Abstract
The objective of the study was to investigate the frequency of traditional risk factors for the cardiovascular (CV) disease, to calculate the Systematic COronary Risk Evaluation (SCORE) for CV-related mortality in Danish patients with psoriatic arthritis (PsA) and ankylosing spondylitis (AS), and to compare with results from patients with rheumatoid arthritis (RA) from the same settlement. All PsA and AS patients aged 18–85 years from one outpatient clinic were invited. A rheumatology nurse conducted 30-min screening consultation, preceded by a lipid and glucose profile. High SCORE risk led to recommendation of follow-up by general practitioners. Multiple and logistic regression analyses, adjusted for age and gender, were performed, to compare risk factors and risk SCOREs. Participants were 116 AS (29.3% female) and 170 PsA (54.7% female). AS had opposed PsA patients’ lower 10-year risk SCOREs of CV mortality than RA patients: AS versus RA coefficient −0.47 (confidence interval (CI) 95%: −0.84 to −0.) and PsA versus RA −0.14, (−0.43–0.16). Women with PsA and AS had increased waistline compared to women with RA [PsA vs. RA 7.94 (4.51–11.38); AS versus RA 6.67 (1.17–12.17)], and an increased prevalence of hypertension was seen in AS versus RA patients [1.87 (1.15–3.05)]. Traditional, modifiable CV risk factors were present in PsA and AS patients. AS but not PsA patients had an estimated lower 10-year risk of CV mortality than RA patients, according to the SCORE model adjusted for age and gender.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2010, an expert European League Against Rheumatism (EULAR) panel published evidence-based recommendations for cardiovascular (CV) risk management in patients with inflammatory arthritis. This was updated in October 2016 [1, 2]. Systematic risk assessment is recommended in patients with rheumatoid arthritis (RA) and in patients with psoriatic arthritis (PsA) and ankylosing spondylitis (AS), despite the fact that the evidence was not as clear as for patients with RA [3–7]. Any identified risks should be managed according to local guidelines. The European SCORE (Systematic COronary Risk Evaluation) model [8] should be used as the risk assessment tool, unless a different tool was recommended in national guidelines. The SCORE is a visualized algorithm calculating 10-year risk of CV death, based on the patient’s blood pressure, smoking habits, cholesterol-level, gender and age. In RA, a modified SCORE adjusts for the expected increased risk of CV mortality by a factor 1.5, when two out of three specific surrogates for complicated disease are present (disease duration ≥10 years, rheumatoid factor (IgM-RF) or anti-cyclic citrullinated peptide positivity and specific extra-articular manifestations) [2]. The recent EULAR recommendations regarding CV risk management from October 2016 advise to multiply any RA patient’s risk SCORE by 1.5 [1], but in this study we used the 2010 criteria [2]. The SCORE was not modified in patients with PsA and AS in accordance with the past and present EULAR recommendations [1, 2]. The 2010 EULAR recommendations for CV risk management were followed by a national guideline from the Danish Rheumatology Association in 2012 [9]. Furthermore, local guidelines for CV screening of outpatients with AS and PsA were developed based on the EULAR recommendations from 2010 [2], other national guidelines [2, 10–13] and experiences from our CV screening of RA patients [11].
The prevalence of CV risk factors in patients with RA, AS and PsA has been described by Mok et al. [14] in a Hong Kong population and by Rollefstad et al. [15] in a Norwegian outpatient population in 2013. Gulati et al. [16] compared a Norwegian PsA population to the general population. Standardized mortality ratios in AS compared to healthy controls have been found to be significantly increased in recent studies (SMR 1.6–1.9) due to infection and CV death [14, 17, 18]. In PsA, the risk of CV disease events is increased, but the SMRs are ambiguous (0.8–1.8) [14, 19, 20]. However, the documentation of CV risk factor distribution is still sparse for AS and PsA patients.
The aim of this study was to describe the frequency of traditional risk factors for the development of CV disease and the risk SCORE for CV death in Danish patients with PsA or AS, and to compare these results to previously published findings from systematic screening for CV risk [9] in patients with RA from the same outpatient clinic.
