Abstract
Chronic recurrent multifocal osteomyelitis (CRMO) is a rare non-infectious inflammatory disorder with unpredictable clinical course, characterized by acute exacerbations and spontaneous remissions. There are no randomized-controlled trials about treatment options. Non-steroidal anti-inflammatory drugs (NSAID) are the first-line treatment option; glucocorticoids seem to be effective; positive outcomes have been obtained with bisphosphonates. In the last few years successful use of biologic agents like anti-TNF agents has been reported. We report the cases of 3 children suffering from CRMO who were treated with NSAID, steroid, bisphosphonates and eventually received etanercept and 1 case without vertebral involvement treated with etanercept after NSAID and steroid; all cases showed clinical improvement. The mean ages at symptoms onset and diagnosis were 8 and 10 years and 10 months, respectively. Two patients presented with back pain and three had vertebral lesions. Mean interval from diagnosis to the onset of anti-TNF treatment was 14 months. According to our small experience, we suggest considering therapy with etanercept for the treatment of severe cases with persistently active disease despite multiple treatments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic recurrent multifocal osteomyelitis (CRMO) is a rare non-infectious inflammatory disorder with unclear aetiology [1]. Symptoms of presentation may range from mild unspecific bone pain, local swelling and warmth to severe pain, malaise, fevers and even fractures. Clinical course is unpredictable and characterized by acute exacerbations and spontaneous remissions [2]. CRMO is part of a large group of conditions grouped under the name of non-bacterial osteomyelitis, whose diagnostic criteria have been recently formulated [3]. However, an accurate diagnosis is challenging because clinical findings, laboratory tests and radiography are often unspecific and CRMO remains a diagnosis of exclusion [4]. CRMO is associated with pathologic conditions such as psoriasis, palmoplantar pustulosis, Sweet’s syndrome, Takayasu’s arteritis, Wegener’s granulomatosis, spondyloarthropathy, pyoderma gangrenosum and inflammatory bowel diseases [5].
There are no randomized-controlled trials about treatment options. Non-steroidal anti-inflammatory drugs (NSAID) are the first-line treatment option; glucocorticoids seems to be effective at doses of 1–2 mg/kg a day with progressive tapering off [6]; positive outcomes have been obtained with bisphosphonates [7]. There are a number of reports for successful use of biologic agents like tumour necrosis factor (TNF)-α inhibitors [8,9,10,11].
We report the cases of three children suffering from CRMO who were treated with NSAID, steroid, bisphosphonates and eventually received etanercept and 1 case without vertebral involvement treated with etanercept after NSAID and steroid, all cases showed clinical improvement.
Case presentation
Case 1
CM is a 9-year-old male child who started to limp complaining of pain in his right hip and left buttock from January 2014. He underwent hip and pelvic X-ray which excluded a traumatic event. At that time laboratory tests showed mild alteration of inflammatory indexes [C-reactive protein (CRP) = 2.38 mg/dL; normal value < 0.8 mg/dL] and throat swab was positive for streptococcal infection. Physical examination showed a painful limitation in active and passive movements of the hips. Ultrasonography revealed a bilateral coxitis with mild swelling and subsequent pelvic magnetic resonance imaging (MRI) confirmed a mild bilateral arthrosynovitis. Medical history, laboratory tests and imaging results focused our attention on a reactive arthritis. Antibiotic and anti-inflammatory therapies failed to improve the painful limping and importantly, fatigue. The pain then migrated to the gluteal region during the following weeks and it was treated with NSAID. At the same time, blood inflammatory markers slightly improved [erythrocyte sedimentation rate (ESR) dropped from 80 to 43 mm] while painful symptoms were inconstant. Interferon gamma release assay (IGRA) test was negative. The child then complained occasionally thoracic and scapular pain and physical examination showed a mild scoliosis and kyphosis. Therefore, we performed vertebral plain X-ray which revealed a densification in the first thoracic vertebra (T1), a partial collapse with an expansion of the disc space. A similar alteration was present in C6–C7 too. An MRI of the spine was performed showing diffuse signal alterations (hypointensity on T1 sequences, hyperintensity on T2 and STIR, high contrast enhancement) in several vertebral bodies: in T1 with depression of superior endplate, more subtle in T6, T7, T8, T10 and T11; similar aspects were also present in the left sacroiliac joint and less in the right one.
