Abstract
This study aims to estimate the prevalence of serositis and identify risk factors for serositis in a large cohort of systemic lupus erythematosus (SLE) patients. A cross-sectional study was conducted based on the medical records of patients hospitalized with SLE at the First Affiliated Hospital of Anhui Medical University and Anhui Provincial Hospital. Patients were diagnosed with serositis when they presented with symptoms and signs of pleuritis or/and pericarditis. We explored factors associated with the generation and quantity of serositis by using binary and ordinal logistic regression analysis. Among the 1668 lupus patients, 298 have serositis. Active lupus disease, fever (≥38 °C) and high D-dimer were all significantly associated with the generation and quantity of serositis. Male gender was independent significant risk factor for pleuritis but not for pericarditis, while low complement C4 and high erythrocyte sedimentation rate (ESR) were risk factors for pericarditis rather than for pleuritis. The possible prevalence of serositis in patients with SLE was 17.9%. The significant associations of active lupus disease, fever (≥38 °C) and high D-dimer with serositis suggest that higher disease activity and hypercoagulability may both contribute to the generation and development of serositis in SLE. The risk factors for pleuritis and pericarditis in SLE are similar but not identical.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is one of the common autoimmune diseases that can affect almost all organs of the body. Predominant manifestations include arthritis, rash, renal and nervous system involvement [1]. Serositis, which refers to inflammation of serous membranes, does occur in SLE and may be a significant cause of morbidity. In light of the 1997 revised American College of Rheumatology (ACR) criteria, serositis refers either to pleuritis or to pericarditis [2].
The prevalence of serositis in SLE varies depending on definitions of disease used, the different diagnostic approaches, the patient’s selection criteria and number of patients involved. A study including 50 SLE patients and 50 age- and sex-matched control subjects found that 54% patients had pericardial effusion and this prevalence was significantly higher than that in control subjects [3]. Another study of 2104 SLE patients reported 16% patients with serositis as a component, which was found to have significant association with the presence of nephropathy, interstitial lung diseases, pulmonary hypertension, hypocomplementemia, leucopenia, thrombocytopenia, elevated anti-double-stranded DNA (anti-dsDNA) antibodies and active disease [4].
An important aim in clinical evaluation of patients is to recognize those at risk to develop disease manifestations, with the goal of precluding irreversible organ and tissue damage before they occur. The symptom of lupus serositis ranges from pleuritic pain and/or pericardial friction murmur to the life-threatening consequences of massive pleural effusion and/or congestive heart failure [5,6,7]. In this study, we set out to (1) determine the prevalence of serositis in a SLE patient cohort; (2) find the risk factors for occurrence of serositis; and (3) test whether the common risk factors for occurrence of pleuritis and pericarditis were associated with the quantity of serositis.
Patients and methods
Study’s design
A cross-sectional study.
Patient recruitment
The protocol for our study was consistent with the provisions of the World Medical Association Declaration of Helsinki, and informed consent was obtained from each subject before enrollment. This study was conducted with the approval of the ethics committee of Anhui Medical University. We collected the medical records of patients hospitalized with SLE at the First Affiliated Hospital of Anhui Medical University and Anhui Provincial Hospital. All patients fulfilled at least 4 of the SLE classification criteria of the ACR [8]. Collection of data was carried out from January 2011 to December 2015.
Definition of pleuritis, pericarditis and serositis
Patients were diagnosed with serositis when they presented with symptoms and signs of pleuritis or/and pericarditis. Pleuritis was diagnosed when any of the following symptoms were present: typical pleuritic chest pain, pleural rub, radiological evidence (such as chest X-ray or CT scan) or pleurocentesis and laboratory examinations of pleural effusion. Pericarditis was diagnosed when any of the following were detected: typical precordial sharp pain, pericardial rub, electrocardiographic abnormalities, evidence of pericardial effusion on echocardiographic examination or pericardiocentesis and laboratory examinations of pericardial effusion. The diagnosis of lupus-associated serositis was made by exclusion of malignant, thromboembolic and transudative causes such as hypoalbuminemia and heart failure [9]. Moreover, to be considered as non-infectious lupus-related serositis, the clinical records were further reviewed to exclude cases due to tuberculosis, viral and bacterial infections [10]. With these criteria, a retrospective cohort of 1766 SLE patients was recruited. Ninety-eight patients were excluded for missing or incomplete case notes. A final sample of 1668 SLE patients contributed to the analyses.
