Abstract
To systematically search for the availability of evidence for exercise impacting on sleep for people who have rheumatoid arthritis. Two reviewers independently searched seven electronic databases, identified and extracted relevant studies by applying eligibility criteria. Sources of bias were assessed independently by two reviewers using the Cochrane bias assessment tool for randomized controlled trials (RCTs) and Newcastle–Ottawa Quality Assessment Scale for non-RCTs. Data were synthesized using a level of evidence approach. Meta-analyses were deemed to be inappropriate due to the heterogeneity of study designs, measurement tools and interventions. Five studies were included: one RCT; two pilot RCTs and two samples of convenience. A total of 262 people with RA were included. Interventions used were difficult to assess due to the heterogeneity of study designs and the inclusion of two using different types of yoga as an intervention. Different sleep outcome measures were used thus, it was not feasible to pool results. Studies had a high risk of bias. This review could find no consistent or conclusive evidence on whether exercise impacts on sleep in people who have rheumatoid arthritis, therefore no firm conclusions can be made. However, there is some indication that exercise may have positive benefits on sleep in people who have rheumatoid arthritis. Further studies with improved study designs, using subjective and objective measures, are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is an autoimmune disease, which causes chronic inflammation of the joints and injury to the organs of the body [1], which can lead to people with RA not being as physically active as their healthier counterparts [2, 3]. A significant body of research has investigated the effects of physical activity and exercise on sleep, in the general population. Results generally suggest that they are beneficial for sleep; however, it is unclear how large these benefits are, and to what extent variables such as age and type and duration of exercise moderate these benefits [4]. Current practice guidelines, recommend exercise as a key component in the management of people with RA however, what is lacking is its effect on sleep quality and sleep disturbances.
It has been well established that regular exercise is important for those who have been diagnosed with RA and has been shown to increase muscle strength, improvements in cardiovascular fitness and reduction in pain. The position stand from the American College of Sports Medicine (ACSM) regarding exercise for those with chronic conditions is categorized by cardio-respiratory exercise, resistance exercise, flexibility exercise and neuro-motor exercise [5].
Sleep is an important aspect of maintaining the body’s circadian rhythm. In general getting fewer than 5 h sleep per day has been associated with cardiovascular problems, diabetes and obesity and can also be linked to depression, anxiety and poor productivity [6–8]. Poor sleep is a common complaint among people with RA with disturbed sleep and fatigue known to affect up to 70% in this population [9, 10]. This consequently has an effect on their quality of life, in addition to mental and physical health.
It is known that exercise improves mood state [11], which can also be an additional factor in improving or indeed disrupting quality of sleep [12]. Exercise has been identified as an important part of the non-pharmacological management of poor sleep and in improving sleep quality [13, 14] however, people with RA were previously cautioned about undertaking exercise. It was noted in a 2013 Cochrane review [15], of exercise and fatigue, that sleep quality was yet to be examined. Therefore, changes in sleep quality should be evaluated through exercise so that we can understand more the potential for long-term changes in overall health status, in people who have RA.
The aim of this review is to systematically search for the availability of evidence for exercise in sleep for people who have RA and to determine its quality and strength, with the goal of informing an exercise intervention looking at the effect on sleep in this population.
Materials and methods
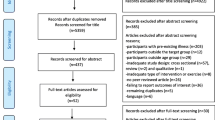
Reporting of this systematic review has been guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [16]. A protocol outlining the review strategy and methods of analysis was registered with a registry of systematic reviews http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015027943.
Eligibility criteria
Types of studies and population
Randomized controlled trials (RCT), controlled clinical trials (CCT) without randomization, cross-sectional, case controlled and cohort studies were all considered. Only those publications in English were considered and participants were people who were aged 18 years or older with a confirmed diagnosis of RA according to the American College of Rheumatology classification criteria [17] or the American College of Rheumatology/European League Against Rheumatism classification criteria [18].