Suspecting CRMO, a whole-body MRI (wbMRI) was performed which confirmed the vertebral column involvement and revealed areas of altered signal in the right acetabulum, in the acromion of the left scapula, in the right medial malleolus and in the left lateral one too. To exclude a malignant origin of the lesions the child was subjected to a bone biopsy in the left iliac wing that showed unspecific fibrosis and chronic inflammatory changes without any evidence of Langerhans cell histiocytosis or suppurative infection.
Since the child had been treated for a long time with NSAID with only partial relief, steroid therapy (prednisone 1 mg/kg) was started with initial improvement [Fig. 1].
Patient 1: pelvic and spinal MRI before and after steroid therapy. a Coronal STIR image: hyperintensity of the iliac wings, in particular in the left acetabular seating. Vertebral sagittal T2-weighted image (b) and sagittal T1-weighted fat-suppressed gadolinium-enhanced image (c) showing diffuse hyperintensity in several vertebral bodies: in T1 with depression of superior endplate, more subtle in T6, T7, T8, T10 and T11. d Coronal T1-weighted fat-suppressed gadolinium-enhanced image showing improvement of signal alteration of the iliac wings after steroid therapy. Sagittal cervico-dorsal (e) and dorso-lumbar (f) T1-weighted fat-suppressed gadolinium-enhanced images showing improvement with the resolution of the signal alteration previously described in the vertebrae
The following month the child experienced a clinical relapse and inflammatory aspects in the left sacroiliac joint with pathological contrast enhancement at MRI were found. For the persistence of symptoms despite steroid therapy and continuous disease activity at imaging evaluation, treatment with bisphosphonates (intravenous pamidronate) was started. The child underwent three cycles of infusions over three consecutive days with initial improvement. However, for the persistence of backache and worsening of vertebral lesions at MRI evaluation biologic treatment with etanercept was started. Clinical remission was achieved and the imaging evaluation 3 and 10 months later showed no active lesions. The patient’s symptoms are currently controlled at 16 months from the beginning of therapy. Some months later skin lesions appeared and were diagnosed as follicular psoriasis and treated with topical steroid.
Case 2
SC is a 15-year-old boy who came to our attention in June 2014 after a 5-year history of migrant pain. During that period the child underwent several plain X-rays, all negative. The child was left motherless some years before and his pain was considered mostly due to psychological problems. At first evaluation in our Centre, he presented morning stiffness and pain in the left scapular region together with dorsal backache, without signs of inflammation. A right dorso-lumbar scoliosis was detected. Blood tests showed alterations in inflammatory indexes (ESR 61 mm and CRP 2.31 mg/dL) and negative anti-nuclear antibodies. IGRA test was negative. Suspecting a CRMO, the child underwent a wbMRI showing bilateral multiple signal alterations at the bone metaphysis and epiphysis of distal humeri, distal and proximal femurs, greater trochanters, distal and proximal tibiae and more tenuous alterations at proximal humeri and at right wrist. Other signal alterations were present at the fifth lumbar vertebral body (L5) and at the pelvis (from sacrum and iliac wings to acetabulum). Another cervico-dorsal spine MRI showed signal alterations at C4, C6, C7, T4, T6, T8 and T9 level with partial collapse of C4 and complete vertebral collapse of C7, depression of the superior endplate of C5 and T4. Moreover, signal alterations were present in the spinous processes of T9, T10 and T11. Bone scintigraphy was performed and revealed increased uptake along the distal extremity of the right clavicle and the left greater trochanter. Moreover, he underwent bone marrow aspiration which was negative for malignant cells. The diagnosis of CRMO was then established and the boy started steroid therapy with slow clinical and radiological improvement.
A few months later he experienced a clinical relapse at the lumbar spine and the sacroiliac joint associated with severe functional impairment; it was therefore decided to start therapy with pamidronate while tapering glucocorticoids (Fig. 2). He underwent six cycles of three monthly infusions without either complete clinical or radiological improvement and with persistently elevated inflammation indexes. He started therapy with etanercept and the MRI evaluation 3 months later showed dramatic regression of the previously described lesions and all the disease activity parameters improved. The patient is now free of symptoms 12 months from the beginning of biologic therapy.
