Abstract
The objective of the study was to explore the phenotype and intracellular signaling events of B cells in patients with systemic sclerosis (SSc). Peripheral blood B cell surface markers CD19 and CD22 were evaluated by flow cytometry in 23 patients with SSc and seven healthy individuals. Levels of intracellular kinases Lyn, Syk and P-Y 348 Syk along with phosphatase SHP-1 were examined with Western immunoblotting in selected patients. P-Y 822 CD22 was subsequently evaluated flow cytometrically in antigen receptor stimulated B cells. A statistically significant decrease in CD22 B cell surface expression was found in the diffuse subset of patients (median CD22 MFI ± SD was 5.90 ± 2.35 vs 10.20 ± 1.88 for patients vs healthy controls respectively; p = 0.021), while no statistically significant change was found regarding CD19. CD22 underexpression was more pronounced when interstitial lung disease (ILD) was present (median CD22 MFI ± SD was 5.90 ± 2.25 vs 10.20 ± 1.88 for patients with ILD vs healthy controls respectively; p = 0.011). CD22 phosphorylation following B cell receptor (BCR) stimulation was also found to be impaired in patients with diffuse SSc (median change in MFI ± SD was 0.28 ± 0.09 vs 0.38 ± 0.08 for patients vs healthy controls respectively; p = 0.034). Low CD22 expression was arithmetically correlated with kinase Lyn underexpression (Pearson coefficient 0.926; p = ns) in B cells from a small sample of patients. These results suggest that CD22 underexpression and impaired phosphorylation along with implications for Lyn kinase aberrations could contribute to the activated B cell phenotype in SSc.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic sclerosis (SSc) is a multisystem fibrotic connective tissue disease with significant morbidity and mortality among rheumatic diseases. The pathophysiologic process of the disease is considered to rely mainly on immune aberrations, vasculopathy and eventually abnormal fibroblast activation and tissue fibrosis [1]. Knowledge about specific features of autoimmunity and its connection with the final phenotype of fibrosis is at least incomplete, rendering the need for a better understanding of the pathogenesis important.
The role of B cells in autoimmunity is well established. B cells are constantly and thoroughly selected in bone marrow and the periphery in order to eliminate self-reacting clones, by mechanisms such as receptor editing, clonal deletion and anergy. However, a proportion of peripheral B cells escape the check points of the immune system and enhance the susceptibility of the individual with this B cell repertoire to the genesis of autoimmune diseases [2]. B cells have been implicated in SSc mechanisms with a great amount of data derived from both animal models and humans, indicating that B cells play a role in the fibrotic process [3,4,5,6,7]. Patients with SSc exhibit abnormalities of B cell subsets in their peripheral blood, with an expanded naive B cell pool and activated, though diminished due to increased apoptosis, memory B cells [8]. B cell activating factor (BAFF) levels are also increased in the serum of patients, correlating positively with the extent of skin fibrosis [9]. In addition, recent studies have reported that B regulatory cells are reduced and functionally impaired in the peripheral blood of patients with SSc [10, 11]. In vitro experiments using human SSc and healthy B cells and fibroblasts argue for a crosstalk between the two cell types [12,13,14]. On top of the aberrations present in the peripheral blood compartment, B cells actually infiltrate major sites of fibrosis. Microarrays from scleroderma skin show upregulation of endothelial, fibroblast and, perhaps unexpectedly, B cell genes compared to normal skin [15]. Lung biopsies and bronchoalveolar lavage specimens from patients with the disease also exhibit B cell infiltration [16, 17]. Finally, data from genetic studies correlate polymorphisms of genes encoding B cell signaling molecules such as BANK1 and BLK with SSc [18, 19].