Types of interventions and outcomes
Studies were required to include exercise and its outcomes on sleep in people who have RA. Studies comparing exercise interventions with no exercise were also included with no specificity regarding setting.
Search strategy
A comprehensive search of the literature was performed by two reviewers (SMcK and LC) in January 2016, to identify published literature in relation to exercise interventions on sleep in people who have RA. The following databases were searched: EbscoHost (Academic Search Complete, AMED, CINAHL, MEDLINE and SPORTDiscus), PUBMED and Web of Science. Based on a scoping review undertaken to determine the best terms to use, a combination of these key terms and MeSH headings were utilized: rheumatoid arthritis OR rheumatoid arthritis patients OR rheumatoid sufferers OR RA AND exercise OR physical activity OR sleep OR sleep quality OR sleep disturbance. Grey literature were also searched through appropriate sources for conference abstract publications and the search was also extended by secondary searching through the reference lists of papers retrieved, to identify any additional suitable references.
Following the removal of duplicates, two authors (SMcK & LC) independently assessed titles and abstracts of the total search for relevance based on the eligibility criteria. These authors then independently assessed the remaining full text articles for eligibility. A third independent reviewer (NK) was available for consultation if disputes arose however, this was not required. A consensus method was utilized to solve disputes regarding the study articles to include or exclude.
Where abstracts were returned without the availability of a full text article authors were contacted, by email, to identify the origin of the abstract, ascertain if it had been published and to request a means of accessing same in an effort to include all relevant studies. In a similar manner, where a study did not present all relevant data or if additional data was deemed necessary authors were contacted for access to this information.
Data extraction
A data extraction template based on the Cochrane recommendations was piloted on two randomly selected studies and modified accordingly for this review [19]. For each article that met the inclusion criteria, the following information was recorded by the reviewer: (1) study citation, (2) study population, i.e. number of participants, age range, % of total study population that was RA (3) study design, (4) outcome measures used, (5) interventions delivered, using the Frequency, Intensity, Time & Type (FITT) principle (6) the statistical tests utilized and (7) results. Means and standard deviations were extracted utilising spreadsheets (Microsoft Excel 2010).
Quality assessment
An important step in conducting a systematic review is to assess the methodological quality of each included trial. Variations in study quality can explain differences in the findings of studies that are included in a systematic review. As a result, the quality of a study will reflect the strength of the evidence that can be drawn from it [20]. As both randomized and non-randomized studies (RCTs) were included in this review, a number of systems to appraise the studies had to be applied:
For RCTs the Cochrane Collaboration risk of bias tool was used [19]. This consists of seven domains (selection, detection, performance, attrition, reporting, allocation concealment and other issues). Each domain in the tool requires a specific entry(s) and consists of two parts. The first part of the tool describes what was reported to have happened in the study, in sufficient detail to support a judgement about the risk of bias, while the second part of the tool assigns a judgement relating to the risk of bias for that entry [19]. This was achieved by assigning a judgement of ‘Low risk’ of bias, ‘High risk’ of bias, or ‘Unclear risk’ of bias. When one or more of the domains were not met then there was a high risk of bias. Disagreements between the reviewers about these entries were resolved through discussion to achieve consensus.
For non-randomized studies the Newcastle–Ottawa Scale (NOS), with some modifications was used [21]. This system assesses the quality of the studies in three main areas: selection, comparability, and/or outcome and exposure. As this review is looking at the availability for evidence, the scale was modified to include assessment of the validity and reliability of the outcome measure used, in addition to the statistics used. Stars are awarded for appropriate fulfilment of each criteria with a maximum of four stars for section one, two stars for section two and three stars for section three, giving a possible maximum total score of nine stars. The quality of the studies was carried out independently by two authors (SMcK & LC). Where disagreement occured both authors deliberated until a consensus was reached.
Results
Study selection
The search strategy and selection process is summarized as per the PRISMA flowchart [16], which is presented in Fig. 1. A total of five studies were included in this review [22–26].