Patient 2: total body MRI before and after therapy with bisphosphonates. Coronal STIR images showing hyperintensity in proximal femurs and greater trochanters (a); in distal femurs, proximal tibiae (b); and in distal tibiae (c). d Coronal STIR: resolution of bone signal alterations in femurs, knees (e) and distal tibiae (f)
Case 3
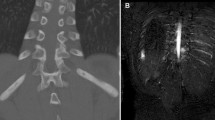
CR is a 7-year-old girl who came to our attention on March 2014. Three years before she suffered from stiff neck and difficulty in walking for which she underwent a brain and cervical spine MRI showing intra-articular fluid at C1–C2 level and inflammatory intervertebral subluxation. Anti-inflammatory therapy was started with clinical improvement. After 9 months she suffered from migrant pain at thoraco-cervical level for a few days. X-ray examination did not show any alteration but, for the persistence of symptoms, she underwent dorsal MRI which showed a vertebral collapse at the sixth thoracic vertebra (T6) with peri-lesional oedema. Suspecting an oncologic aetiology she underwent positron emission tomography which showed an area of hyperfixation at the superior endplate of T6 and at the soft tissue posterior to the right femoral neck. A computed tomography-guided biopsy was then performed revealing chronic osteomyelitis with negative cultural tests. IGRA test was negative. The child was then referred to our Centre. We performed a further cervical spine MRI which revealed a mild intra-articular effusion at C1–C2 level, an inflammatory synovial thickening and contrast enhancement after gadolinium injection. She started an anti-inflammatory therapy with clinical-instrumental improvement. Some weeks later she started to complain of occasional right thoracic, tibial and cervical pain and later a painful and hyperaemic swelling of the left ankle appeared. Suspecting CRMO, we performed a wbMRI which revealed multiple areas of signal hyperintensity: a subtle round area at the right sterno-clavicular joint, at the right upper trochanteric region and at the left femoral neck, at bilateral tibial distal metaphysis and at the distal epiphysis of the left fibula; “vertebra plana” sign at T6 level. She started steroid therapy with great clinical improvement, confirmed by MRI; the therapy was gradually tapered and completely stopped in April 2015. However, significant pain recurred 6 months later in the left ankle so therapy with bisphosphonates was started. After an initial good clinical response, after six cycles of pamidronate she had recurrence of pain and swelling in the left ankle. The MRI showed new areas of signal hyperintensity in the tibial epiphysis bilaterally and in the peroneal metaphysis with post-contrastographic enhancement (Fig. 3). For this reason therapy with etanercept was started in February 2016. Some months earlier plantar pustulosis appeared and started recurring. The wbMRI performed 7 and 13 months later showed no active lesions and the child is in good clinical condition.
Case 4
BL is a 11-year-old girl who came to our attention in October 2015 after one year of limping and pain in the right inguinal region, sometimes treated with aspirin with good response. After a fracture of the right tibia in April, she suffered from persistent pain in the ipsilateral knee. At clinical evaluation a painful functional limitation was detected in the right knee and hip. The suspicion of CRMO was confirmed by wbMRI showing diffuse signal alteration in the right knee, in the diaphyseal and epiphyseal region of femur and tibia bilaterally, in the right ankle and in the astragalus. The girl underwent a bone biopsy that showed chronic inflammation with negative culture.
Considering the significant painful symptomatology reported and her limitation in daily activities, oral steroid therapy was started, but only minimal response occurred. It was thus decided to add biologic treatment with etanercept in April 2016. The radiological follow-up with MRI 1 year later showed a progressive improvement of bone lesions without complete remission and the girl intermittently needed short cycles of NSAID.
