Abstract
There is a need for better definition of polyarteritis nodosa (PAN) subphenotypes and the influence of ethnicity and geography. This study is aimed to study the demographic and clinical features of PAN cohorts from the UK and Turkey (TR) and to compare and contrast disease characteristics. A retrospective survey of databases from two vasculitis centres between 1990 and 2016 for PAN patients fulfilling the EMEA Vasculitis Classification algorithm. All paediatric-onset adult patients met the Ankara 2008 (EULAR/PReS endorsed) criteria for childhood PAN. Those with typical angiographic and/or histopathologic findings consistent with PAN were included. 93 (M/F: 51/42) patients (UK: 47, TR: 46) were included. Three were HBV-related, 20 (21.5%) had paediatric onset and 16 (16.5%), cutaneous PAN. TR patients had younger age of disease onset 44 (28.5–59.0) vs. 24.5 (11.8–40.5), p = 0.002. Twelve (26%) of TR patients had monogenic disease (Familial Mediterranean Fever association (n = 7), deficiency of adenosine deaminase 2, DADA2, (n = 5). No difference was found in phenotype between paediatric and adult onset patients except for frequency of cutaneous lesions (p = 0.002). During a median 67.5 (32–126) months follow-up, 13 patients died (12.7% in UK vs. 15.2% in Turkish cohorts). No difference was found between two cohorts in relation to relapse rate, death and vasculitis damage index. This study defined a diagnosis of PAN according to the EMEA algorithm. The TR group had a younger age of disease onset and more cases of monogenic disease; however, disease extent, relapse rate, damage index and death rates were similar between groups.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Polyarteritis nodosa (PAN) was described in 1866 by Kussmaul and Maier [1]. The diagnosis of PAN can be challenging since there are no specific laboratory tests. The most frequent clinical features include non-specific constitutional symptoms, neurologic and cutaneous manifestations, abdominal pain, and hypertension [2]. Occasionally PAN and anti-neutrophil cytoplasm antibody (ANCA)-associated vasculitis can exhibit clinically and pathologically indistinguishable necrotizing medium and small arteritis [3]. Diagnosis relies on angiographic or histologic demonstration of a medium-sized vessel arteritis, negative ANCA, absence of mucocutaneous lymph node syndrome features, and no evidence for glomerulonephritis. Earlier definitions of PAN, such as the 1990 ACR classification, included microscopic polyangiitis (MPA) within the PAN subgroup but since 1993, MPA has been regarded as a separate entity within the ANCA vasculitis subgrouping.
According to the 2012 revised international Chapel Hill consensus conference nomenclature of vasculitides, PAN is classified as idiopathic systemic PAN and a separate “secondary” hepatitis B virus (HBV)-associated PAN [3]. Moreover, various subgroups of PAN or PAN-like diseases are now recognised, including HBV and hepatitis C virus (HCV)-associated PAN, Familial Mediterranean Fever (FMF) associated PAN, Deficiency of Adenosine DeAminase 2 (DADA2) with PAN-like disease, cutaneous PAN, and drug-induced PAN (e.g. minocycline) [2,3,4,5,6,7]. On the other hand, we lack data to support the observation of different clinical features between childhood and adult-onset PAN [8].
Compared to other vasculitides little is known about the disease due to its rarity. The estimated annual incidence of PAN is 2–9/million adults [9]. In a large multinational observational study of vasculitis, DCVAS (Diagnostic and Classification criteria in VAsculitis Study) PAN was the least frequent vasculitis to be reported [10]. Ethnic and geographical affects on the development of the disease are not clear. Although the clinical characteristics and outcomes of PAN have been reported previously, there are no studies that have directly compared PAN in different countries.
This study aimed to define the demographic and clinical characteristics of PAN and to identify differences between two geographic regions, the UK and Turkey. It also aimed to further characterise differences between PAN and two subgroups: paediatric onset PAN and cutaneous PAN.