Study characteristics
Of the five studies, one was an RCT [26], two were pilot RCTs [22, 24] with the final two sample of conveniences [23, 25]. Study characteristics are included in Table 1. A total of 262 people with arthritis are included in this review, all of whom had a confirmed medical diagnosis of RA according to the ACR [17] or ACR/EULAR [18] criteria. In four of the studies the population was people with RA, while in the fifth the population was a mixed population of RA and ankylosing spondylitis (AS). The mean study sample size was 52 (range 20–93), with the majority of participants being female (70%), which is slightly lower than the 75% reported by the American college of Rheumatology [27].
Outcome measure used
Two studies used the Pittsburgh sleep quality index (PSQI) as their sleep outcome measure [25, 26], one used a subscale from the Nottingham Health Profile—Swedish version (NHP) [23], one the Insomnia Severity Index (ISI) [22] and one a Weekly Monitoring Form (WMF) [24].
The PSQI is an outcome measure used to assess sleep quality and disturbances in adults, over the preceding month [28, 29] and can be completed in 10 min. It characterizes ‘poor’ from ‘good’ sleep quality by measuring seven variables: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunction. The range for this measure is 0–21, with a higher score indicating worse sleep quality. The PSQI has been used in a number of disease areas [30], as an outcome in clinical trials [31] and has also been used to evaluate sleep quality in rheumatoid arthritis (RA) [32].
The NHP is an outcome measure intended for primary health care and can be completed in 5 min [33, 34]. It contains 38 statements of subjective concerns encompassing six different sub-areas: pain, energy level, physical mobility, sleep, emotional reactions and social isolation ref. Each question is answered Yes or No with each section score being weighted. The higher the score, the greater is the number and severity of problems. Each question is assigned a weighted value; with sleep being five and the sum of all weighted values in a given subarea adds up to 100.
The ISI a seven-item questionnaire, which asks the person to rate the nature and symptoms of their sleep problems using a five-point Likert scale (0 = no problem, 4 = very severe problem) [35, 36] and can be completed in 5 min or less. Questions relate to subjective qualities of sleep, including the severity of symptoms, satisfaction with his/her sleep patterns, the degree to which insomnia interferes with daily functioning, how noticeable any insomnia is to others, and the overall level of distress created by the sleep problem.
A WMF is a self-designed form and can be used to monitor and assess numerous questions using a Likert-type scale and can be used within 5 min. In this outcome it was used to assess a participants’ ‘difficulty staying asleep for the entire night’ from 0 (no difficulty) to 10 (very difficult). Full details are summarized in Table 2.
None of the outcome measures discussed above were developed specifically for rheumatologic or musculoskeletal conditions [37]. Each scale has relied heavily on populations with primary sleep disorders for validation [38]. Of the five outcome measures listed above, the PSQI and the ISI have been used to varying extents in rheumatologic populations [39]. Numerous studies using the PSQI in a variety of older adult populations internationally have supported high validity and reliability [37] and it has been used to evaluate sleep quality in RA [32].
Outcome measure results
Pittsburgh Sleep Quality Index (PSQI)
An RCT from Ireland, found that sleep quality improved significantly (p = 0.04) based on their exercise programme [26]. While a sample of convenience from the Arthritis Foundation Exercise Program (AFEP) in the US, ANOVA revealed a statistically significant difference in scores between the groups (f (3,72) = 4.892, p < 0.05) [25]. Tukey post hoc analysis showed statistically significant differences in total scores between the pre- and post-scores within the experimental group. However, while AFEP participants did increase sleep quality/disturbance, this was not significantly different compared to the comparison group.
Nottingham Health Profile: sleep subscale (NHP)
A Swedish sample of convenience, based in rehabilitation centres in Tenerife and Israel using people with RA as 48% of the total participants, found an improvement in overall NHP and sleep sub-score. The sleep sub-score was statistically significant shortly after (p < 0.001), after 3 months (p < 0.005) and after 6 months (p < 0.001) [23].