Discussion
CRMO is an autoinflammatory bone disorder mostly affecting children and adolescents. Multifocal lytic bone lesions with swelling and pain are the most characteristic features of the disease. The clinical spectrum ranges from mild, self-limiting form to prolonged and recurrent courses [12]. CRMO may be part of a spectrum of diseases where isolated bone inflammation could be the paediatric presentation of SAPHO syndrome, which includes synovitis, acne, pustulosis, hyperostosis, and osteitis. The aetiology of CRMO is not completely understood. Infections seem not to be involved, as a matter of fact wide microbiological analysis resulted negative and antibiotics were ineffective. It has been suggested that imbalance between pro-inflammatory cytokines like interleukin [IL]-6, IL-1, TNF-alpha and anti-inflammatory cytokines like IL-10 may be involved in disease pathogenesis [13].
Evidence for a genetic basis is also present in non-syndromic or sporadic CRMO. In fact, the prevalence of inflammatory bone disease among patients’ relatives varied between 12 and 32% in large cohorts of patients with CRMO [14], and several reports described families with multiple affected members or a high incidence of psoriasis, inflammatory bowel disease, and other chronic inflammatory conditions in first-degree relatives [15]. This suggests a continuum between autoinflammation and autoimmunity.
There are no randomized-controlled trials about treatment options in CRMO. NSAID (ibuprofen and naproxen) are commonly used as first-line therapy [2, 16]. However, according to different studies, only almost 50% maintained stable clinical remission without further treatment [17]. In individuals who fail to reach clinical and radiographic remission in response to NSAID treatment, oral corticosteroids may be administered. Patients who fail to respond to NSAID and repeated oral corticosteroid courses should be treated more aggressively. Possible options are the classic disease modifying antirheumatic drugs, like methotrexate; they are more commonly used in North America [8]. Positive outcomes have been obtained with bisphosphonates, in particular with intravenous pamidronate [7]. Pamidronate can be administered following two different protocols: an initial dose of 0.5 mg/kg/day followed by 1 mg/kg/day (maximum 60 mg) on days 2 and 3 every 3 months for a total of 3–4 courses, or 1 dose of 1 mg/kg (very first dose 0.5 mg/kg, maximum 60 mg) every month for 1–6 months [18, 19].
Recently, a report of the use of an oral bisphosphonate (alendronate) has been published [20]. Alendronate is tenfold more potent than pamidronate; numerous studies in children with osteogenesis imperfecta showed that oral alendronate and intravenous pamidronate are equally effective.
In the last years, successful use of biologic agents like TNF-α inhibitors has been reported [8,9,10,11]. However, in the absence of randomized placebo-controlled trials, retrospective evaluation of clinical courses is the only available approach to understand treatment responses in CRMO. Moreover, there are few reports of good response of the inflammatory bone lesions to an IL-1 blocking therapy [9]. We reviewed the published data about biologic therapy for CRMO performing a comprehensive search through Pubmed, MEDLINE, EMBASE, Scopus, and Web of Science. The key words included were “chronic recurrent multifocal osteomyelitis” together with “biologic therapy” or “anti-TNF” or “Etanercept” or “Infliximab”. We analysed the review articles and case reports. We also checked the references list of relevant studies to identify additional studies. We decided to exclude cases of CRMO associated with palmoplantar pustulosis, SAPHO syndrome or Majeed syndrome (Table 1).
We described four children affected by CRMO with persistent pain despite treatment with NSAID, glucocorticoids and bisphosphonates. The mean age at symptoms onset and diagnosis was 8 years and 10 years and 10 months, respectively. Two patients presented with back pain and three had vertebral lesions.
Patients’ characteristics are described in Table 2.
Mean interval from diagnosis to the onset of TNF-α inhibitors treatment was 14 months. Between etanercept and infliximab, we chose the first since it can be given at home rather than by intravenous infusion, and immediate adverse reactions are less likely. Etanercept dose was 0.8 mg/kg per week and no adverse reactions were reported. However, 2 of our patients developed skin lesions while on therapy (Cases 1 and 3). It is not clear if it is a side effect of the treatment or, more likely, another aspect of the disease. The biologic treatment resulted in progressive and sustained clinical remission and radiological control of the disease in all patients, only 1 child showed a slow improvement and needed short cycles of NSAID.