CD19 and CD22 are important surface molecules of the B cell participating in a loop that fine tunes the threshold of antigen receptor stimulation. Disruption in these molecules has been implicated in autoimmunity and autoantibody production [20]. CD19 exerts a positive effect in B cell signaling and patients with SSc are reported to overexpress it [10, 21]. CD22 on the other hand, which is the major focus of this study, is a negative regulator of B cell signaling thresholds. It belongs to the family of sialic-acid-binding immunoglobulin-type lectins (Siglecs) and is found exclusively on the surface of B cells. Both extracellular ligand-binding and intracellular signaling domains of the molecule have been implicated in its inhibitory function with distinct mechanisms [22]. The extracellular domain is currently considered to bind sialic acids contributing to the association of CD22 with the BCR complex but also the recognition of peptides in the external environment of the cell. Self-antigens are usually highly sialylated and this can differentiate them from foreign pathogens. Apart from the obvious role of this ligand-binding function in the fight against infection, it is also thought to recognize weakly affiliated self-antigens and maintain autoimmune clones of mature B cells in a state of clonal ignorance. Kinase Lyn as well as target molecules of Lyn, such as kinase Syk and the cytoplasmic domain of CD22, are critical molecules in the early signaling events following antigen receptor stimulation [23]. Lyn is recruited rapidly after BCR engagement and is indispensable regarding CD22 activation [24]. Phosphatase SHP-1 is the major enzyme activated by the phosphorylated CD22 [23]. The phosphorylation of immunoreceptor tyrosine-based inhibitory motifs (ITIMs) in the intracellular tail of CD22 is a crucial step in the Lyn/CD22/SHP-1 inhibitory pathway. The dampening of the B cell signaling by this pathway is a developmental stage in B cell maturation offering a critical inhibitory mechanism promoting B cell tolerance [25]. One can assume that CD22, which is expressed mostly in mature B cells, is of special importance in the mechanisms of tolerance in the periphery, for those clones that have escaped the initial strict check points in B cell maturation.
This study focuses on the B cell in SSc. Primary aim of the study was to offer insight regarding the phenotype and the early signaling events of the B cell in patients with the disease. In addition, functional aspects of the CD22 molecule were investigated. Research of the B cell intracellular signaling events adds to the novelty of this effort.
Materials and methods
Patients and healthy donors
Peripheral blood was obtained from 15 patients with diffuse systemic sclerosis (dSSc), eight patients with limited systemic sclerosis (lSSc) and seven healthy donors. We used all samples for flow cytometry. Samples from this cohort (cohort 1) with adequate cell numbers for protein extraction were used for B cell intracellular molecule evaluation. At a later time point, new samples were obtained from a new cohort of nine patients with dSSc (cohort 2) and six age- and sex-matched healthy donors for the CD22 phosphorylation experiments. All patients fulfilled the ACR/EULAR criteria for SSc diagnosis [26]. The procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. A local (Patras University Hospital) ethics committee approved the study protocol. Written informed consent was obtained from all individual participants included in the study.
Cells
Peripheral blood mononuclear cells (PBMCs) were isolated from heparinized blood using Ficoll gradient centrifugation (Biochrom GmbH, Berlin). B cells were negatively selected with magnetic isolation from PBMCs by depletion of non-B cells using the human B cell isolation kit II (Miltenyi Biotec, Auburn, CA) as described elsewhere [27]. Percentages of B cells, determined by flow cytometry, were > 95% including samples used in Western immunoblotting.
Reagents and antibodies
Fluorochrome-conjugated monoclonal antibodies (mAb) anti-CD19-FITC and anti-CD22-PE/Cy5 were from Bio Legend, San Diego, CA. Rabbit polyclonal anti-human Lyn, mouse monoclonal anti-human Syk, goat polyclonal HRP-conjugated anti-human SHP-1, rabbit polyclonal HRP-conjugated anti-human GAPDH, as well as the secondary HRP-conjugated antibodies goat anti-rabbit IgG and goat anti-mouse IgG were all from Santa Cruz Biotechnology, Inc. (Santa Cruz, CA). The antibody against the phosphorylated form of Syk at the 348 tyrosine site and the PE-conjugated antibody against the phosphorylated form of CD22 at the 822 tyrosine site were both from Becton–Dickinson Biosciences, San Diego, CA. B cells were stimulated with the F(ab′)2 fragment of an affinity purified goat anti-human µ heavy chain antibody (IgM Fc5µ) (Jackson Immunoresearch Laboratories Inc). B cells were permeabilized and fixed with BD Phosflow™ Perm buffer III (1X) and BD Phosflow™ Lyse/Fix buffer (5X) from Beckton Dickinson Biosciences, San Diego, CA.
Flow cytometry
PBMCs (0.5 × 106) enriched in B cells by magnetic isolation were used for the surface expression study of CD19 and CD22. Samples were incubated on ice with saturating concentrations of fluorochrome-conjugated mAb or their respective isotypic-control mAb for 1 h.
PBMCs (1 × 106) were used for the intracellular phosphorylation study of CD22. Cells first stained for surface CD19 to define the B cell population were then permeabilised and fixed. Briefly, human PBMCs were either stimulated by cross-linking of BCR with the F(ab′)2 fragment of an affinity purified goat anti-human µ heavy chain antibody at 37 °C for 6 min or unstimulated. The cells were fixed with pre-warmed BD Phosflow™ Lyse/Fix Buffer for 10 min at 37 °C, permeabilized with BD Phosflow™ Perm Buffer III on ice for at least 30 min, and then stained with PE Mouse anti-CD22 (pY822) mAb at saturating concentrations for 1 h.