Methods
The patients were offered a 30-min CV screening consultation with a rheumatology specialist nurse in addition to the patients’ regular follow-up visits. The nurses, supervised by the principal investigator, were experienced in the use of CV screening, because they had used the screening procedure since 2011 for RA patients.
Participants
All outpatients at King Christian X Hospital for Rheumatic Diseases, Graasten, Denmark, 18–85 years of age, were diagnosed by a rheumatologist either following the CASPAR (ClASsification criteria for Psoriatic ARthritis) group criteria for PsA [21] or the New York criteria for AS [22]. Regardless of disease duration and other parameters, they were invited consecutively based on birth month to participate in the screening consultations as part of normal clinical practice. Thus, no informed consent was obtained.
In order to compare the results from patients with PsA and AS to our population of RA patients, we used data from our previous study on patients with RA [11]. The RA population included 836 patients from the same outpatient clinic. The patients had participated in similar nurse-led screening for CV risk between September 2011 and November 2012. For this population, we calculated the modified SCORE (mSCORE) in addition to the SCORE as recommended in the EULAR recommendations for cardiovascular risk management from 2010 [2].
Study design
We used a cross-sectional design, as in our previous study [11], where the screening method is described in detail. Before the screening consultation, a full lipid profile (total, high-density lipoprotein (HDL) and low-density lipoprotein (LDL) cholesterol and triglycerides) and fasting blood glucose level or HbA1c was taken. The nurse-led screening consultation elicited information about known CV disease, hypertension or diabetes mellitus (DM), prescribed medications, habits of smoking (described as: never, former or present smoker), physical activity apart from normal daily activities (described as: less or ≥5 times a week) and alcohol usage (below or above national recommendations of maximum 7/14 units per week for females/males, respectively). In addition, height, weight, waistline and blood pressure were measured and body mass index (BMI) was calculated. Waistline was measured 2 cm above the patient’s umbilicus (midway between the lower rib margin and the iliac crest) [11, 23]. Blood pressure (BP) was measured while the patient was sitting in a chair and after at least 5-min rest [13]. If the patient’s blood pressure exceeded the national recommendations by 5 mmHg, a total of four measures (two on each arm) were performed and the mean of the last two measures was used [11]. Information about gender, age, systolic blood pressure, total-/HDL-cholesterol ratio and smoking habits were used to calculate the SCORE [8]. The outcome is the risk of cardiovascular death in 10 years divided into three groups: low/moderate risk (<5% risk of cardiovascular death over 10 years), high risk (≥5% and <10%) and very high risk (>10%) [8]. The model is not applicable to patients with DM and cardiovascular disease (CVD) [8]. The SCORE was not modified in patients with PsA and AS, as it was in patients with RA in accordance with the EULAR recommendations [1, 2].
The findings were documented in the patients’ journal and in the national quality database, DANBIO [24]. After the consultation, an electronic copy of the journal note was sent to the patient’s general practitioner (GP). Following a dialogue about the results with the patient, a printout of the entries in DANBIO was offered to the patient, together with relevant pamphlets.
Statistical analysis
Descriptive statistics of baseline characteristics and crude data for the spread of risk factors are reported with mean and standard deviation (SD), mean and 25/75 percentiles or median and interquartile range (IQR), as appropriate. Percentages were calculated based on the number of observations available for each variable. As the SCORE model is not applicable for patients with known DM or CVD (7), we performed comparative analyses between diagnoses on the subgroup with no known DM or CVD. Diagnoses were created as dummy variables. Multiple regression analyses were used to test for significant differences in continuous variables and risk SCOREs between diagnoses (PsA or AS vs. RA as the reference group). Results are reported with coefficients, confidence intervals and p values. Multinominal logistic regression analyses were used to test for significant differences between diagnoses regarding the frequency of comorbidities (hypertension, DM and CVD) and in binary risk factors in the subgroup without known CVD or DM. Results are reported with coefficients or odds ratios, confidence intervals and p values. The analyses were adjusted for age and gender, because of great variance in the patient groups in these variables. For differences between diagnoses in BMI, we report the gender-specific results adjusted for age. The significance level was set at 95%. STATA V.13.0 was used to perform all the analyses.