Materials and methods
Patients
In this retrospective observational study, data were extracted from two centres (Addenbrooke’s Hospital, Cambridge in the UK & Hacettepe University Vasculitis Centre, Ankara in Turkey) during a period between 1990 and 2016. We excluded 21 of 68 patients from Addenbrooke’s Hospital and 14 of 60 from Hacettepe University due to missing data.
The medical ethics committee of Hacettepe University approved the study for Turkish cohort (28.02.2017, GO 17/157-23). For the UK cohort, in accordance with UK National Health Service Research Ethics Committee guidelines, ethical approval was not required for this work because it comprises retrospective data and all treatment decisions were made prior to our evaluation. Due to retrospective design of the study, patient’s written informed consent to publish the material could not be obtained.
Patients that had a diagnosis of PAN according to the European Agency for the Evaluation of Medicinal Products (EMEA) Vasculitis Classification algorithm [11] were included. The EMEA algorithm mandates exclusion of ANCA associated vasculitis [Granulomatosis with polyangiitis (GPA/Wegener’s), Microscopic polyangiitis (MPA) and Eosinophilic granulomatosis with polyangiitis (EGPA/Churg-Strauss)] and requires the presence of typical angiographic or histological features consistent with PAN.
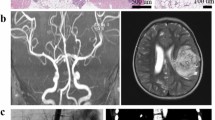
An expert radiologist confirmed the angiographic features of PAN in each case characterized by segmental narrowing, dilatation, occlusion or aneurysms of visceral arteries in the absence of evidence for atherosclerotic vessel changes or vasculitis mimics such as fibromuscular dysplasia. Patients with isolated small vessel vasculitis and other single organ vasculitis were excluded.
Patients were sub-classified as:
-
If there was only skin involvement with or without musculoskeletal and general constitutional symptoms they were classified as having “cutaneous only” PAN.
-
If there was evidence for any organ system involvement including neurological (neuropathy, mononeuritis multiplex, cranial angiographic findings, transient ischaemic attack), gastrointestinal, renal or testicular involvement they were classified as systemic PAN.
-
Patients who were diagnosed with PAN as a child (< 16 years old) were considered to have paediatric onset PAN.
-
Monogenic PAN/PAN-like disease included those with DADA2 or FMF.
Assessment
Demographic data included age, sex, time to diagnosis, age at disease onset and consanguinity. Additionally, evaluation of retrospective data included the findings of FMF and DADA2 to assess possible relationship with these diseases established. Not all of the patients are tested routinely, but in case of suspicion tests were done in Turkish group. Phenotypic data included serum erythrocyte sedimentation rate (ESR), creatinine, and C-reactive protein (CRP) and organ involvement. All data were abstracted from the written and electronic medical records.
The disease extent index (DEI), originally developed for GPA/Wegener’s is a simple list of organs involved and was used to assess disease extent (any of 10 major organ systems score 2/system, apart from joint involvement that scores 1) [12]. Organ involvement during disease course was established using modified DEI definitions. In case of renal involvement, disease-related hypertension and renal angiographic findings were used to identify the organ involvement. Similarly, mesenteric and hepatic artery involvement was used to identify gastrointestinal involvement. Involvement of new organs in the follow-up phase was also assessed.
Treatment
‘Response to therapy’ was determined according to documentation by the treating physician at last follow-up. ‘Failure’ was defined as absence of clinical remission, occurrence of new vasculitis manifestation(s) or death before remission was obtained. ‘Relapse’ was defined as recurrence of vasculitis requiring treatment change, increasing dose of glucocorticoids and/or addition of an immunosuppressant, IV pulsed methylprednisolone pulse, intravenous immunoglobulin, plasma exchange or therapeutic biologic.