All samples were analyzed on a Beckman Coulter Cytomics FC 500 cytometer.
Western immunoblotting
Samples highly enriched in B cells (> 95%) were lysed as resting cells. Proteins (7 µg per lane) were separated in 10% SDS-polyacrylamide gels and transferred to nitrocellulose membranes (Sigma-Aldrich, Inc.) using a semi-dry transfer system. Membranes were incubated overnight at 4 °C with the appropriate antibody in blocking solution and then washed and incubated with the appropriate HRP-conjugated secondary antibody when needed for 2 h at room temperature. Detection of bands was performed with the ECL Plus detection system (Amersham, Buckinghamshire, UK) on Kodak X-Omat LS films (Eastman Kodak, Rochester, NY). Densitometric analysis was performed using ImageJ software and results are expressed as densitometric ratios of Lyn, Syk, P-Y 348 Syk or SHP-1 density over GAPDH.
Statistical analysis
Statistical analysis was performed with IBM SPSS Statistics 24 software. The normality of data was tested with the Kolmogorov–Smirnov and Shapiro–Wilk tests. The Mann–Whitney U and Pearson tests were used for data analysis. Values of p ≤ 0.05 were considered to be statistically significant.
Results
Decreased expression of surface CD22 in resting peripheral B cells in patients with dSSc
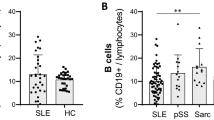
PBMCs enriched in B cells from 15 patients with diffuse disease, eight patients with limited disease and seven healthy individuals were phenotypically analyzed by flow cytometry. The clinical characteristics, demographic data, serologic profile and current treatment of these patients (cohort 1) are summarized in Table 1. The two molecules examined were CD19 and CD22 and mean fluorescence intensity (MFI) was used as a measure of their surface expression. B cell expression of CD22 was significantly decreased in patients with diffuse SSc, but not in those with the limited form of the disease, compared to healthy donors. More specifically, the median (min; max) CD22 MFI ± SD was 5.90 (2.91; 10.70) ± 2.35 vs 10.20 (6.38; 11) ± 1.88 for patients with dSSc vs healthy controls respectively (p = 0.021), while it was 9.11 (4.78; 11.9) ± 2.67 for patients with lSSc (p = ns and p < 0.05 when compared with healthy controls and patients with dSSc respectively). B cell surface CD19 expression did not differ significantly between the three groups in our cohort. Median (min; max) CD19 MFI ± SD was 8.10 (4.78; 11.2) ± 1.58 vs 9.19 (8.09; 13.4) ± 1.67 vs 9.11 (7.27; 11.8) ± 1.41 for patients with dSSc vs patients with lSSc vs healthy controls (p = ns for either SSc subtype vs healthy controls). A representative comparison experiment from the samples of one healthy donor and one patient with diffuse disease along with collective data is depicted in Fig. 1. The experiments presented provide, therefore, evidence that B cell surface expression of the signaling inhibitory molecule CD22 is decreased in patients with dSSc compared to healthy individuals.
Flow cytometry data depicting decreased CD22 surface expression in SSc. a Flow cytometry images depicting a patient vs a healthy donor sample. Both samples are highly enriched in B cells. The overlay histogram depicts significant difference in CD22 surface expression between the two samples. b Boxplot graph depicting surface CD22 expression in healthy controls and patients with diffuse disease. CD22 expression is significantly lower in patients with the diffuse subset of SSc. c Boxplot graph depicting the significantly lower CD22 surface expression in patients with interstitial lung disease (ILD) versus healthy controls
Decreased expression of B cell surface CD22 in the subset of patients with interstitial lung disease
To address the question whether decreased B cell surface CD22 expression was correlated with disease activity, a separate analysis of patients with dSSc and concomitant ILD was chosen, because reliable scoring systems for disease activity in patients with dSSc are currently lacking. Such analysis of patients with severe dSSc as evidenced by the presence of ILD (manifested by the presence of ground glass, reticular or honeycombing lesions in high resolution computed chest tomography) was, therefore, performed. Median (min; max) FVC ± SD and median (min; max) DLCO ± SD was 92 (58; 110) ± 16.3 and 72.5 (25; 100) ± 20.2, respectively, for this subgroup of patients, which consisted of 11 patients. Patients with dSSc and ILD were found to have significantly lower CD22 expression in our cohort indicating that severe disease correlated with an even greater decrease in the expression of this critical B cell molecule. Median (min; max) CD22 MFI ± SD was 5.90 (2.91; 9.63) ± 2.25 vs 10.20 (6.38; 11) ± 1.88 for patients with ILD vs healthy controls respectively (p = 0.011). Median (min; max) CD22 MFI ± SD was 8.96 (4.48; 11.9) ± 2.69 for all patients without evidence of lung involvement. The comparison of the latter with healthy controls did not reveal statistically significant difference while it tended but did not reach statistical significance (p = 0.057) when compared to patients with ILD. Data are depicted in Fig. 1c.