Results
In total, 286 patients with PsA or AS were screened from March 2012 through September 2013; 170 with PsA (54.7% female) and 116 with AS (29.3% female). Baseline characteristics and known comorbidities are presented in Table 1, together with previously published results from the RA population [11]. Almost all patients were Caucasians.
Reasons given for declining participation were severe disability or comorbidities, an ill spouse, or that it was difficult for them to attend due to transportation or work-related issues. Some patients felt that their GP already took care of the content in the screening consultation or that they did not want to discuss lifestyle issues. Approximately 10% of the patients declined to participate, but this information was only registered the first year after implementation in clinical practice.
After adjusting for age and gender, the logistic regression analyses revealed an almost doubled odds ratio of hypertension in AS versus RA patients (odds ratio (OR), [95% confidence interval (CI), p value)] [1.87, (1.15; 3.05, p = 0.012)] and a non-significant tendency towards higher odds for having DM in AS versus RA patients [OR 1.92, (0.92; 4.02, p = 0.084)]. No difference was seen in the odds of CVD in PsA versus RA [OR 1.03, (0.63; 1.69, p = 0.91)] or in AS versus RA [OR 0.82, (0.43; 1.57, p = 0.55)].
The frequency of CV risk factors (crude data) for the entire screened population with PsA and AS is presented in Table 2, including the frequency of CV risk factors in the RA population from the previous study [11].
As the SCORE system does not apply for patients with known CVD or DM, the following results will report the results for the sub-sample with no known CVD or DM only. In Table 3, the results are reported for each diagnostic group according to the nationally recommended limits. Out of the 138 PsA and the 94 AS patients, 7 (5.1%) and 3 (3.2%), respectively, had a fasting glucose ≥7 mM, which indicates undiagnosed DM.
Table 4 shows the results from the regression analyses in the subgroup with no known CVD or DM. The distribution of risk factors is compared in PsA versus RA and AS versus RA and adjusted for age and gender. The first part reports results from multiple regression analyses for the continuous variables, and the second part reports the results from the logistic regression analyses on the binary variables (yes/no to present smoking, alcohol above the recommended limits and exercise less than 5 times a week).
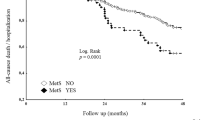
The calculated SCOREs were categorized into three groups according to the level of the risk (low, high or very high risk) [8], and these results are presented in Table 5.
In Table 5, the comparison of the risk SCOREs by multiple regression analysis for AS and PsA patients with the non-modified SCORE for RA patients as the reference group is presented. A significant difference was seen in risk of CV death: AS versus RA [−0.75 (−1.21; −0.28, p = 0.002)] and PsA versus RA [−0.63 (−1.03; −0.23, p = 0.002)]. When adjusting for age and gender, the tendency remained for patients with AS versus RA [−0.47 (−1.30; −0.41), p < 0.001], but for PsA versus RA the difference was no longer significant [−0.14 (−0.43; 0.16), p = 3.666].
When comparing the SCORE for AS and PsA patients with the mSCORE for RA patients and adjusting for age and gender, the coefficients were as follows: AS versus RA patients (−0.85 (−1.30; −0.41), p < 0.001] and PsA versus RA [−0.49 (−0.85; −0.13), p = 0.008].
Discussion
We found that Danish outpatients with AS and PsA had a lower estimated risk of CV mortality in 10 years compared to outpatients with RA, based on the SCORE, but the difference between PsA and RA patients was no longer significant when adjusting for age and gender. When comparing the SCORE for AS and PsA patients with the mSCORE for patients with RA, both patients with AS and PsA had significantly lower estimated risk compared to patients with RA. Significant differences were found in BMI and waistlines. Female patients diagnosed with PsA or AS had a coefficient of 8 and 6.7, respectively, compared to female patients with RA. This difference was not present in the males in these populations.