Until now it has not been possible to define a predictive score of disease severity able to help in the therapeutic choice. Wipff et al. [14] showed that a longer time from symptom onset to diagnosis is associated with a worse outcome, while none of the other demographic or disease characteristics correlates with remission. The assessment of disease activity remains somewhat unclear. Beck et al. provided the Pediatric CNO (PedCNO) score, which includes 5 measures: ESR, number of radiological lesions, severity of disease estimated by the physician, severity of disease estimated by the patient or parent, and the Childhood Health Assessment Questionnaire [16].
Therefore, the optimal approach to the management of CRMO remains unknown and further prospective studies are required to compare different treatments and to determine the long-term efficacy and safety of biologic agents in children with CRMO. According to our small experience, we suggest considering therapy with etanercept for the treatment of severe cases with persistently active disease despite multiple treatments.
References
Jurik AG, Helmig O, Ternowitz T, Muller BN (1988) Chronic recurrent multifocal osteomyelitis: a follow-up study. J Pediatr Orthop 8:49–58
Huber AM, Lam PY, Duffy CM, Yeung RS, Ditchfield M, Laxer D et al (2002) Chronic recurrent multifocal osteomyelitis: clinical outcomes after more than five years of follow-up. J Pediatr 141:198–203
Jansson A, Renner ED, Ramser J, Mayer A, Haban M, Meindl A et al (2007) Classification of non-bacterial osteitis: retrospective study of clinical, immunological and genetic aspects in 89 patients. Rheumatology (Oxford) 46:154–160
Jurriaans E, Singh NP, Finlay K, Friedman L (2001) Imaging of chronic recurrent multifocal osteomyelitis. Radiol Clin North Am 39:305–327
Kim YS, Lee J, Kim HS (2013) Sternocostal involvement in chronic recurrent multifocal osteomyelitis associated with ulcerative colitis. Rheumatol Int 33:2889–2892
Holden W, David J (2005) Chronic recurrent multifocal osteomyelitis: 2 cases of sacral disease responsive to corticosteroids. Clin Infect Dis 40:616–619
Hofmann C, Wurm M, Schwarz T, Neubauer H, Beer M, Girschick H et al (2014) A standardized clinical and radiological follow-up of patients with chronic non-bacterial osteomyelitis treated with pamidronate. Clin Exp Rheumatol 32:604–609
Eisenstein EM, Syverson GD, Vora SS, Williams CB (2011) Combination therapy with methotrexate and etanercept for refractory chronic recurrent multifocal osteomyelitis. J Rheumatol 38:782–783
Eleftheriou D, Gerschman T, Sebire N, Woo P, Pilkington CA, Brogan PA (2010) Biologic therapy in refractory chronic non-bacterial osteomyelitis of childhood. Rheumatology (Oxford) 49:1505–1512
Marangoni RG, Halpern AS (2010) Chronic recurrent multifocal osteomyelitis primarily affecting the spine treated with anti-TNF therapy. Spine (Phila Pa 1976) 35:E253-6
Batu ED, Ergen FB, Gulhan B, Topaloglu R, Aydingoz U, Ozen S (2015) Etanercept treatment in five cases of refractory chronic recurrent multifocal osteomyelitis (CRMO). Joint Bone Spine 82:471–473
Schnabel A, Range U, Hahn G, Berner R, Hedrich CM (2017) Treatment response and longterm outcomes in children with chronic nonbacterial osteomyelitis. J Rheumatol 44:1058–1065
Taddio A, Zennaro F, Pastore S, Cimaz R (2017) An Update on the pathogenesis and treatment of chronic recurrent multifocal osteomyelitis in children. Paediatr Drugs 19:165–172
Wipff J, Costantino F, Lemelle I, Pajot C, Duquesne A, Lorrot M et al (2015) A large national cohort of French patients with chronic recurrent multifocal osteitis. Arthritis Rheumatol 67:1128–1137
Bousvaros A, Marcon M, Treem W, Waters P, Issenman R, Couper R et al (1999) Chronic recurrent multifocal osteomyelitis associated with chronic inflammatory bowel disease in children. Dig Dis Sci 44:2500–2507