Insomnia Severity Index (ISI)
A pilot RCT from New Zealand, published as a conference paper/abstract, showed that while no group effects of yoga compared to usual care were reported, individual clinical improvements in sleep were at a higher rate among Yoga participants compared to usual care [22].
Weekly monitoring form
Using mixed model tests, a second pilot RCT from the USA, showed a decrease in sleep difficulty but this was not statistically significant (f (181) = 1.59, p = 0.10).
Interventions
Interventions used were diverse, with Hafstrom and Hallengren’s [23] consisting of dynamic and static exercise programs on land and in heated swimming pools, with therapy given in either Tenerife or Israel, over a 4-week period. Individual adjustments were done due to responses to therapy. Durcan et al. [26] was the most comprehensive programme which included cardiovascular, resistance training, flexibility and neuromotor conditioning, with full evaluation carried out at baseline and 12 weeks.
McManus et al. [25] was concerned with the Arthritis Foundation Exercise Program (AFEP) which was created by the Arthritis Foundation, in the US, to promote self-management of the disease through an 8-week group recreational exercise program [40].
Evans et al. [24] was based on a 6-week Iyengar yoga program, with a 2 months follow up.
Ward et al. [22] focused on the feasibility and safety of an 8-week relaxation focused Yoga intervention, with measures taken at baseline, week-9 and week-12.
Risk of bias within studies
The Cochrane risk of bias form was used to assess the RCT [26] and two were pilot RCTs [22, 24], and the risk of bias was high, with results summarised in Table 3. All three studies had low risk of bias for selection, attrition and reporting, with performance bias being high. Detection, allocated concealment and other bias were unclear.
The Newcastle–Ottawa Scale, with some modifications was used for the two sample of conveniences [23, 25] and is included in Table 4. The overall methodological quality of the included studies was varied, with total scores ranged from five to seven stars. Neither study satisfied the criteria relating to adequate representation of the case population, predisposing the increased likelihood of selection bias.
Based on the above results a meta-analysis was not undertaken due to the heterogeneity of study designs, participants, interventions and reported outcome measures.
Discussion
As far as we are aware this is the first systematic review looking at the availability of evidence for exercise and sleep, in people who have rheumatoid arthritis. The small number of studies, their heterogeneous nature and a high risk of bias prevent firm conclusions being drawn and therefore, restrict the generalizability of findings. It was therefore, deemed inappropriate to undertake a meta-analysis.
However, based on these limited number of studies they do indicate some positive results with regard to sleep quality and disturbances and improvements in same, due to exercise.
Outcome measures
The study of sleep disturbances can be challenging as gold standard tests like polysomnography can be both expensive and require an additional commitment of time from participants [39]. There is, therefore, a strong incentive to have other non-laboratory based studies to justify utilizing other outcome measures, in both clinical and home settings, for assessing sleep patterns in rheumatologic diseases. From this review four different sleep outcome measures were used, all subjective, however, not all meet the Outcome measures in Rheumatology (OMERACT) criteria for validity, feasibility and discrimination of differences [41]. It is acknowledged that subjective measures are cheaper and easier to administer however, it is important to choose a method to measure exercise that will allow for continuous and detailed recording of usual activity [42], which should also include sleep patterns.
The two studies that used the PSQI showed that sleep quality improved significantly although McManus et al. state that their AFEP participants were not significantly different compared to the control [25]. From the literature, the PSQI seems to be the most widely used general measure of sleep quality available. Strengths of the measure include its range of coverage of multiple dimensions of sleep quality, its flexibility as a brief clinical tool, its demonstrated use in chronic pain research and is one of the few measures of sleep that incorporate questions relating to daytime sleepiness. However, as PSQI’s items refer to ratings of sleep over the previous month, it may be less sensitive to estimating significant changes over time or with brief intervention periods.