The data from Rollefstad et al. [15] largely correspond to our results, although their risk SCORES are slightly higher in AS and RA patients, compared to our Danish population (Rollefstad: SCORE ≥ 5%: PsA = 14.3%, AS = 16.4%, RA = 13.6% compared to our study: SCORE ≥ 5%: PsA = 14.1%, AS = 11.9%, RA = 12.6%) [15]. Gulati et al. [16] presented higher amount of very high SCORES in their Norwegian PsA population (SCORE < 5%: 82.6%; SCORE ≥ 5% and ≤ 10%: 3.0%; SCORE ≥ 10%: 14.3%). Furthermore, they found that people with PsA had a higher prevalence of CV risk factors (smoking, hypertension, BMI and triglycerides), compared to controls, but no differences were found in their overall SCOREs.
Even though the risk is estimated to be lower in patients with AS compared to patients with RA, other studies still indicate an increased risk compared to people without AS. In a large population-based cohort study by Essers et al. [25], only women with AS had an increased incidence of ischaemic heart disease, compared to matched controls [hazards ratio (HR) = 1.88, (1.22; 2.90)]. The difference disappeared when adjusting for use of nonsteroidal antiinflammatory drugs (NSAID) [25], a possible surrogate for high disease activity/inflammation. Another study found adjusted HR for vascular death in AS of 1.36 (1.13; 1.65), compared to healthy controls. Men had a significantly higher risk than women, but NSAID-use lowered the risk [5]. In a Hong Kong population, the age- and gender-adjusted standardized mortality rates for patients with PsA, AS and RA were 1.59 (1.16; 2.03), 1.87 (1.61; 2.13) and 1.68 (1.59; 1.77), respectively, when compared to controls [14]. The above-described studies all correspond to the increased CV risk found by Ahlehoff et al. [4] and Haroon et al. [5] in PsA and AS patients, stressing the need for CV screening and CV risk management in patients with PsA and AS as well as in patients with RA. Our results also show high risk SCOREs in especially PsA patients, increasing the evidence, of the presence of modifiable risk factors in these populations.
The prominent significant differences we found between diagnoses in BMI and waistlines are consistent with the results from the studies by Mok et al. [14] and Rollefstad et al., where patients with PsA had higher BMI than patients with RA or AS, but they did not investigate gender differences [15]. This discrepancy in BMI and waistlines between men and women is remarkable and unexplained, and needs further investigation.
The mean non-adjusted values (Table 2) for cholesterol seemed to be equally distributed between the three diagnoses, but when adjusted for age and gender, we found significant differences regarding LDL cholesterol, total cholesterol and triglycerides in the populations (Table 4). Both patients with PsA and AS had an increased risk of high total-cholesterol, compared to patients with RA. Patients with AS had higher LDL cholesterol compared to patients with RA, and for patients with PsA the same tendency (non-significant). Patients with PsA had higher triglycerides than patients with RA, but this was not the case in patients with AS. This may be related to the higher prevalence of obesity and DM in the population with PsA compared to patients with RA. Previous studies only found significant differences in HDL cholesterol [14, 15].
There was no difference in the proportion of patients with alcohol consumption above the national recommendations in the three patient groups. This is in contrast to the findings from other studies, where it was indicated that patients with PsA had higher alcohol consumption, compared to both other arthritis patients and controls from the general population [26, 27]. Possible underestimation of alcohol usage because of the delicate situation of face-to-face reporting is the same in all three patient groups. The lower frequency of alcohol intake in patients with PsA compared to patients with AS in our study could, in part, be related to the use of methotrexate and leflunomide in PsA patients’ treatment, but this is not the case for RA patients, where the treatment strategy is similar to PsA.
The odds for smoking were significantly lower for PsA, compared to RA patients, whereas the difference did not reach a significant level between AS and RA patients. Gulati et al. [16] found that 21.3% of patients with PsA were smokers versus 16.4% in the healthy control group (p = 0.02). In contrast to this, we found fewer smokers among patients with no known CVD or DM and PsA (18.9%), slightly more smokers among patients with AS (23.4%) and (24.5%) smokers among patients with RA [11]. In the general population in the same region (Southern Denmark), the share of smokers was 22.2% in 2010. It can be difficult to compare the results, because of possible differences in the recruitment of patients, but there seems to be more smokers in the Norwegian PsA population, compared to our Danish population. These differences are unexplained.