Outcome measures
The prognostic Five-Factor Score (FFS), which includes parameters predictive of poorer outcome and mortality (creatinine > 140 mmol/dl, proteinuria > 1 g/24 h, gastrointestinal involvement, cardiomyopathy, CNS involvement) was estimated at diagnosis [13]. Remission status, relapses, time to first relapse, vasculitis damage index (VDI) [14] at last visit, death, time to death and causes of death were collected for each patient. Data were acquired from patients’ medical charts and computer records.
Statistics
Descriptive statistics (means, percentages, median and interquartile range, etc.) were used to summarize the data. The data from the UK and Turkish patients was compared to identify the key differences in clinical features, demographics, laboratory tests and treatments provided using Chi-square, or Mann Whitney U test and Wilcoxon rank-sum tests. Subgroup analysis was carried out to identify common features and distinct differences in the clinical characteristics of PAN disease subgroups, including paediatric-onset vs. adult-onset PAN.
The cumulative rates for survival and relapse were assessed by the Kaplan–Meier survival curve, and compared by log-rank test. Binary logistic regressıon models assessed risk factors for mortality and relapse. Risk factors for mortality and relapse were examined using uni-variable Cox proportional hazards models. Statistical analyses were performed using SPSS (Version 21) statistical package.
Results
Demographic and Clinical Characteristics
93 (M/F: 51/42) patients (UK: 47, Turkey: 46) were included. Age at disease onset was 36.0 (20.0–49.8, median, range) years. Of the combined cohort, Hepatitis B virus-related PAN was seen in three (3.2%), 20 (21.5%) patients had paediatric onset and 16 (16.5%) patients had cutaneous PAN. No patients had minocycline-related PAN.
Constitutional (87.7%), musculoskeletal (78.0%), and cutaneous (71.7%) manifestations were the most common clinical features. Renal and gastrointestinal involvements were seen in half of the patients (Table 1). Over 30% had new onset hypertension or exacerbation in HT. Totally 36 (38.8%) patients had neurologic involvement (polyneuropathy: 17, cerebrovascular event: 9, mononeuritis multiplex: 11).
None of the patients had ear/nose/throat (ENT) involvement. Three had ophthalmologic involvement (2 anterior uveitis, 1 scleritis). Pulmonary fibrosis (2 patients), cardiac involvement (3 patients) and pleural effusion (3 patients) were noted in a minority. The mean (SD) DEI score was 5.84 (2.4). Over 50% had FFS ≥ 1. Nine underwent abdominal surgery for PAN related gastrointestinal complications (mesenteric ischemia, bowel infarct/perforation and periduodenal mass/obstruction).
Tissue biopsy performed in 75 (80.6%) patients confirmed the diagnosis in 61 (66%). Angiography (conventional, CT or MR) performed in 65 (69.8%) confirmed the diagnosis in 52 (55.9%). Viral DNA was detected in all patients with positive HBV serology.
Twelve patients (26%) of the Turkish cohort had an identified/suspected monogenic disease, FMF in 7, DADA2 in 5 patients. In sixteen patients, MEFV mutations were studied and seven had any of (M694V, M680I, V726A, E148Q) mutations. Four from the UK had features suspicious for a monogenic aetiology (two of them had stroke and all had livedoid rash), but this could not be confirmed in the current study.
Treatments
Oral glucocorticoids were widely used in both Turkey and the UK (95.6 and 93.6%, respectively; Table 2). Initial oral prednisolone doses were 60 mg/day in Turkey and 45 mg/day in the UK. Glucocorticoid tapering was slower in Turkey than in the UK, and oral prednisolone doses 6 months after initiation were 17.5 and 10 mg/day in Turkey and the UK.
The majority of patients received cyclophosphamide (65%) for induction therapy. Azathıoprine (62%) and Mycophenolate (58%) were also used. Seven of 93 (8%) had refractory disease. Biologics were used in 28 (30%), with rituximab and infliximab the mostly widely used (Table 2). All FMF patients received colchicine. HBV-related patients received antiviral agents together with immunosuppressive therapy.