Lyn protein underexpression in a proportion of patients with low surface CD22 expression
Samples highly enriched in B cells (> 95%) from three patients with dSSc, two patients with lSSc and two healthy donors were lysed and the protein extracted was used in Western immunoblotting. Protein expression of major kinases such as Lyn, Syk and P-Y 348 Syk as well as the phosphatase SHP-1 was examined in resting B cells. Median (min; max) Lyn/GAPDH ratio ± SD was 0.54 (0.33; 2.02) ± 0.92 vs 1.57 (1.36; 1.78) ± 0.29 vs 1.52 (1.10; 1.94) ± 0.58 for patients with dSSc vs patients with lSSc vs healthy controls, respectively. Median (min; max) Syk/GAPDH ratio ± SD was 0.90 (0.52; 1.05) ± 0.27 vs 1.12 (1.09; 1.16) ± 0.05 vs 1.49 (1.30; 1.68) ± 0.26 for dSSc vs lSSc vs healthy controls respectively. Median (min; max) P-Y 348 Syk/GAPDH ratio ± SD was 0.14 (0.09; 0.32) ± 0.12 vs 0.31 (0.19; 0.43) ± 0.17 vs 0.15 (0.12; 0.18) ± 0.04 for dSSc vs lSSc vs healthy controls respectively. Mean SHP-1/GAPDH ratio ± SD was 0.15 (0.13; 0.18) ± 0.02 vs 0.20 (0.16; 0.24) ± 0.05 vs 0.15 (0.14; 0.17) ± 0.02 for dSSc vs lSSc vs healthy controls respectively. No significant differences were found in all comparisons. Two out of the three patients with dSSc studied showed decreased CD22 surface expression in our initial flow cytometry experiments. For these two patients, an even greater arithmetic difference was clear for Lyn/GAPDH ratio compared to healthy controls [median (min; max) Lyn/GAPDH ratio ± SD was 0.43 (0.33; 0.54) ± 0.14 vs 1.52 (1.10; 1.94) ± 0.58, respectively]. Pearson correlation coefficient was 0.926 for the two variables of CD22 surface expression and Lyn/GAPDH ratio (p = ns). We propose that the aberrant CD19/CD22 loop could correlate with kinase Lyn decreased expression in some patients with the disease, even though a larger sample of patients is warranted for more clear conclusions. A representative Western blot experiment and clustered bars depicting surface CD22 MFI along with Lyn protein expression are shown in Fig. 2.
Lyn protein expression and correlation with CD22 in SSc. a Paired Western blot films depicting Lyn protein and GAPDH control protein expression in three patients with diffuse SSc (dSSc), two patients with limited SSc (lSSc) and two healthy controls (Cnt). b Paired bars depicting Lyn densitometric ratio along with surface CD22 expression for each one of the presented cases
Impaired CD22 Y 822 phosphorylation following BCR stimulation in patients with dSSc
Based on our initial findings of the significant CD22 underexpression and also on the tendency of Lyn underexpression in patients with dSSc, we evaluated whether there is any functional impairment of the CD22 molecule in the diffuse form of the disease. Phosphorylation of CD22 before and after BCR stimulation was studied in B cells from nine patients with dSSc and six healthy donors. Demographic data, clinical characteristics and treatment of this cohort of patients (cohort 2) are presented in Table 1. Lyn is currently thought to be the major kinase to phosphorylate tyrosine residues lying into ITIMs in the CD22 intracellular component [24]. The 822 tyrosine residue found in one of the ITIMs of CD22 was evaluated, the phosphorylation of which provides docking site for SHP-1 activation. SHP-1 is a tyrosine phosphatase that upon activation subsequently negatively regulates the signaling cascade [28].