The strength of our study is the systematic documentation in a national registry for all three patient groups. However, there could still be type II errors, because of a lack of power regarding differences in the distribution of risk factors and type I errors and we did not adjust for multiple comparisons. Moreover, it was not possible to adjust the analyses for possible differences in disease duration, disease activity and medications, as these data were not available. There is also the possibility that the population is selected because it is based on an extra consultation in addition to the regular outpatient consultations and some patients decline to participate. Unfortunately, we were unable to report the exact number of patients who declined to participate as we did not collect this information and could therefore not check for selection bias. We did not have a control group from the general population for comparison, which would have strengthened the study. The limitation in using a cross-sectional design is that the study cannot explain a cause and effect relation regarding the different frequencies of risk factors and risk SCORE. Also the results are only based on Caucasians.
Whether the patients’ actual risk is in agreement with their estimated risk, and whether interventions can help lower the patients’ risk, are all issues that need further investigation in patients with inflammatory arthritis.
Conclusion
AS patients have a slightly lower risk of CV mortality in 10 years than RA patients, according to the SCORE model. Patients with PsA have similar estimated risk SCORE as patients with RA, but lower risk than patients with RA when comparing with the mSCORE for patients with RA. AS patients had a doubled risk of hypertension and a higher risk of increased total and LDL cholesterol, and female AS patients had a higher risk of an increased waistline above the recommended measurements, compared to the RA patients. Patients with PsA had a significantly higher risk for obesity, high fasting glucose, and total and LDL-cholesterol levels, compared to patients with RA.
The results support the decision to implement screening consultations in especially PsA and AS patients, because of the prevalence of multiple modifiable risk factors and a high risk of CV mortality in these patients. The findings can be useful for comparison between hospitals and countries and for evaluation of specific interventions to address these patients risk profiles.
References
Agca R, Heslinga SC, Rollefstad S, Heslinga M, McInnes IB, Peters MJ, Kvien TK, Dougados M, Radner H, Atzeni F, Primdahl J, Sodergren A, Wallberg Jonsson S, van Rompay J, Zabalan C, Pedersen TR, Jacobsson L, de Vlam K, Gonzalez-Gay MA, Semb AG, Kitas GD, Smulders YM, Szekanecz Z, Sattar N, Symmons DP, Nurmohamed MT (2016) EULAR recommendations for cardiovascular disease risk management in patients with rheumatoid arthritis and other forms of inflammatory joint disorders: 2015/2016 update. Ann Rheum Dis. doi:10.1136/annrheumdis-2016-209775
Peters MJ, Symmons DP, McCarey D, Dijkmans BA, Nicola P, Kvien TK, McInnes IB, Haentzschel H, Gonzalez-Gay MA, Provan S, Semb A, Sidiropoulos P, Kitas G, Smulders YM, Soubrier M, Szekanecz Z, Sattar N, Nurmohamed MT (2010) EULAR evidence-based recommendations for cardiovascular risk management in patients with rheumatoid arthritis and other forms of inflammatory arthritis. Ann Rheum Dis 69(2):325–331. doi:10.1136/ard.2009.113696
Jamnitski A, Symmons D, Peters MJ, Sattar N, McInnes I, McIinnes I, Nurmohamed MT (2013) Cardiovascular comorbidities in patients with psoriatic arthritis: a systematic review. Ann Rheum Dis 72(2):211–216. doi:10.1136/annrheumdis-2011-201194
Ahlehoff O, Gislason GH, Charlot M, Jørgensen CH, Lindhardsen J, Olesen JB, Abildstrøm SZ, Skov L, Torp-Pedersen C, Hansen PR (2011) Psoriasis is associated with clinically significant cardiovascular risk: a Danish nationwide cohort study. J Intern Med 270(2):147–157. doi:10.1111/j.1365-2796.2010.02310.x