The use of the ISI showed clinical improvements in sleep. The ISI has been validated against both polysomnographic and prospective sleep diary measures and demonstrates convergence with clinical interview criteria [35]. While it was not specifically developed for rheumatology patients, scale development included a heterogenous group of patients with insomnia secondary to pain conditions. Due to its brevity and Likert scale data, this instrument would not be an appropriate stand-alone measure of sleep disturbance [43]. The scale is limited to questions connected to severity and impact of insomnia and does not assess frequency of symptoms. It also does not include items relevant to other sleep disorders, which may occur more frequently in chronic pain populations.
Results using the NHP did show that improvements in sleep were significant. However, the NHP is designed to measure a person’s view of their overall health status, in six different areas with sleep just one of those areas. It has been used in research studies worldwide in order to determine the effect a given disease has on a patient’s quality of life, including insomnia [44] and sleep [45]. However, like the ISI would not be an appropriate stand-alone measure of sleep disturbance.
Finally, using the WMF showed a decrease in sleep difficulty. A WMF is a simple way to subjectively assess any type of condition, in this case sleep difficulty, using a numeric rating scale (NRS). The WMF would not be an appropriate scale to use as an outcome measure to ascertain the effectiveness of exercise on sleep, as it is unable to capture different sleep related domains like the other measures. Combining the PSQI with prospective monitoring such as daily sleep diaries or actigraphy is recommended [43]. In addition supplementing an assessment of sleep in rheumatology patients with measures of fatigue, with either the Stanford Sleepiness Scale (SSI) [46] or the Epworth Sleepiness Scale (ESS) [47], is also recommended [43].
Interventions
Exercise programmes used were difficult to assess and compare according to the frequency, intensity, time and type (FITT) principle due to the heterogeneity of study designs and the inclusion of two using different types of Yoga as an intervention.
Poor cardiovascular health is the main cause of death in people with RA as they tend to have poor cardio respiratory fitness. Therefore, the inclusion of aerobic exercise as part of treatment is essential, which was included in three of the included studies [23, 25, 26], with the other two studies comprising of yoga [22, 24]. The addition of resistance exercises helps to mitigate rheumatoid cachexia and other musculoskeletal and joint health issues. Both types of exercises may need to be required for maintaining bone mineral density [48] and was included in three of the studies [23, 25, 26]. The current ACSM guidelines recommend moderate intensity aerobic exercise for a minimum of 30 min, 3–5 times per week and 2–3 days per week for resistance exercise [49]. However, the ACSM also recommend stretching to improve flexibility and balance work due to problems with lower-extremity arthritis and these were only used by three of the studies.
Pharmacologic interventions have improved the management of RA however, physical activity (PA) and exercise remain an important part of overall treatment [50]. The language used regarding PA and exercise is extremely important. During the conduct of this review it was found that authors and health professionals sometimes use PA and exercise interchangeably however, they are quite different considerations. Indeed from the literature some studies used PA, exercise and physical function interchangeably within their texts. This can further make it difficult to compare any findings. PA is defined as ‘any bodily movement produced by skeletal muscles that results in energy expenditure’ while exercise is ‘a subset of PA, which is planned, structured and repetitive’ [51] with the view to improving or maintaining physical fitness. Structured exercise confers benefits at low risk in a majority of people with RA [52, 53], therefore, it is important to clarify the difference when planning an intervention, prior to it being studied and researched.
Limitations
Non-randomized controlled trials were included in this review to increase its scope however, this simultaneously increased its risk of bias. This risk coupled with the diversity of design makes reviewing the methodological quality challenging.
According to the literature there are numerous appraisal tools however, no gold standard exists for evaluating risk of bias. In this review we took the decision to use the Cochrane risk of bias and Newcastle–Ottawa Quality Assessment Scale on the basis of the design of the included studies.
The heterogeneous nature and methodological limitations of the included studies prevent firm conclusions being drawn and restrict the generalizability of findings.
Consideration should be paid to the exercise habits of those participants prior to any study which may or may not affect any results [6] however, this was not part of the objectives for this review.