Time-response flow cytometry experiments were first conducted in order to determine the kinetics of CD22 Y 822 phosphorylation following BCR activation. Maximum phosphorylation was found to be achieved at 6 min following activation. Our goal was to compare the change in Y 822 phosphorylation, which comes as an effect of BCR stimulation, between patients with dSSc and healthy donors. To achieve this, phosphorylation values at each time point (baseline and 6 min post activation) were measured and then subtracted. Rather than using the MFI of the B cell population alone (CD19+ cells) as the phosphorylation value mentioned earlier, we chose to calculate the ratio of MFI (MFI r ) of the B cell population to that of the non-B cell population as an own control. This way a possible nonspecific fluorescence effect of the BCR stimulating antibody used was corrected. The median (min; max) change in phosphorylation (ΔMFIr) ± SD was 0.28 (0.13; 0.41) ± 0.09 vs 0.38 (0.32; 0.49) ± 0.08 for patients with dSSc vs healthy controls respectively (p = 0.034), thus depicting a significantly decreased Y 822 phosphorylation of CD22. Representative experiments of one healthy donor and one patient as well as the cumulative data are depicted in Fig. 3. B cell signaling regulator molecule CD22 was not only found reduced regarding its surface expression in a proportion of patients with dSSc but its inhibitory function, reflected by the phosphorylation of Y 822, was also decreased. This may, at least in part, explain the previously reported activated phenotype of the B cell in SSc.
Flow cytometry data depicting impaired CD22 phosphorylation in SSc. a Flow cytometry images of a healthy control sample. The phosphorylation of CD22 at the 822 tyrosine site in CD19-positive cells before and after B cell receptor stimulation was studied. The overlay histogram reveals the change in phosphorylation after stimulation. b Similar images as in a regarding a patient sample. The overlay histogram portrays the impaired phosphorylation of CD22 after B cell receptor stimulation. c Box plot graph depicting the statistically significant difference in CD22 phosphorylation after B cell receptor activation between healthy controls and patients with dSSc
Discussion
B cell’s deranged phenotype in the diffuse subset of systemic sclerosis is correlated with low surface expression and functional aberrations of the molecule CD22 in this study. This was more evident in active disease, as depicted by the presence of ILD. Decreased CD22 surface expression was correlated with low Lyn expression, albeit not in a statistically significant manner due to the small number of patients. Impaired phosphorylation of CD22 was found following BCR stimulation in diffuse disease. These data hopefully offer new insight regarding the role of B cell and the molecule CD22 in the pathogenesis of systemic sclerosis.
Findings from the previous studies showcase the importance of an aberrant CD22 expression and function. In animal models, deficient CD22 expression was reported to lead to autoantibody production in CD22 knockout mice. Ca++ flux was increased upon BCR ligation and high affinity IgG anti ds-DNA antibodies were evident in aging mice although they did not proceed to develop autoimmune disease [29]. In tight-skin mice, a genetic model of SSc, the constitutive as well as the BCR engagement induced CD22 tyrosine phosphorylation was significantly lower compared to wild type B cells [4]. Regarding systemic sclerosis in humans, CD22 underexpression was previously reported. This finding was evident in patients with peripheral vascular alterations, as expressed by the modified Medsger score [30]. Also, previous studies reported impaired CD22 function, attributed either to genetic polymorphisms of the molecule in a cohort of patients with lSSc [31] or the presence of anti CD22 antibodies in a mixed cohort of patients with both diffuse and limited SSc. The anti-CD22 antibodies were correlated with the diffuse subset of the disease (numerically higher titers) and increased disease activity while they were also found to be functionally active as they diminished the tyrosine phosphorylation of the cytoplasmic tail of CD22 [32]. The decreased CD22 expression found in this study could be partly responsible for the survival of autoreactive clones of B cells facilitating the disease pathogenesis and evolution. This could be mediated by either increased BCR signaling or defective silencing by the ligand binding function of CD22. However, other studies in the past did not show statistically important differences regarding the molecule expression [21]. It is also noteworthy that this cohort failed to verify the previously reported increased CD19 expression [10, 21]. Perhaps the density of these molecules on the cell membrane is a characteristic that fluctuates according to different factors such as the disease activity and the cytokine milieu affecting the cell.
Interestingly, this study’s attempt to investigate kinases and phosphatases of B cell early signaling cascade with Western immunoblotting showed that two patients with dSSc who exhibited significantly low CD22 expression appeared to also have numerically low Lyn expression. This suggests that in some patients there appears to be an immunological aberration that may correlate both low CD22 and low Lyn expression in the Lyn/CD22/SHP-1 inhibitory pathway. The small number of patients studied is definitely a disadvantage and can only set these data as an observation that warrants more patients and well-designed experiments in order to be verified. The finding of reduced CD22 and Lyn expression in this cohort as well as the reports of functional aberrations of this inhibitory molecule was the trigger for us to further explore its functional behavior after BCR stimulation in the disease of SSc. As mentioned earlier, Lyn is considered to be indispensable regarding the phosphorylation of CD22 cytoplasmic domain after BCR activation [24]. These data indeed suggest that CD22 inhibitory function is impaired in B cells after the stimulation of their immunoglobulin receptor. This has not been reported to our knowledge until now. The impaired CD22 Y 822 phosphorylation presented in this paper cannot be directly correlated with the low CD22 or/and Lyn expression; however, it is a finding that verifies the deranged B cell phenotype at least in patients with active diffuse disease.