Haroon NN, Paterson JM, Li P, Inman RD, Haroon N (2015) Patients with ankylosing spondylitis have increased cardiovascular and cerebrovascular mortality: a population-based study. Ann Intern Med 163(6):409–416. doi:10.7326/M14-2470
Wright KA, Crowson CS, Michet CJ, Matteson EL (2015) Time trends in incidence, clinical features, and cardiovascular disease in ankylosing spondylitis over three decades: a population-based study. Arthritis Care Res (Hoboken) 67(6):836–841. doi:10.1002/acr.22512
Ernste FC, Sánchez-Menéndez M, Wilton KM, Crowson CS, Matteson EL, Maradit Kremers H (2015) Cardiovascular risk profile at the onset of psoriatic arthritis: a population-based cohort study. Arthritis Care Res (Hoboken) 67(7):1015–1021. doi:10.1002/acr.22536
Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, De Backer G, De Bacquer D, Ducimetière P, Jousilahti P, Keil U, Njølstad I, Oganov RG, Thomsen T, Tunstall-Pedoe H, Tverdal A, Wedel H, Whincup P, Wilhelmsen L, Graham IM, SCORE project group (2003) Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 24(11):987–1003
Asmussen KH, Steengaard-Pedersen K, Hørslev-Pedersen K et al. (2012) Reumatoid Arthritis - klinisk retningslinje (Rheumatoid Arthritis - clinical guideline). Dansk Reumatologisk selskab (Danish Rheumatology Association). Accessed 20 Mar 2013
Prescott E, Rasmusen H, Gustafsson I (2013) Forebyggelse af hjertesygdom (prevention of heart disease). Dansk kardiologisk selskab (Danish Cardiological Association). Accessed 17 Feb 2014
Primdahl J, Clausen J, Hørslev-Petersen K (2013) Results from systematic screening for cardiovascular risk in outpatients with rheumatoid arthritis in accordance with the EULAR recommendations. Ann Rheum Dis 72(11):1771–1776. doi:10.1136/annrheumdis-2013-203682
Christensen B, Færgemann O, Heebøll-Nielsen Forebyggelse af iskæmisk hjerte-kar-sygdom i almen praksis (prevention of ischemic cardiovascular disease in general practise). Dansk selskab for almen medicin (DSAM) (Danish association for General Practice). Accessed 20 Mar 2013
Bang LECK, Hansen KW et al. (2006) Diagnostisk blodtryksmåling - på døgnbasis, hjemme og i konsultationen. (Diagnostic bloodpressure measurement - at 24-hour basis, at home and in the consultation). Dansk Hypertensions selskab (Danish Hypertension Association). Accessed Mar 2013
Mok CC, Kwok CL, Ho LY, Chan PT, Yip SF (2011) Life expectancy, standardized mortality ratios, and causes of death in six rheumatic diseases in Hong Kong, China. Arthritis Rheum 63(5):1182–1189. doi:10.1002/art.30277
Rollefstad S, Kvien TK, Holme I, Eirheim AS, Pedersen TR, Semb AG (2013) Treatment to lipid targets in patients with inflammatory joint diseases in a preventive cardio-rheuma clinic. Ann Rheum Dis 72(12):1968–1974. doi:10.1136/annrheumdis-2012-202789
Gulati AM, Semb AG, Rollefstad S, Romundstad PR, Kavanaugh A, Gulati S, Haugeberg G, Hoff M (2016) On the HUNT for cardiovascular risk factors and disease in patients with psoriatic arthritis: population-based data from the Nord-Trøndelag health study. Ann Rheum Dis 75(5):819–824. doi:10.1136/annrheumdis-2014-206824
Bakland G, Gran JT, Nossent JC (2011) Increased mortality in ankylosing spondylitis is related to disease activity. Ann Rheum Dis 70(11):1921–1925. doi:10.1136/ard.2011.151191
Exarchou S, Lie E, Lindstrom U, Askling J, Forsblad-d’Elia H, Turesson C, Kristensen LE, Jacobsson LT (2016) Mortality in ankylosing spondylitis: results from a nationwide population-based study. Ann Rheum Dis 75(8):1466–1472. doi:10.1136/annrheumdis-2015-207688
Ogdie A, Yu Y, Haynes K, Love TJ, Maliha S, Jiang Y, Troxel AB, Hennessy S, Kimmel SE, Margolis DJ, Choi H, Mehta NN, Gelfand JM (2015) Risk of major cardiovascular events in patients with psoriatic arthritis, psoriasis and rheumatoid arthritis: a population-based cohort study. Ann Rheum Dis 74(2):326–332. doi:10.1136/annrheumdis-2014-205675