Study variables
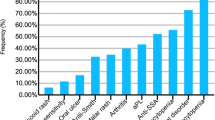
Clinical manifestations of SLE patients, including lupus nephritis, skin rash, alopecia, oral ulcers, neuropsychiatric symptoms, arthritis, myositis, fever (≥38 °C) and vasculitis, were obtained from the medical records. Laboratory abnormalities, including thrombocytopenia (<100 × 109/L), leukopenia (<4.0 × 109/L), anti-Sm, anti-SSA/Ro, anti-SSB/La, anti-RNP, anti-ribosomal RNP (anti-Rib P), anti-dsDNA, low C3 (<0.85 mg/mL), low C4 (<0.12 mg/mL), high erythrocyte sedimentation rate (ESR) (>20 mm/h), high D-dimer (>0.5 ug/mL) and high fibrinogen (>4.0 mg/ml), were also retrieved. SLE disease activity was evaluated by SLE Disease Activity Index (SLEDAI) score [11]. Active lupus disease was defined as SLEDAI score >8. Additionally, data on use of corticosteroids or immunosuppressive drugs (use in the past month or not) were obtained by medical record review.
Statistical analysis
A case–control approach was used to compare parameters between disease and non-disease groups. Age and disease duration were dichotomized at the median value. Categorical variables were summarized as frequency (percentage). Comparison of each variable between different groups was evaluated using the Chi-square test or Fisher’s exact test. Factors with p values <0.05 in the univariate analyses were investigated further using binary logistic regression analysis; results are presented as odds ratio (OR) along with their 95% confidence intervals (CI).
Next, we investigated the association between the variables, which were the common risk factors for occurrence of pleuritis and pericarditis, with the quantity of serositis. For this analysis, we categorized outcome as (1) ‘A’ (if the patients have neither pleuritis nor pericarditis); (2) ‘B’ (if the patients have either pleuritis or pericarditis) and (3) ‘C’ (if the patients have both pleuritis and pericarditis). Ordinal logistic regression models tested the relation of the risk factors with the odds of having multi-symptom disease.
To test the robustness of our findings, ordinal logistic regression models were further adjusted for demographic variables, including age, sex and disease duration. However, because this did not change the results appreciably, only the results of analyses without adjusting these variables were described below. p value <0.05 was considered statistically significant. All statistical analyses were performed using SPSS 13.0 (Chicago, Illinois, USA).
Results
Serositis
The majority of the cohort was female (n = 1526; 91.5%). The median age was 36 years. The median disease duration for SLE was 1.5 years. Among the 1668 lupus patients in this study, 298 have serositis; the prevalence was 17.9%. As shown in Table 1, patients with disease duration <1.5 years were more likely to have serositis than those with a longer disease course (p = 0.009), while there was no significant difference in age or gender between SLE patients with serositis versus those without serositis.
Clinical characteristics and laboratory findings are compared between patients with serositis and patients without this feature. The results indicated that lupus nephritis and fever (≥38 °C) were significantly associated with serositis (all p < 0.050). Moreover, rates of anti-Sm, anti-dsDNA, thrombocytopenia, low C3, low C4, high ESR, high D-dimer and high fibrinogen were significantly higher in the patients with serositis (all p < 0.050). However, rates of other clinical manifestations and laboratory findings were not significantly different between the groups (Tables 2, 3). Associations of lupus activity and drug use with serositis were also analyzed. As shown in Table 4, the presence of active lupus disease was significantly higher in the patients with serositis (p < 0.001); in contrast, rate of use of corticosteroids or immunosuppressive drugs was significantly lower (p = 0.002). Finally, binary logistic regression analysis revealed that fever (≥38 °C), active lupus disease, high D-dimer, low C4 and high ESR were independent significant risk factors for serositis (all p < 0.050) (Table 5).
