Abstract
Multidisciplinary treatments have shown to be effective for fibromyalgia. We report detailed functional outcomes of patients with fibromyalgia who attended a 3-month Multidisciplinary treatment program. The hypothesis was that patients would have increased functional status, physical activity level, and exercise regularity after attending this program. We performed a retrospective analysis of a randomized, simple blinded clinical trial. The inclusion criteria consisted of female sex, a diagnosis of fibromyalgia, age 18–60 and 3–8 years of schooling. Measures from the Fibromyalgia Impact Questionnaire (FIQ) and the COOP/WONCA Functional Health Assessment Charts (WONCA) were obtained before and at the end of the treatment and at 3-, 6-, and 12-month follow-ups. Patients recorded their number of steps per day with pedometers. They performed the six-minute walk test (6 MW) before and after treatment. In total, 155 women participated in the study. Their median (interquartile interval) FIQ score was 68.0 (53.0–77.0) at the beginning of the treatment, and the difference between the Multidisciplinary and Control groups was statistically and clinically significant in all of the measures (except the 6-month follow-up). The WONCA charts showed significant clinical improvements in the Multidisciplinary group, with physical fitness in the normal range across almost all values. In that group, steps/day showed more regularity, and the 6 MW results showed improvement of −33.00 (−59.8 to −8.25) m, and the differences from the Control group were statistically significant. The patients who underwent the Multidisciplinary treatment had improved functional status, physical activity level, and exercise regularity. The functional improvements were maintained 1 year after treatment completion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fibromyalgia (FM) is a chronic syndrome characterized by widespread pain and allodynia, and it is often accompanied by fatigue, affective symptoms, memory problems, and sleep disturbances. Existing data suggest that disturbed central pain processing plays an important role in the syndrome’s pathogenesis [1].
Multidisciplinary treatments have proved effective in reducing the impact and pain level associated with FM [2–6]. However, there is little evidence that these treatments successfully measure functional status [7]. It is defined as an individual’s ability to perform normal daily activities required to meet basic needs, fulfill usual roles, and maintain health and well-being [8]. As the improvement in functional outcomes generated by alleviation of pain and its clinical significance is debated, Marcus et al. [7] called for increased levels of functional evaluation.
Various outcome measures have been proposed to assess function in patients with FM, including the Fibromyalgia Impact Questionnaire (FIQ) [9], which is the most commonly used instrument for this purpose [10]. The distance walked in six minutes (6 MW) has also been validated as a measure of function in patients with FM [11, 12]. The number of steps/day quantified by a pedometer and the physical fitness and daily activities domains of the Dartmouth COOP/WONCA Functional Health Assessment Charts (WONCA) questionnaire have also been used [13, 14].
The American Pain Society highly recommends aerobic exercise as part of a Multidisciplinary treatment for patients with chronic FM [10]. Much research has demonstrated the benefits of exercise, but more effort is needed to motivate patients to continue regular exercise after the intervention, enhancing their adherence to exercise recommendations. Pedometer use is a suitable technique to increase patient motivation and promote adherence [13, 15–17].
This study was designed to supplement previously published data by reporting detailed functional outcomes from patients with FM who attended a 24-session, 3-month Multidisciplinary FM treatment program [5]. The hypothesis of the present study was that patients with FM would increase their functional status, physical activity level, and exercise regularity after this Multidisciplinary treatment program.
Patients and methods
This study is a retrospective analysis of a randomized, simple blinded, clinical trial. The Clinical Research Ethics Committee of the Hospital Universitari Joan XXIII (Tarragona, Spain) approved the study protocol. All subjects were interviewed individually to provide them with details about the nature of the study. All of them signed voluntary consent forms prior to enrollment.
Participants who met the following inclusion criteria were included in the study: female sex, FM diagnosis according to the diagnostic criteria of the American College of Rheumatology [18], age 18–60 and 3–8 years of schooling. The exclusion criteria were: coexistence of another severe chronic pain pathology (e.g., sciatica or complex regional pain syndrome), having been diagnosed with inflammatory rheumatic disease, physical inability to perform the exercises, an open wound, a skin disease, having been under psychiatric and/or psychological treatment within the past 3 years, significant suicidal ideation, cognitive or sensorial deterioration, or a pending disability-related legal resolution.
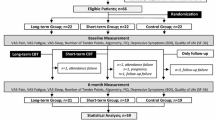
Patients were recruited from consultations with a rheumatologist and treated from September 2008 to March 2010. Consecutive participants who met all of the inclusion criteria and agreed to participate in the study were assigned to conventional pharmacologic treatment or Multidisciplinary treatment groups in a 1:1 ratio in blocks of 32 according to a computer-generated random number table. Of the 460 individuals evaluated, 174 were included in the study. Of these 174 participants, 19 were included in a pilot study, and the study sample consisted of 155 participants (Fig. 1).
Procedures
After a pilot study was conducted to improve the procedures, the refined program was applied, and the rating measurements were collected. Demographic and clinical data were collected, and the measurement instruments were applied before the interventions, with reassessment performed in the week immediately after treatment completion and after a further 3, 6, and 12 months. Although the participants and therapists (i.e., psychologist and physical therapist) could not be blinded to treatment condition, the evaluators (i.e., physician, psychologist, and physical therapist) were blinded to the different treatment conditions.