Future research
While exercise benefits for people with RA are widely acknowledged, further studies are required to investigate its effect on sleep and therefore, the most effective exercise prescription in terms of the FITT principle, the ideal approach to exercise delivery and indeed how compliance can be promoted.
Future research should include a control arm which receives usual care, which should include the provision of information regarding exercise, which will allow for a fair evaluation of the actual intervention.
Improving the overall quality of research should serve to improve the quality and overall effectiveness of interventions in increasing exercise in people who have RA. The accurate measurement of sleep is also imperative and it is recommended that only measures which have been found reliable and valid in the RA population be used in future research. This would also address any risk of detection bias which only use self-report outcome measures. Long-term follow-up is also suggested in all future studies to explore whether any beneficial effects are maintained.
Exercise offers a potentially attractive alternative or adjuvant treatment for those people with RA who have sleep issues however, examination of a participant’s exercise habits prior to any study would be important as it may have an impact on its effectiveness.
Conclusion
The small number of studies available, heterogeneity of study designs and measurement tools coupled with a high level of bias limit any firm conclusions that may be drawn regarding exercise and sleep in people who have RA. However, there is some indication that exercise may have positive effects with regard to sleep quality and disturbances and improvements in same.
More studies using both subjective and objective measures of sleep are necessary to confirm these findings and need to be replicated using a large sample size with appropriate size calculations. In addition, PA and exercise need to be strictly defined, prior to any intervention being undertaken, which would ultimately result in more comparability.
References
Firestein GS (2005) Immunologic mechanisms in the pathogenesis of rheumatoid arthritis. JCR. J Clin Rheumatol 11:S39–S44
Eurenius E, Brodin N, Lindblad S, Opava CH, Group PS (2007) Predicting physical activity and general health perception among patients with rheumatoid arthritis. J Rheumatol 34:10–15
van den Berg MH, de Boer IG, le Cessie S, Breedveld FC, Vlieland TPMV (2007) Are patients with rheumatoid arthritis less physically active than the general population? JCR J Clin Rheumatol 13:181–186
Driver HS, Taylor SR (2000) Exercise and sleep. Sleep Med Rev 4:387–402
Moore G, Durstine JL, Painter P (2016) ACSM’s exercise management for persons with chronic diseases and disabilities, 4th edn. American College of Sports, Human Kinetics, pp 15–30
Youngstedt SD (2005) Effects of exercise on sleep. Clin Sports Med 24:355–365
Lucassen PJ, Meerlo P, Naylor AS, Van Dam AM, Dayer AG, Fuchs E, Oomen CA, Czeh B (2010) Regulation of adult neurogenesis by stress, sleep disruption, exercise and inflammation: Implications for depression and antidepressant action. Eur Neuropsychopharmacol 20:1–17
Pickering TG, Harshfield GA, Kleinert HD, Blank S, Laragh JH (1982) Blood pressure during normal daily activities, sleep, and exercise: comparison of values in normal and hypertensive subjects. JAMA 247:992–996
Van Hoogmoed D, Fransen J, Bleijenberg G, Van Riel P. Physical and psychosocial correlates of severe fatigue in rheumatoid arthritis. Rheumatology. 2010:keq043
Løppenthin K, Esbensen BA, Østergaard M, Jennum P, Tolver A, Aadahl M, Thomsen T, Midtgaard J (2015) Physical activity and the association with fatigue and sleep in Danish patients with rheumatoid arthritis. Rheumatol Int 35:1655–1664
Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO (2005) Exercise treatment for depression: efficacy and dose response. Am J Prev Med 28:1–8