Pleuritis
Among the 1668 lupus patients, 233 patients have pleuritis; the prevalence was 14.0%. Compared with female, male patients were more likely to have pleuritis (p = 0.020). In contrast, there was no significant difference in age or disease duration between SLE patients with pleuritis versus those without pleuritis (Table 1).
Clinical characteristics and laboratory findings are compared between patients with pleuritis and patients without this feature. The results indicated that lupus nephritis, fever (≥38 °C) and alopecia were significantly associated with pleuritis (all p < 0.050). Moreover, rates of anti-dsDNA, thrombocytopenia, low C3, low C4, high ESR, high D-dimer and high fibrinogen were significantly higher in the patients with pleuritis (all p < 0.050). However, rates of other clinical manifestations and laboratory findings were not significantly different between the groups (Tables 2, 3). Associations of lupus activity and drug use with pleuritis were also analyzed. As shown in Table 4, the presence of active lupus disease was significantly higher in the patients with pleuritis (p < 0.001); in contrast, rate of use of corticosteroids or immunosuppressive drugs was significantly lower (p = 0.025). Finally, binary logistic regression analysis revealed that fever (≥38 °C), active lupus disease and high D-dimer and male gender were independent significant risk factors for pleuritis (all p < 0.050) (Table 5).
Pericarditis
Among the 1668 lupus patients, 161 have pericarditis; the prevalence was 9.7%. Patients with age <36 years were more likely to have pericarditis than those with age ≥36 years (p = 0.009). In addition, patients with disease duration <1.5 years were more prone to have pericarditis than those with a longer disease course (p = 0.009). In contrast, there was no significant difference in gender between SLE patients with pericarditis versus those without pericarditis (Table 1).
Clinical characteristics and laboratory findings are compared between patients with pericarditis and patients without this feature. The results indicated that fever (≥38 °C), alopecia and myositis were significantly associated with pericarditis (all p < 0.05). Moreover, rates of anti-Sm, anti-RNP, anti-dsDNA, thrombocytopenia, low C3, low C4, high ESR, high D-dimer and high fibrinogen were significantly higher in the patients with pericarditis (all p < 0.050). However, rates of other clinical manifestations and laboratory findings were not significantly different between the groups (Tables 2, 3). Associations of lupus activity and drug use with pericarditis were also analyzed. As shown in Table 4, the presence of active lupus disease was significantly higher in the patients with pericarditis (p < 0.001); in contrast, rate of use of corticosteroids or immunosuppressive drugs was significantly lower (p = 0.002). Finally, binary logistic regression analysis revealed that fever (≥38 °C), active lupus disease, high D-dimer, low C4 and high ESR were independent significant risk factors for pericarditis (all p < 0.050) (Table 5).
Association between fever (≥38 °C), active lupus disease and high D-dimer with the quantity of serositis.
For this analysis, we categorized patients as ‘A’, ‘B’ and ‘C,’ as discussed in the ‘Patients and methods’ section. Occurrence of serositis only at only one site (pleura or pericardium) was found in 202 (12.1%) patients. Simultaneously, occurrence of serositis at two sites (pleura or pericardium) was present in 96 (5.7%) patients. Ordinal logistic regression analysis found that fever (≥38 °C), active lupus disease and high D-dimer were all significantly associated with the quantity of serositis (p = 0.003 for fever, p < 0.001 for active lupus disease and p < 0.001 for high D-dimer) (Table 6).