These data depict aspects of the immunological aberrations present in patients with SSc. However, some of these aberrations could be common between autoimmune diseases rather than disease specific. Lyn underexpression had been previously reported in systemic lupus erythematosus patients [33]. In addition, unpublished data regarding lupus patients in our lab show an even more impaired CD22 phosphorylation after BCR activation. B cell is an important player in the pathogenesis of autoimmune diseases and systemic sclerosis in particular. Efficient therapeutic interventions for this orphan disease are limited, and new treatment targets could offer new hope. Epratuzumab, a CD22-targeted monoclonal antibody with nondepleting but rather immune adjusting function, is under research as a possible treatment in hematologic malignancies and autoimmune diseases. Despite its early encouraging results in lupus, the phase III trials failed to verify significant results in patients with this autoimmune disease [34]. The immunomodulating role of epratuzumab is not clear but there are data showing that it can enhance phosphorylation of CD22 ITIMs and attenuate BCR and Toll-like receptor induced signaling [35,36,37]. Moreover, several studies have already shown promising, still preliminary, results assessing the efficacy of B cell depletion with rituximab, a chimeric monoclonal antibody against the CD20 antigen, in the treatment of SSc associated ILD and skin fibrosis [38,39,40,41,42,43,44,45]. Better understanding of the altered procedures in B cell delicate fine tuning could help in the disease management and perhaps even showcase new immune modulating biologic therapies or the targeting of small molecules as potentially helpful treatment interventions in the future.
References
Varga J, Abraham D (2007) Systemic sclerosis: a prototypic multisystem fibrotic disorder. J Clin Invest 117:557–567
Pillai S, Mattoo H, Cariappa A (2011) B cells and autoimmunity. Curr Opin Immunol 23:721–731
Saito E, Fujimoto M, Hasegawa M, Komura K, Hamaguchi Y, Kaburagi Y et al (2002) CD19-dependent B lymphocyte signaling thresholds influence skin fibrosis and autoimmunity in the tight-skin mouse. J Clin Invest 109:1453–1462
Asano N, Fujimoto M, Yazawa N, Shirasawa S, Hasegawa M, Okochi H et al (2004) B Lymphocyte signaling established by the CD19/CD22 loop regulates autoimmunity in the tight-skin mouse. Am J Pathol 165:641–650
Yoshizaki A, Iwata Y, Komura K, Ogawa F, Hara T, Muroi E et al (2008) CD19 regulates skin and lung fibrosis via toll-like receptor signaling in a model of bleomycin-induced scleroderma. Am J Pathol 172:1650–1663
Komura K, Yanaba K, Horikawa M, Ogawa F, Fujimoto M, Tedder TF et al (2008) CD19 regulates the development of bleomycin-induced pulmonary fibrosis in a mouse model. Arthritis Rheum 58:3574–3584
Yoshizaki A, Sato S (2015) Abnormal B lymphocyte activation and function in systemic sclerosis. Ann Dermatol 27:1
Sato S, Fujimoto M, Hasegawa M, Takehara K (2004) Altered blood B lymphocyte homeostasis in systemic sclerosis: expanded naive B cells and diminished but activated memory B cells. Arthritis Rheum 50:1918–1927
Matsushita T, Hasegawa M, Yanaba K, Kodera M, Takehara K, Sato S (2006) Elevated serum BAFF levels in patients with systemic sclerosis: enhanced BAFF signaling in systemic sclerosis B lymphocytes. Arthritis Rheum 54:192–201
Mavropoulos A, Simopoulou T, Varna A, Liaskos C, Katsiari CG, Bogdanos DP et al (2016) Breg cells are numerically decreased and functionally impaired in patients with systemic sclerosis. Arthritis Rheumatol 68:494–504
Matsushita T, Hamaguchi Y, Hasegawa M, Takehara K, Fujimoto M (2016) Decreased levels of regulatory B cells in patients with systemic sclerosis: association with autoantibody production and disease activity. Rheumatology 55:263–267
François A, Chatelus E, Wachsmann D, Sibilia J, Bahram S, Alsaleh G et al (2013) B lymphocytes and B-cell activating factor promote collagen and profibrotic markers expression by dermal fibroblasts in systemic sclerosis. Arthritis Res Ther 15:R168