Nicassio PM, Ormseth SR, Kay M, Custodio M, Irwin MR, Olmstead R, Weisman MH (2012) The contribution of pain and depression to self-reported sleep disturbance in patients with rheumatoid arthritis. Pain 153:107–112
Espie CA (1993) ABC of sleep disorders. Practical management of insomnia: behavioural and cognitive techniques. BMJ. Br Med J 306:509
Buman MP, Hekler EB, Bliwise DL, King AC (2011) Moderators and mediators of exercise-induced objective sleep improvements in midlife and older adults with sleep complaints. Health Psychol 30:579
Cramp F, Hewlett S, Almeida C et al (2013) Non-pharmacological interventions for fatigue in rheumatoid arthritis. Cochrane Database Syst Rev 8:CD008322
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151:264–269
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS. The American Rheumatism Association (1988) 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO, Birnbaum NS, Burmester GR, Bykerk VP, Cohen MD (2010) 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 62:2569–2581
Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions. Wiley, Chichester
Ryan R, Hill S, Prictor M, McKenzie J (2013) Cochrane Consumers and Communication Review Group. Study quality guide. http://cccrg.cochrane.org/author-resources
Wells GA, Shea B, O’connell D, Peterson JEA, Welch V, Losos M, Tugwell P (2000) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute
Ward L, Stebbings S, Athens J, Cherkin D, Baxter GD (2014) Yoga for pain and sleep quality in rheumatoid arthritis: A pilot randomized controlled trial. J Alternat Complement Med 20:A87–A
Hafström I, Hallengren M (2003) Physiotherapy in subtropic climate improves functional capacity and health-related quality of life in Swedish patients with rheumatoid arthritis and spondylarthropathies still after 6 months. Scand J Rheumatol 32:108–113
Evans S, Moieni M, Lung K, Tsao J, Sternlieb B, Taylor M, Zeltzer L (2013) Impact of iyengar yoga on quality of life in young women with rheumatoid arthritis. Clin J Pain 29:988
McManus KM, Visker JD, Cox CC (2015) Effect of an arthritis foundation exercise program on sleep quality/sleep disturbance in seniors with rheumatoid arthritis: a pilot study. Activ Adapt Aging 39:56–63
Durcan L, Wilson F, Cunnane G (2014) The effect of exercise on sleep and fatigue in rheumatoid arthritis: a randomized controlled study. J Rheumatol 41:1966–1973
Alamanos Y, Voulgari PV, Drosos AA (2006) Incidence and prevalence of rheumatoid arthritis, based on the 1987 American College of Rheumatology criteria: a systematic review. Semin Arthritis Rheum 36:182–188
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213
Buysse DJ, Reynolds CF, Monk TH, Hoch CC (1991) Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI). Sleep 14:331–338
Berger AM, Lockhart K, Agrawal S (2009) Variability of patterns of fatigue and quality of life over time based on different breast cancer adjuvant chemotherapy regimens: publisher
Johnson DA, Orr WC, Crawley JA, Traxler B, McCullough J, Brown KA, Roth T (2005) Effect of esomeprazole on nighttime heartburn and sleep quality in patients with GERD: a randomized, placebo-controlled trial. Am J Gastroenterol 100:1914–1922
Cakirbay H, Bilici M, Kavakçi Ö, Cebi A, Güler M, Tan Ü (2004) Sleep quality and immune functions in rheumatoid arthritis patients with and without major depression. Int J Neurosci 114:245–256
Hunt SM, McKenna SP, McEwen J, Williams J, Papp E (1981) The Nottingham Health Profile: subjective health status and medical consultations. Social science & medicine part a: medical psychology & medical. Sociology 15:221–229
Wiklund I, Romanus B, Hunt SM (1988) Self-assessed disability in patients with arthrosis of the hip joint: reliability of the Swedish version of the Nottingham Health Profile. Int Disabil Stud 010:159–163
Bastien CH, Vallières A, Morin CM (2001) Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med 2:297–307