Discussion
In our study, the point prevalence of serositis in the patients with SLE was 17.9%. This rate is in accordance with recent data from mainland Chinese SLE patients [4]. By contrast, it is lower than the prevalence reported in Hong Kong SLE patients [3]. Because of the retrospective nature of the study, we have tried to enhance the validity of the results through collecting the medical records of lupus patients who have been hospitalized in department of rheumatology, which ensured the reasons for hospital admission were related to SLE. Moreover, in general, medical records from patients in inpatient settings were more detailed than that from patients in outpatient settings. Therefore, it is likely that our study reflects the prevalence rate better than the previous studies.
Among the connective tissue diseases, SLE is the most important cause of serositis. Identifying a subgroup of patients with SLE at higher risk of serositis provides the opportunity for early intervention. We found that active lupus disease was significantly associated with serositis. In line with this result, Li et al. [12] and Zhao et al. [4] reported that the presence of serositis was significantly more frequent in active SLE than in inactive SLE. In addition, hypocomplementemia and increased ESR, which are two well-recognized markers for disease activity, were associated with serositis in the present study. Taken together, all of these findings support that active SLE is an indicator of serositis.
In addition to the reported active lupus disease, we note that high D-dimer was related to risk of serositis. This finding indicates the role of hypercoagulability as a mechanism in the pathogenesis of serositis in SLE. This is in keeping with results from previous studies involving experimental as well as clinical interventions. For example, blockade of pleural hypercoagulability by administration of intrapleural heparin in rabbits with tetracycline (TCN)-induced pleuritis alleviates severity of disease, which associated with reduced visceral-parietal adhesions [13, 14]. In addition, the clinical efficacy of fibrinolytic agents demonstrates fibrin deposition in the human pleural compartment [15, 16]. Thus, we suggest that lupus patients experiencing a disease flare should be screened for serositis, especially if they also have high D-dimer.
We proved that the fever was an independent risk factor. This is in line with another study, which has reported the case of SLE pericarditis presenting as fevers of unknown origin in an adult [17]. Future investigations are required to determine the exact mechanism of fever in the pathogenesis of SLE-associated serositis.
One interesting finding from this study was the fact that male gender was found to be a risk factor for pleuritis, but not for pericarditis, while low C4 and high ESR were independent risk factors for pericarditis rather than for pleuritis. Although serositis refers either to pleuritis or to pericarditis in SLE patients, significant differences between the two diseases should not be ignored.
Another intrigued finding was that the presence of fever, active lupus activity and high D-dimer were proved as indicators of the quantity of the SLE-associated serositis. It is well known that the symptom of SLE-associated serositis ranges from pleuritic pain and/or pericardial friction murmur to the life-threatening consequences of massive pleural effusion and/or congestive heart failure. Although treatment with nonsteroidal anti-inflammatory drugs (NSAID) may be effective in mild cases [5], we suggest that more aggressive immunosuppressive therapies combined with anticoagulant drugs might be considered in complex multi-symptom cases.
The present findings must be interpreted within the context of their potential limitations. First, the cross-sectional design of our study provides insights into associations, but cannot determine causality. Establishing time sequence is requisite to hypothesize causality. Second, in the course of collecting medical records, we found that only about 50% of SLE patients have data on C-reactive protein (CRP). The rest of SLE patients have data on hypersensitive CRP (hsCRP) rather than on CRP. HsCRP and CRP, while similar to each other, they are biologically different. Thus, we could not examine the relationship between CRP and serositis in this study. Third, serositis is one item that contributes to the SLEDAI score of disease activity. When including the SLEDAI score of disease activity among the tested risk factors for serositis, this can pose a problem of circularity. However, when we subtracted the SLEDAI score of serositis from each of the SLEDAI score of the SLE patients with serositis and then tested risk factors for serositis, the results also indicated active lupus disease was significantly associated with serositis. Fourth, for the patients who were diagnosed without serositis in our study, the diagnosis partly comes from clinical practice. Further researches are required to demonstrate our findings. Finally, the generalizability of the findings in the present study may be limited given that all lupus patients are Chinese.