Buckley C, Cavill C, Taylor G, Kay H, Waldron N, Korendowych E, McHugh N (2010) Mortality in psoriatic arthritis—a single-center study from the UK. J Rheumatol 37(10):2141–2144. doi:10.3899/jrheum.100034
Taylor W, Gladman D, Helliwell P, Marchesoni A, Mease P, Mielants H, CASPAR Study Group (2006) Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheum 54(8):2665–2673. doi:10.1002/art.21972
van der Linden S, Valkenburg HA, Cats A (1984) Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum 27(4):361–368
Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, Albus C, Benlian P, Boysen G, Cifkova R, Deaton C, Ebrahim S, Fisher M, Germano G, Hobbs R, Hoes A, Karadeniz S, Mezzani A, Prescott E, Ryden L, Scherer M, Syvänne M, Scholte op Reimer WJ, Vrints C, Wood D, Zamorano JL, Zannad F, (EACPR) EAfCPR, (CPG) ECfPG (2012) European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The fifth joint Task force of the European society of cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur Heart J 33(13):1635–1701. doi:10.1093/eurheartj/ehs092
Hetland ML (2011) DANBIO—powerful research database and electronic patient record. Rheumatology (Oxford) 50(1):69–77. doi:10.1093/rheumatology/keq309
Essers I, Stolwijk C, Boonen A, De Bruin ML, Bazelier MT, de Vries F, van Tubergen A (2014) Ankylosing spondylitis and risk of ischaemic heart disease: a population-based cohort study. Ann Rheum Dis. doi:10.1136/annrheumdis-2014-206147
Tilling L, Townsend S, David J (2006) Methotrexate and hepatic toxicity in rheumatoid arthritis and psoriatic arthritis. Clin Drug Investig 26(2):55–62
Huidekoper AL, van der Woude D, Knevel R, van der Helm-van Mil AH, Cannegieter SC, Rosendaal FR, Kloppenburg M, Huizinga TW (2013) Patients with early arthritis consume less alcohol than controls, regardless of the type of arthritis. Rheumatology (Oxford) 52(9):1701–1707. doi:10.1093/rheumatology/ket212
Acknowledgements
The authors would like to acknowledge the multidisciplinary steering group for the systematic screening (senior consultants Vibeke Ringsdal, head of the secretariat Anette Christensen, head of the department of clinical chemistry Charlotte Drachmann and the outpatient nurses Pia Rhode Rasmussen, Joan Clausen and Kirsten Nørret Hansen). Thank you to Niels Steen Krogh from Zitelab and the DANBIO registry for cooperation in development of the CVR theme as part of a yearly visit. Thank you to Lorna Campbell for assistance in language editing. Funding was provided by Gigtforeningen (DK) (Grant No. R116-A2801).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was funded by a research grant from the Association against Rheumatism (Gigtforeningen; patient organization), Denmark. Author 1 has received financial support from Bristol-Myers Squibb to attend a conference. Authors 2 and 3 have received speaker fees from multiple pharmacological companies, and author 2 has received financial support from multiple different pharmacological companies to attend conferences during the past 10 years.
Ethical approval
The study has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and later amendments. The data used in this study were obtained and entered into a national quality database (DANBIO) as part of daily clinical practice. Thus, permission from a research ethics committee was not required and formal informed consent was not obtained.
Rights and permissions
About this article
Cite this article
Nissen, C.B., Hørslev-Petersen, K. & Primdahl, J. Cardiovascular risk profiles in a hospital-based population of patients with psoriatic arthritis and ankylosing spondylitis: a cross-sectional study. Rheumatol Int 37, 113–120 (2017). https://doi.org/10.1007/s00296-016-3614-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-016-3614-0