Beck C, Morbach H, Beer M, Stenzel M, Tappe D, Gattenlohner S et al (2010) Chronic nonbacterial osteomyelitis in childhood: prospective follow-up during the first year of anti-inflammatory treatment. Arthritis Res Ther 12:R74
Kaiser D, Bolt I, Hofer M, Relly C, Berthet G, Bolz D et al (2015) Chronic nonbacterial osteomyelitis in children: a retrospective multicenter study. Pediatr Rheumatol Online J 13:25
Hospach T, Langendoerfer M, von Kalle T, Maier J, Dannecker GE (2010) Spinal involvement in chronic recurrent multifocal osteomyelitis (CRMO) in childhood and effect of pamidronate. Eur J Pediatr 169:1105–1111
Miettunen PM, Wei X, Kaura D, Reslan WA, Aguirre AN, Kellner JD (2009) Dramatic pain relief and resolution of bone inflammation following pamidronate in 9 pediatric patients with persistent chronic recurrent multifocal osteomyelitis (CRMO). Pediatr Rheumatol Online J12; 7:2
Daishi Hirano Kosuke, Chiba, Saya Yamada and Hiroyuki Ida (2017) Oral alendronate in pediatric chronic recurrent multifocal osteomyelitis. Pediatr Int 59:506–508
Carpenter E, Jackson MA, Friesen CA, Scarbrough M, Roberts CC (2004) Crohn’s-associated chronic recurrent multifocal osteomyelitis responsive to infliximab. J Pediatr 144:541–544
Deutschmann A, Mache CJ, Bodo K, Zebedin D, Ring E (2005) Successful treatment of chronic recurrent multifocal osteomyelitis with tumor necrosis factor-alpha blockage. Pediatrics 116:1231–1233
Stern S, Marzan K, Borzutzky A, Steinberg E, Reiff A (2010) Use of TNF antagonists in the treatment of chronic non-bacterial osteomyelitis (CNO) (abstract). Arthritis Rheum 62 Suppl 10:241. https://doi.org/10.1002/art.28010
Barral Mena E, Freire Gómez X, Enríquez Merayo E, Casado Picón R, Bello Gutierrez P, de Inocencio Arocena J (2016) [Non-bacterial chronic osteomyelitis: experience in a tertiary hospital]. An Pediatr (Barc) 85:18–25
Walsh P, Manners PJ, Vercoe J, Burgner D, Murray KJ (2015) Chronic recurrent multifocal osteomyelitis in children: nine years’ experience at a statewide tertiary paediatric rheumatology referral centre. Rheumatology (Oxford) 54:1688–1691
Moussa T, Bhat V, Kini V, Fathalla BM (2017) Clinical and genetic association, radiological findings and response to biological therapy in seven children from Qatar with non-bacterial osteomyelitis. Int J Rheum Dis 20:1286–1296
Catalano-Pons C, Comte A, Wipff J, Quartier P, Faye A, Gendrel D, Duquesne A et al (2008) Clinical outcome in children with chronic recurrent multifocal osteomyelitis. Rheumatology (Oxford) 47:1397–1399
Aygun D, Barut K, Camcioglu Y, Kasapcopur O (2015) Chronic recurrent multifocal osteomyelitis: a rare skeletal disorder. BMJ Case Rep 2015. https://doi.org/10.1136/bcr-2015-210061
Author information
Authors and Affiliations
Contributions
Authors disclose involvement of any external agent in language editing. ET and AM conceptualized and designed the study; acquired, analysed and interpreted the data, drafted the initial manuscript, and approved the final manuscript as submitted. MB and LG performed the radiological exams, acquired, analysed and interpreted the data, critically reviewed the manuscript, and approved the final manuscript as submitted. AP substantial contributed to the conception of the study, revised the manuscript critically for important intellectual content, and gave final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. Standard care treatment was provided, and the patients were not part of a research study. For this type of article, formal ethical approval is not required.
Informed consent
Consent from the parents/LARs of the patients below 16 years for publication was obtained.
Rights and permissions
About this article
Cite this article
Tronconi, E., Miniaci, A., Baldazzi, M. et al. Biologic treatment for chronic recurrent multifocal osteomyelitis: report of four cases and review of the literature. Rheumatol Int 38, 153–160 (2018). https://doi.org/10.1007/s00296-017-3877-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-017-3877-0