Comparison of cutaneous PAN vs. systemic PAN
None of those with cutaneous PAN evolved into systemic PAN. There was a female predominance in cutaneous PAN in contrast to the weak male predominance seen in patients with systemic disease. No difference was found between groups with regards to constitutional or musculoskeletal symptoms; or in relation to the outcomes of response to treatment and relapse. Groups were not different in terms of response and relapse but death was more frequent in those with systemic PAN.
Comparison of paediatric-onset PAN vs. adult-onset PAN
Twenty patients had paediatric onset-PAN. All of the paediatric onset patients had cutaneous involvement compared to 47 (64.3%) of adult onset-PAN patients (p = 0.002). None of the other demographic and clinical features were different between the groups (data not shown).
Comparison of the UK and Turkish Cohort
The disease was predominantly seen in males in Turkey compared to the UK cohort (65.2 vs. 44.7%, p = 0.047). Turkish patients had a younger age at disease onset than UK patients Table 3. There was no difference in proportion of patients with paediatric onset disease between the two groups (17 vs. 26%, p = 0.287).
Cutaneous, musculoskeletal and constitutional manifestations were the most frequent features in both cohorts and these features were not statistically different between the Turkish and the UK groups (p > 0.05; Table 3). However, cutaneous PAN was more frequent in the UK group (25.5 vs. 8.6%, p = 0.031). Conversely, renal involvement was seen more frequent in the Turkish group (76.1 vs. 40.4%, p < 0.001). The median DEI was higher in the Turkish group [6.35 (2.3) vs. 5.3 (2.5, p = 0.05)].
Patient-related long-term outcomes
Patients were followed for a median of 68 (32–126) months. All patients except for two were followed for > 6 months. The median follow-up was comparable between cohorts (Table 2, p = 0.669).
Relapse
More than half of patients had one or more relapses (55.5% UK vs. 50% Turkey, p = 0.784). The median time to relapse was 12 (10–18) months. Survival analysis did not show any difference in the time to relapse between the two groups (Fig. 1, log-rank test, p = 0.387). In cox-regression models predictors such as age, sex, organ involvement, and genetic disease were not associated with relapses. There was a trend to more frequent relapses in cutaneous PAN.
Mortality
Thirteen patients died (12.7% in the UK vs. 15.2% in Turkish cohorts). There was no difference in survival curves between the two cohorts (log-rank test, p = 0.190). The 1-, 5- and 10-year survival rates of the UK cohort and Turkish cohort are shown in Fig. 2.
In cox-regression models, the aforementioned predictors including age, sex, organ involvement, and genetic disease along with the need for surgery were not associated with mortality. However, FFS score was related to mortality (p = 0.013). Five of thirteen patients with FFS = 2, and 5 of 37 patients with FFS = 1, had deceased (Fig. 3). Of the 13 that died, the cause of death was known in seven (Pneumonia: 2, renal failure & pneumonia: 1, malignancy: 3, heart failure: 1).
Other outcomes
Malignancy was observed in 9 (9.7%) patients. Non-melanoma skin cancers, three; colon cancer, two; lymphoma, chronic myelomonocytic leukemia, acute myeloblastic leukemia and malign mesenchymal tumour, one for each.
The median Vasculitis damage index (VDI) score was 1 (0–1) at the last follow-up visit, and comparable between the UK and Turkish groups (p = 0.632).
Discussion
This is the largest study defining a diagnosis of PAN according to the EMEA algorithm. We also present a comparison of PAN from two different geographic areas. The Turkish group had a younger age of disease onset and more cases of monogenic disease. Even though there were certain demographic, clinical characteristic and treatment differences; relapse rate, damage index and death rates were comparable between the two groups.
Cutaneous, musculoskeletal and constitutional manifestations were the most frequent features in both cohorts. Renal and gastrointestinal involvement was seen in about half of the patients. These frequencies were similar to a recent Mayo clinic PAN cohort [15]. However, over 70% of French cohort had high neurologic involvement, whereas in the UK cohort this was 34%, and half of Turkish group [2]. Cutaneous PAN patients were more frequent in the UK group and renal involvement more frequent in the Turkish group. However, disease extent index was similar between the cohorts.
