the levels between those with and without coronary artery aneurysms during the first week [10].
Studies also have found that there were no significant differences between the responders and non-responders with regard to age, gender and fever duration before treatment; however, significant difference has been demonstrated in the levels of markers like CRP, IL6, IL18, pro BNP, etc., in the sera of KD patients [11].
The present study was done to compare IL6 with well-known marker, CRP and how it changes with the disease severity as seen in the form of CALs and resistance to IVIG in the Indian population. Our results showed significantly higher levels of these markers in patients who later developed CALs and also in the non-responders, in contrary to those who did not have CALs or resistance to IVIG. We also compared demographic factors like age, sex and duration of fever and did not find any significant relation with development of CALs or disease refractoriness.
Another previous study on cytokines and Kawasaki disease showed that prior to treatment with IVIG, the level of IL-6 among other cytokines was slightly lower in IVIG non-responders compared to IVIG responders, but post-IVIG, the IL-6 levels were significantly higher in IVIG non-responders than in IVIG responders; thus, suggesting that a slower decrease in IL-6 levels after treatment with IVIG may be related to IVIG resistance and the occurrence of CALs in these KD patients and the attenuation of proinflammatory cytokine responses, especially IL-6, following infusions of IVIG may play an integral role in the rapid resolution of symptoms and in reduced levels of acute-phase proteins in children with KD [12]. In our study population, we found similar results.
We tried to find optimum cutoff values for CRP and IL6 prior to the treatment with IVIG in predicting CALs and IVIG resistance in Indian population and found that pre-IVIG serum CRP had a sensitivity of 90% and specificity of 36.0% for predicting IVIG resistance at cutoff value of 40 mg/L but pre-IVIG serum IL6 had a sensitivity of 72% and specificity of 68% for predicting IVIG resistance at > 75 pg/ml cutoff value which shows better accuracy of IL6 in predicting IVIG resistance than CRP.
For predicting CALs, on the other hand, pre-treatment IL6 had a sensitivity of 81.0% and specificity of 82.0% when the cutoff value was > 75 pg/ml whereas pre-IVIG serum CRP had a sensitivity of 72.0% and specificity of 74% at 78 mg/L cutoff value.
Hence, it can be suggested from the present study that an acute-phase serum IL6 level of > 75 pg/ml is associated with higher likelihood of developing coronary changes and IVIG resistance in our population subset. Furthermore, it showed a better predictability than CRP.
Hence, to conclude, the present study shows that significantly higher serum IL6 and CRP levels are associated with CALs and resistance to IVIG. Serum IL6, therefore, can be used as a new novel marker for prediction of coronary artery involvement and resistance to IVIG.
References
Kawasaki T (1967) Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children. Jpn J Allergol 16:178–222
Jamieson N, Singh-Grewal D (2013) Kawasaki disease: a clinician’s update. Int J Pediatr 2013:645391
Manlhiot C, Christie E, McCrindle BW, Rosenberg H, Chahal N, Yeung RS (2012) Complete and incomplete Kawasaki disease: two sides of the same coin. Eur J Pediatr 171:657–662
Clark SC (1989) Interleukin-6. Multiple activities in regulation of the hematopoietic and immune systems. Ann NY Acad Sci 557:438–443
McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, Baker AL, Jackson MA, Takahashi M, Shah PB, Kobayashi T, Wu MH, Saji TT, Pahl E, American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Surgery and Anesthesia; and Council on Epidemiology and Prevention (2017) Diagnosis, treatment, and long-term management of kawasaki disease: a scientific statement for health professionals from the american heart association. Circulation 135(17):e927–e999. https://doi.org/10.1161/CIR.0000000000000484
Egami K, Muta H, Ishii M et al (2006) Prediction of resistance to intravenous immunoglobulin treatment in patients with Kawasaki disease. J Pediatr 149:237–240
Suganami Y, Kawashima H, Hasegawa D et al (2008) Clinical application of rapid assay of serum interleukin-6 in Kawasaki disease. Pediatr Int 50:264–266
Hirano T, Yasukawa K, Harada H, Taga T, Watanabe Y, Matsuda T, Kashiwamura S, Nakajima K, Koyama K, Iwamatsu A et al (1986) Complementary DNA for a novel human interleukin (BSF-2) that induces B lymphocytes to produce immunoglobulin. Nature 324(6092):73–76
Kim DS (1992) Serum interleukin-6 in Kawasaki disease. Yonsei Med J 33(2):183–188
Rawat Amit, Singh Surjit (2015) Biomarkers for diagnosis of kawasaki disease. Indian Pediatr 52:473–474. https://doi.org/10.1007/s13312-015-0658-2
Sato S, Kawashima H, Kashiwagi Y, Hoshika A (2013) Inflammatory cytokines as predictors of resistance to intravenous immunoglobulin therapy in Kawasaki disease patients. Int J Rheum Dis 16:168–172
Wang Y, Wang W, Gong F, Fu S, Zhang Q, Hu J (2013) Evaluation of intravenous immunoglobulin resistance and coronary artery lesions in relation to Th1/Th2 cytokine profiles in patients with kawasaki disease. Arthritis Rhuem 65(3):805–814
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The above authors Dr. Alolika Nandi, Dr. Priyankar Pal and Dr. Surupa Basu declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nandi, A., Pal, P. & Basu, S. A comparison of serum IL6 and CRP levels with respect to coronary changes and treatment response in Kawasaki disease patients: a prospective study. Rheumatol Int 39, 1797–1801 (2019). https://doi.org/10.1007/s00296-019-04375-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-019-04375-9