Daoussis D, Liossis S-NC (2013) B cells tell scleroderma fibroblasts to produce collagen. Arthritis Res Ther 15:125
Dumoitier N, Chaigne B, Régent A, Lofek S, Mhibik M, Dorfmüller P et al (2017) Scleroderma peripheral B lymphocytes secrete interleukin-6 and transforming growth factor β and activate fibroblasts. Arthritis Rheumatol 69:1078–1089
Whitfield ML, Finlay DR, Murray JI, Troyanskaya OG, Chi J-T, Pergamenschikov A et al (2003) Systemic and cell type-specific gene expression patterns in scleroderma skin. Proc Natl Acad Sci USA 100:12319–12324
Lafyatis R, O’Hara C, Feghali-Bostwick CA, Matteson E (2007) B cell infiltration in systemic sclerosis-associated interstitial lung disease. Arthritis Rheum 56:3167–3168
De Santis M, Bosello SL, Peluso G, Pinnelli M, Alivernini S, Zizzo G et al (2012) Bronchoalveolar lavage fluid and progression of scleroderma interstitial lung disease. Clin Respir J 6:9–17
Rueda B, Gourh P, Broen J, Agarwal SK, Simeon C, Ortego-Centeno N et al (2010) BANK1 functional variants are associated with susceptibility to diffuse systemic sclerosis in Caucasians. Ann Rheum Dis 69:700–705
Ito I, Kawaguchi Y, Kawasaki A, Hasegawa M, Ohashi J, Kawamoto M et al (2010) Association of the FAM167A-BLK region with systemic sclerosis. Arthritis Rheum 62:890–895
Tedder TF, Sato S, Poe JC, Fujimoto M (2000) CD19 and CD22 regulate a B lymphocyte signal transduction pathway that contributes to autoimmunity. Keio J Med 49:1–13
Sato S, Hasegawa M, Fujimoto M, Tedder TF, Takehara K (2000) Quantitative genetic variation in CD19 expression correlates with autoimmunity. J Immunol 165:6635–6643
Müller J, Nitschke L (2014) The role of CD22 and Siglec-G in B-cell tolerance and autoimmune disease. Nat Rev Rheumatol 10:422–428
Dal Porto JM, Gauld SB, Merrell KT, Mills D, Pugh-Bernard AE, Cambier J (2004) B cell antigen receptor signaling 101. Mol Immunol 41:599–613
Smith KG, Tarlinton DM, Doody GM, Hibbs ML, Fearon DT (1998) Inhibition of the B cell by CD22: a requirement for Lyn. J Exp Med 187:807–811
Gross AJ, Lyandres JR, Panigrahi AK, Prak ETL, DeFranco AL (2009) Developmental acquisition of the Lyn-CD22-SHP-1 inhibitory pathway promotes B cell tolerance. J Immunol 182:5382–5392
Van den Hoogen F, Khanna D, Fransen J, Johnson SR, Baron M, Tyndall A et al (2013) 2013 classification criteria for systemic sclerosis: an American College of Rheumatology/European League Against Rheumatism Collaborative Initiative: ACR/EULAR classification criteria for SSc. Arthritis Rheum 65:2737–2747
Karampetsou MP, Andonopoulos AP, Liossis S-NC (2011) Treatment with TNFα blockers induces phenotypical and functional aberrations in peripheral B cells. Clin Immunol 140:8–17
Doody GM, Justement LB, Delibrias CC, Matthews RJ, Lin J, Thomas ML et al (1995) A role in B cell activation for CD22 and the protein tyrosine phosphatase SHP. Science 269:242–244
O’Keefe TL, Williams GT, Batista FD, Neuberger MS (1999) Deficiency in CD22, a B cell-specific inhibitory receptor, is sufficient to predispose to development of high affinity autoantibodies. J Exp Med 189:1307–1313
Soto L, Ferrier A, Aravena O, Fonseca E, Berendsen J, Biere A et al (2015) Systemic sclerosis patients present alterations in the expression of molecules involved in B-cell regulation. Front Immunol 6:496
Hitomi Y, Tsuchiya N, Hasegawa M, Fujimoto M, Takehara K, Tokunaga K et al (2007) Association of CD22 gene polymorphism with susceptibility to limited cutaneous systemic sclerosis. Tissue Antigens 69:242–249
Odaka M, Hasegawa M, Hamaguchi Y, Ishiura N, Kumada S, Matsushita T et al (2010) Autoantibody-mediated regulation of B cell responses by functional anti-CD22 autoantibodies in patients with systemic sclerosis. Clin Exp Immunol 159:176–184
Liossis SN, Solomou EE, Dimopoulos MA, Panayiotidis P, Mavrikakis MM, Sfikakis PP (2001) B-cell kinase lyn deficiency in patients with systemic lupus erythematosus. J Investig Med 49:157–165