PAN presents both in children and adults. The mean age at disease onset in previous studies was reported as in the 6th decade [15, 2]. Over 20% of our patients had a paediatric onset. Thus, Median age at disease onset of our patients was younger than previous cohorts (Mayo, 52.8 ± 15.8, French cohort 51.2 ± 17.3). Even though the frequency of paediatric onset patients were not different between the UK and Turkey cohorts, Turkey patients had a > 10 years younger disease onset.
Additionally, we evaluated if the patients had monogenic disease such as FMF and DADA2. Twelve (26%) of the Turkish cohort had an identified/suspected monogenic disease (FMF in 7, DADA2 in 5). Four patients from the UK had features suspicious for the above-mentioned monogenic diseases but this could not be confirmed in this retrospective study. The high consanguinity rate and the high prevalence of MEFV mutations in Turkey explain the high rate for these diseases in this cohort [16]. Again, in the Turkish cohort the presence of genetic factors that predispose to inflammation might have been effective in the younger onset due to the relevant genetic load.
Chronic HBV infection is associated with a subgroup of PAN. One-third of the French group had HBV-related PAN [2]. There were 7 (15%) patients with hepatitis B and 2 (4%) with hepatitis C in the Mayo PAN cohort [15]. We had three patients out of 91. This difference may relate to time of the observation period (French cohort was 1965, Mayo cohort was 1980, the present study 1990). However, rare frequency of our HBV-related patients is comparable to French data after 2002. Successful vaccination could result HBV-related PAN to less than 5% and to none of paediatric onset cases [17].
Cutaneous PAN was present in sixteen with a female predominance. Over 75% had constitutional and musculoskeletal features. No patients evolved into systemic PAN and this was only seen in one of 41 in the Mayo Clinic cohort. We also compared clinical features of paediatric to adult patients. The only difference was the higher frequency of cutaneous disease in the paediatric group.
Treatment routinely employed corticosteroids and had additional immunosuppressives, typically cyclophosphamide. Even though most had used cyclophosphamide, biologics were used in > 30% patients (more in the UK group). DADA2 patients received anti TNF treatment. Seven patients had refractory disease.
During follow-up, we evaluated relapses, mortality and malignancy. The relapse rates were similar in both cohorts and over half of patients had at least one relapse with a median time to relapse of 12 months. The Mayo group reported a 5-year cumulative rate of first relapse as 45.2% in cutaneous PAN, and only 9.6% in systemic PAN group [15]. The French cohort found relapse rates between 20–46% [2, 18, 19]. In the French study, 28.0% of the patients with non–HBV-related PAN relapsed with a mean 29.0 (43.3) months. Cutaneous PAN has a higher relapse tendency. The randomized trial ‘CHUSPAN’ which compared 6–12 cyclophosphamide pulses and found a lower relapse rate with the longer treatment [20]. However, long-term results showed that early advantage progressively declined and became non-significant by 10 years [21].
The 1-, 5- and 10-year survival rates were comparable between the UK and Turkey cohorts. These rates were not different from previous studies. Five-year survival was over 95% in both groups. We assessed Five-factor score at disease presentation. In multivariate analysis, none of the other characteristics, such as, age, sex, organ involvement, and genetic disease was related to mortality. However, FFS correlated with mortality. Five-year survival was 100% in FFS:0, 96% in FFS:1 and 74.6% in FFS:2. As reported before, the Five-factor score is a useful prognostic tool.
Data about malignancy in PAN patients is limited. There are case reports of PAN as a paraneoplastic phenomenon [22, 23]. Malignancy was observed in 10% of patients and in three, it was the cause of death. Malignancy in vasculitis is better known in ANCA-associated vasculitis mostly seen as urinary tract cancer, leukaemia, and non-melanoma skin cancer; this was explained as a result of impaired immunosurveillance, direct oncogenicity of immunosuppressive agents and perhaps malignant degeneration of tissues undergoing chronic immune stimulation [24].