Currie SR, Wilson KG, Curran D (2002) Clinical significance and predictors of treatment response to cognitive-behavior therapy for insomnia secondary to chronic pain. J Behav Med 25:135–153
Abad VC, Sarinas PSA, Guilleminault C (2008) Sleep and rheumatologic disorders. Sleep Med Rev 12:211–228
Wolfe F, Michaud K, Li T (2006) Sleep disturbance in patients with rheumatoid arthritis: evaluation by medical outcomes study and visual analog sleep scales. J Rheumatol 33:1942–1951
Omachi TA (2011) Measures of sleep in rheumatologic diseases: Epworth Sleepiness Scale (ESS), Functional Outcome of Sleep Questionnaire (FOSQ), Insomnia Severity Index (ISI), and Pittsburgh Sleep Quality Index (PSQI). Arthritis Care Res 2011;63:S287–S96
Callahan LF, Mielenz T, Freburger J, Shreffler J, Hootman J, Brady T, Buysse K, Schwartz T (2008) A randomized controlled trial of the people with arthritis can exercise program: symptoms, function, physical activity, and psychosocial outcomes. Arthritis Care Res 59:92–101
Kirwan JR, Boonen A, Harrison MJ, Hewlett SE, Wells GA, Singh JA, Furst DE, Dworkin RH (2011) OMERACT 10 Patient Perspective Virtual Campus: valuing health; measuring outcomes in rheumatoid arthritis fatigue, RA sleep, arthroplasty, and systemic sclerosis; and clinical significance of changes in health. J Rheumatol 38:1728–1734
Livingstone MBE, Robson PJ, Wallace JMW, McKinley MC (2003) How active are we? Levels of routine physical activity in children and adults. Proc Nutr Soc 62:681–701
Smith MT, Wegener ST (2003) Measures of sleep: the insomnia severity index, medical outcomes study (MOS) sleep scale, Pittsburgh sleep diary (PSD), and Pittsburgh sleep quality index (PSQI). Arthritis Care Res 49:S184–S196
Mainio A, Hakko H, Niemelä A, Koivukangas J, Räsänen P (2013) Insomnia among brain tumor patients: a population-based prospective study of tumor patients in northern Finland. J Psychosoc Oncol 31:507–516
Santos AAd, Mansano-Schlosser TCdS, Ceolim MF, Pavarini SCI (2013) Sono, fragilidade e cognição: estudo multicêntrico com idosos brasileiros. Rev Bras Enferm 66(3):351–357
Hoddes E, Zarcone V, Smythe H, Phillips R, Dement WC (1973) Quantification of sleepiness: a new approach. Psychophysiology 10:431–436
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545.
De Jong Z, Munneke M, Jansen LM, Ronday K, Van Schaardenburg DJ, Brand R, Van Den Ende CHM, Vlieland T, Zuijderduin WM, Hazes JMW (2004) Differences between participants and nonparticipants in an exercise trial for adults with rheumatoid arthritis. Arthritis Care Res 51:593–600
Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, Macera CA, Castaneda-Sceppa C (2007) Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation 116:1094
Brosseau L, Wells GA, Tugwell P, Egan M, Dubouloz C-J, Casimiro L, Robinson VA, Pelland L, McGowan J, Bell M (2004) Ottawa Panel evidence-based clinical practice guidelines for therapeutic exercises in the management of rheumatoid arthritis in adults. Phys Ther 84:934–972
Caspersen CJ, Powell KE, Christenson GM (1985) Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep 100:126
Stenström CH, Minor MA (2003) Evidence for the benefit of aerobic and strengthening exercise in rheumatoid arthritis. Arthritis Care Res 49:428–434
de Jong Z, Vlieland TPMV (2005) Safety of exercise in patients with rheumatoid arthritis. Curr Opin Rheumatol 17:177–182
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Funding
Sean McKenna reports receipt of an Irish Research Council (IRC) scholarship (GOIPG201658), during the conduct and writing up of this review.
Conflict of interest
All authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
McKenna, S., Donnelly, A., Fraser, A. et al. Does exercise impact on sleep for people who have rheumatoid arthritis? A systematic review. Rheumatol Int 37, 963–974 (2017). https://doi.org/10.1007/s00296-017-3681-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-017-3681-x