Clowse MEB, Wallace DJ, Furie RA, Petri MA, Pike MC, Leszczyński P et al (2017) Efficacy and safety of epratuzumab in moderately to severely active systemic lupus erythematosus: results from two phase III randomized, double-blind, placebo-controlled trials. Arthritis Rheumatol 69:362–375
Lumb S, Fleischer SJ, Wiedemann A, Daridon C, Maloney A, Shock A et al (2016) Engagement of CD22 on B cells with the monoclonal antibody epratuzumab stimulates the phosphorylation of upstream inhibitory signals of the B cell receptor. J Cell Commun Signal 10:143–151
Sieger N, Fleischer SJ, Mei HE, Reiter K, Shock A, Burmester GR et al (2013) CD22 ligation inhibits downstream B cell receptor signaling and Ca(2+) flux upon activation. Arthritis Rheum 65:770–779
Giltiay NV, Shu GL, Shock A, Clark EA (2017) Targeting CD22 with the monoclonal antibody epratuzumab modulates human B-cell maturation and cytokine production in response to toll-like receptor 7 (TLR7) and B-cell receptor (BCR) signaling. Arthritis Res Ther 19:91
McGonagle D, Tan AL, Madden J, Rawstron AC, Rehman A, Emery P et al (2008) Successful treatment of resistant scleroderma-associated interstitial lung disease with rituximab. Rheumatology 47:552–553
Lafyatis R, Kissin E, York M, Farina G, Viger K, Fritzler MJ et al (2009) B cell depletion with rituximab in patients with diffuse cutaneous systemic sclerosis. Arthritis Rheum 60:578–583
Daoussis D, Liossis S-NC, Tsamandas AC, Kalogeropoulou C, Kazantzi A, Sirinian C et al (2010) Experience with rituximab in scleroderma: results from a 1-year, proof-of-principle study. Rheumatology 49:271–280
Bosello S, De Santis M, Lama G, Spanò C, Angelucci C, Tolusso B et al (2010) B cell depletion in diffuse progressive systemic sclerosis: safety, skin score modification and IL-6 modulation in an up to thirty-six months follow-up open-label trial. Arthritis Res Ther 12:R54
Smith V, Van Praet JT, Vandooren B, Van der Cruyssen B, Naeyaert JM, Decuman S et al (2010) Rituximab in diffuse cutaneous systemic sclerosis: an open-label clinical and histopathological study. Ann Rheum Dis 69:193–197
Keir GJ, Maher TM, Ming D, Abdullah R, de Lauretis A, Wickremasinghe M et al (2014) Rituximab in severe, treatment-refractory interstitial lung disease. Respirology 19:353–359
Jordan S, Distler JHW, Maurer B, Huscher D, Laar JM van, Allanore Y et al (2015) Effects and safety of rituximab in systemic sclerosis: an analysis from the European Scleroderma Trial and Research (EUSTAR) group. Ann Rheum Dis 74:1188–1194
Daoussis D, Melissaropoulos K, Sakellaropoulos G, Antonopoulos I, Markatseli TE, Simopoulou T et al (2017) A multicenter, open-label, comparative study of B-cell depletion therapy with rituximab for systemic sclerosis-associated interstitial lung disease. Semin Arthritis Rheum 46:625–631
Acknowledgements
We would like to thank all study participants. We would also like to thank Eugenia Verigou, MD, for her valuable contribution regarding the flow cytometry experiments and figures.
Funding
This work was supported by the University of Patras through the “Karathodori” research grant and the Hellenic Rheumatology Society through a scholarship.
Author information
Authors and Affiliations
Contributions
KM designed the study, performed patient recruitment, performed flow cytometry and western immunoblotting experiments, analyzed the data and drafted the manuscript. SNL conceived the study concept, designed the study, participated in patient recruitment, data analysis and manuscript drafting and revision. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Melissaropoulos, K., Liossis, SN. Decreased CD22 expression and intracellular signaling aberrations in B cells of patients with systemic sclerosis. Rheumatol Int 38, 1225–1234 (2018). https://doi.org/10.1007/s00296-018-4076-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-018-4076-3