The strength of conclusions from this study is limited by its retrospective design and sample size. In particular, a consistent approach to genetic testing was not possible. Data collection relied on documentation by the treating physician at the time of clinical evaluation, which was not standardized. No standard treatment protocols were used. The DEI, FFS, VDI scores were calculated from patient records. Even though we compared PAN features, we were not able to evaluate ethnicity.
As a conclusion, these results suggest that the UK and TR cohorts generally had comparable disease characteristics. Certain differences were identified, such as, younger age of disease onset in Turkey; survival and relapse rates were similar. This study also highlights the importance of registries and multicentre collaboration. There is now a need for larger scale genotyping and phenotyping of PAN cohorts to better define subgroups, identify pathogenetic pathways to permit a rational approach to diagnosis and treatment.
References
Kussmaul A, Maier R (1866) Ueber eine bisher nicht beschriebene eigenthu ̈mliche Arterienerkrankung (Periarteritis nodosa), die mit Morbus Brightii und rapid fortschreitender allgemeiner Muskel- l ̈ahmung einhergeht. Dtsch Arch Klin Med 1:484–518
Pagnoux C, Seror R, Henegar C, Mahr A, Cohen P, Le Guern V et al (2010) Clinical features and outcomes in 348 patients with polyarteritis nodosa: a systematic retrospective study of patients diagnosed between 1963 and 2005 and entered into the French Vasculitis Study Group Database. Arthritis Rheum 62(2):616–626
Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F et al (2012) Revised international Chapel Hill consensus conference nomenclature of vasculitides. Arthritis Rheum 65:1–11
Tunca M, Akar S, Onen F, Ozdogan H, Kasapcopur O, Yalcinkaya F et al (2005) Familial Mediterranean Fever (FMF) in Turkey: results of a nationwide multicenter study. Medicine (Baltimore) 84:1–11
Kermani TA, Ham EK, Camilleri MJ, Warrington KJ (2012) Polyarteritis nodosa-like vasculitis in association with minocycline use: a single-center case series. Semin Arthritis Rheum 42:213–221
Navon Elkan P, Pierce SB, Segel R, Walsh T, Barash J, Pedeh S, Zlotogorski A et al (2014) Mutant adenosine deaminase 2 in a polyarteritis nodosa vasculopathy. N Engl J Med 370:921–931
de Menthon M, Mahr A (2011) Treating polyarteritis nodosa: current state of the art. Clin Exp Rheumatol 29(1 Suppl 64):S110–S116
Erden A, Batu ED, Bilgin E, Armagan B, Karadag O, Ozen S et al (2016) Comparing the characteristics of adult and pediatric patients with polyarteritis nodosa. Ann Rheum Dis 75:799
Watts R, Lane S, Scott DG et al (2001) Epidemiology of vasculitis in Europe. Ann Rheum Dis 60(12):1156–1157
Craven A, Robson J, Ponte C, Grayson PC, Suppiah RS, Watts RA et al (2013) ACR/EULAR-endorsed study to develop diagnostic and classification criteria for vasculitis (DCVAS). Clin Exp Nephrol 17:619–621
Watts R, Lane S, Hanslik T, Hauser T, Hellmich B, Koldinsnes W et al (2007) Development and validation of a consensus methodology for the classification of the ANCA-associated vasculitides and polyarteritis nodosa for epidemiological studies. Ann Rheum Dis 66:222–227
De Groot K, Gross WL, Herlyn K, Reinhold-Keller E (2001) Development and validation of a disease extent index for Wegener’s granulomatosis. Clin Nephrol 55:31–38