In summary, serositis is not uncommon in SLE patients. Risk factors, including fever, active lupus disease and high D-dimer, were associated with the generation and quantity of SLE-associated serositis. The risk factors for pleuritis and pericarditis in SLE are similar but not identical.
References
Liang Y, Xu WD, Peng H, Pan HF, Ye DQ (2014) SOCS signaling in autoimmune diseases: molecular mechanisms and therapeutic implications. Eur J Immunol 44:1265–1275
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725
Crozier IG, Li E, Milne MJ, Nicholls MG (1990) Cardiac involvement in systemic lupus erythematosus detected by echocardiography. Am J Cardiol 65:1145–1148
Zhao J, Bai W, Zhu P et al (2016) Chinese SLE Treatment and Research group (CSTAR) registry VII: prevalence and clinical significance of serositis in Chinese patients with systemic lupus erythematosus. Lupus 25:652–657
Wang DY (2002) Diagnosis and management of lupus pleuritis. Curr Opin Pulm Med 8:312–316
Weich HS, Burgess LJ, Reuter H, Brice EA, Doubell AF (2005) Large pericardial effusions due to systemic lupus erythematosus: a report of eight cases. Lupus 14:450–457
Clarke A (2004) Proposed modifications to 1982 ACR classification criteria for systemic lupus erythematosus: serositis criterion. Lupus 13:855–856
Tan EM, Cohen AS, Fries JF et al (1982) The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25:1271–1277
Man BL, Mok CC (2005) Serositis related to systemic lupus erythematosus: prevalence and outcome. Lupus 14:822–826
Ngandeu MS, Ndobo P, Gabay C (2009) Non-infectious lupus pericarditis: a retrospective hospital-based observation in Yaoundé-Cameroon. Clin Rheumatol 28:465–468
Bombardier C, Gladman DD, Urowitz MB, Caron D, Chang CH (1992) Derivation of the SLEDAI. A disease activity index for lupus patients. The committee on prognosis studies in SLE. Arthritis Rheum 35:630–640
Li LH, Pan HF, Li WX, Li XP, Xu JH, Ye DQ (2009) Study on clinical features and complications with systemic lupus erythematosus (SLE) activity in Chinese Han population. Clin Rheumatol 28:1301–1307
Glauser FL, Otis PT, Levine RI, Smith WR (1976) Coagulation factors and fibrinogen in pleural effusions. Respiration 33:396–402
Strange C, Baumann MH, Sahn S, Idell S (1995) Effects of intrapleural heparin or urokinase on the extent of tetracycline-induced pleural disease. Am J Crit Care Med 151:508–515
Idell S, Girard W, Koenig K, McLarty J, Fair DS (1991) Abnormalities of pathways of fibrin turnover in the human pleural space. Am Rev Respir Dis 144:187–194
Tillet WS, Sherry S, Read CT (1951) Use of streptokinase-streptodornase in treatment of postpneumonic empyema. J Thorac Surg 21:275–297
Petelin A, Johnson DH, Cunha BA (2013) Fever of unknown origin (FUO) due to systemic lupus erythematosus (SLE) presenting as pericarditis. Heart Lung 42:152–153
Acknowledgements
The authors thank all the investigators and study coordinators from every participating center for their invaluable cooperation as well as all the patients who participated in this study.
Funding
This work was supported by grants from the National Natural Science Foundation of China (81611130222).
Author contribution
All authors contributed to: (1) conception and design or acquisition of data or analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content; and (3) final approval of the version to be published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical approval
This study was conducted with the approval of the ethics committee of Anhui Medical University and according to the Declaration of Helsinki principles.
Humans rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Liang, Y., Leng, RX., Pan, HF. et al. The prevalence and risk factors for serositis in patients with systemic lupus erythematosus: a cross-sectional study. Rheumatol Int 37, 305–311 (2017). https://doi.org/10.1007/s00296-016-3630-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-016-3630-0