Guillevin L, Lhote F, Gayraud M, Cohen P, Jarrousse B, Lortholary O et al (1996) Prognostic factors in polyarteritis nodosa and Churg-Strauss syndrome. A prospective study in 342 patients. Medicine (Baltimore) 75:17–28
Exley AR, Bacon PA, Luqmani RA, Kitas GD, Gordon C, Savage CO et al (1997) Development and initial validation of the vasculitis damage index for the standardized clinical assessment of damage in the systemic vasculitides. Arthritis Rheum 40:371–380
Alibaz-Oner F, Koster MJ, Crowson CS, Makol A, Yterberg SR, Salvarani C et al (2017) The clinical spectrum of medium-sized vessel vasculitis. Arthritis Care Res (Hoboken) 69:884–891
Ozen S (2017) The changing face of polyarteritis nodosa and necrotizing vasculitis. Nat Rev Rheumatol 13:381–386
Mahr A, Guillevin L, Poissonnet M, Aymé S (2004) Prevalences of polyarteritis nodosa, microscopic polyangiitis, Wegener’s granulomatosis, and Churg-Strauss syndrome in a French urban multiethnic population in 2000: a capture–recapture estimate. Arthritis Rheum 51:92–99
Guillevin L, Mahr A, Callard P, Godmer P, Pagnoux C, Leray E et al, French Vasculitis Study Group (2005) Hepatitis B virus-associated polyarteritis nodosa: clinical characteristics, outcome, and impact of treatment in 115 patients. Medicine (Baltimore) 84:313–322
Gayraud M, Guillevin L, le Toumelin P, Cohen P, Lhote F, Casassus P et al, French Vasculitis Study Group (2001) Long-term followup of polyarteritis nodosa, microscopic polyangiitis, and Churg-Strauss syndrome: analysis of four prospective trials including 278 patients. Arthritis Rheum 44:666–675
Ribi C, Cohen P, Pagnoux C, Mahr A, Arene JP, Puechal X et al (2010) Treatment of polyarteritis nodosa and microscopic polyangiitis without poor-prognosis factors: a prospective randomized study of one hundred twenty-four patients. Arthritis Rheum 62:1186–1197
Samson M, Puéchal X, Mouthon L, Devilliers H, Cohen P, Bienvenu B et al, French Vasculitis Study Group (FVSG) (2017) Microscopic polyangiitis and non-HBV polyarteritis nodosa with poor-prognosis factors: 10-year results of the prospective CHUSPAN trial. Clin Exp Rheumatol 35(Suppl 103):176–184
Bohn J, Schippers E, Wagner S, Küsters W, Müller J, Meesmann M, Scheppach W (2010) Solitary liver tumor as a manifestation of polyarteritis nodosa. Dtsch Med Wochenschr 135:236–239
Hutterer M, Steurer M, Höffberger R, Heinfelner JA, Pircher A, Nowosielski M et al (2014) Polyarteritis nodosa complicating multiple myeloma—a case report and review of the literature. Clin Neuropathol 33:143–151
Mahr A, Heijl C, Le Guenno G, Faurschou M (2013) ANCA-associated vasculitis and malignancy: current evidence for cause and consequence relationships. Best Pract Res Clin Rheumatol 27:45–56
Author information
Authors and Affiliations
Contributions
OK, AE, YB, SG, AS, BA, İE, SO, DJ Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. OK, AE, YB, SG, AS, BA, İE, SO, DJ Drafting the work or revising it critically for important intellectual content. OK, AE, YB, SG, AS, BA, İE, SO, DJ Final approval of the version to be published. OK, AE, YB, SG, AS, BA, İE, SO, DJ Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Rights and permissions
About this article
Cite this article
Karadag, O., Erden, A., Bilginer, Y. et al. A retrospective study comparing the phenotype and outcomes of patients with polyarteritis nodosa between UK and Turkish cohorts. Rheumatol Int 38, 1833–1840 (2018). https://doi.org/10.1007/s00296-018-4122-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-018-4122-1