Treatment conditions
All of the participants received a conventional pharmacologic treatment. In addition, the Multidisciplinary group received 24 physical and cognitive–behavioral therapy (CBT) sessions during two consecutive hours twice weekly in reduced groups of 8 patients (12 weeks). The physical therapy component involved two sessions per week including hydrokinesitherapy and a strength-training program. The CBT program included information about FM, theory of pain perception, cognitive restructuring skills training, CBT for primary insomnia, assertiveness training, goal setting, activity pacing and pleasant activity scheduling training, life values, and relapse prevention. All of them were given a pedometer (Yamax Digi-walker SW-200) to encourage activity and an audio CD to practice Schultz autogenic training at home. These sessions’ contents are specified in Supplementary Appendix A of a previous publication [5]. The Control group received only the pharmacological treatment.
A physiotherapist specifically trained for this program delivered the physical therapy program. A clinical psychologist also specifically trained for this program delivered the CBT program. Both were women and about same age, in their 20s.
Assessment
Baseline measures were obtained before the start of treatment, immediately at the end of the treatment, and at 3-, 6-, and 12-month follow-ups. In all of these examinations, subjects were assessed using the FIQ [9] and the WONCA [14]. Patients received the pedometer at the beginning of the program, and they were asked them to register the number of steps made per day (steps/day) each night. They performed the 6 MW at the beginning and end of the treatment [10].
Main outcomes
FIQ was the primary outcome, and WONCA and 6 MW were the secondary outcomes. In addition, steps/day were recorded during treatment. To analyze the two groups’ homogeneity, we also used the catastrophizing subscale of the Coping Strategies Questionnaire [19], the Medical Outcome Study Sleep Scale [20], and the Hospital Anxiety and Depression Scale (HADS) [21].
The FIQ assesses the impact of FM on a patient’s life [8]; it is a self-administered multidimensional questionnaire designed specifically to assess the functional capacity of patients with FM [22]. FIQ scores range from 0 to 100 (with 0 and 100 indicating the best and worst health, respectively). A cutoff of 14% in total FIQ score was established to represent a clinically significant change [23]. Changes in FM impairment were also evaluated: FIQ scores of >59, 59–39, and <39 represent severe, moderate, and mild impairment, respectively [23]. We used the Spanish version [24].
The WONCA was developed to assess functional status in primary care [14], which includes the following domains: physical fitness, mood, daily activities, social activities, pain, and overall health. Several studies have documented the reliability and validity of the charts employed in this assessment [25]. Each chart consists of one statement followed by five response options illustrated with pictograms (e.g., a smiling or sad face). Each chart is associated with a question related to events from the last 2 weeks. The maximum score indicates the lowest functional status. We used the WONCA in Spanish: the Dartmouth Primary Care Cooperative Information Project/World Organization of National Colleges, Academies, and Academic Associations of General Practice/Family Physicians (COOP/WONCA) charts, which has been validated [26]. For the present study, we only used the COOP/WONCA summary index (WONCA) and the items in the physical function (WONCA PHF) and daily activities (WONCA DA) subscales. The questionnaire reference values [27] were also used in the study.
The 6 MW is a simple, objective, clinically useful test to estimate a subject’s exercise tolerance. It assesses distance walked over 6 min at a normal pace in a preset circuit. It is defined as a submaximal test, as it imposes a level of physiological stress that does not demand maximum aerobic capacity [28]. Its reliability in people with FM has been demonstrated [11], and it is widely used in this population [29–31]. The American Thoracic Society validated and produced guidelines for the 6 MW in 2002 [32], and reference values [33] have been published, which were later revised [34]. In this study, we used equation [33] [2.11 × height (cm)] – [2.29 × weight (kg)] – [5.78 × age (years)] + 667. We also recorded steps taken during the 6 MW using a pedometer, as described in the following paragraph.
The patients in the Multidisciplinary group received a Yamax Digi-walker SW-200 pedometer at the beginning of the program to measure the number of steps they took and as a treatment tool. They were instructed to wear it attached at the waist or belt at the anterior midline of the right leg and to register steps/day each night. The reliability and validity of this device have been previously assessed [35–37]. It is inexpensive and easy to use and motivates the patient to adhere to exercise instructions [38]. Pedometer use has been proposed in the treatment of patients with FM to encourage increased activity levels [39]. Steps/day during the entire course of treatment were recorded, but only the data from 81 full days were analyzed: the first and last 2 days were excluded, because data registration was not completed. For each participant, the mean and standard deviation of steps/day were calculated by study week.
Sociodemographic data were also collected at the beginning of the study, along with the Coping Strategies Questionnaire [19] and The Medical Outcome Study Sleep Scale to Sleep Index Problems [20]. Both questionnaires are self-administrated, and the first analyzes catastrophizing through 27 items divided into the following domains: distraction, catastrophizing, ignoring pain sensations, distancing from pain, coping self-statements, and praying. The second 12-item questionnaire measures sleep quality through dimensions of sleep such as initiation, maintenance, respiratory problems, quantity, perceived adequacy, and somnolence.
Data analysis
Frequencies and percentages were used to summarize the sample’s qualitative characteristics, and means (standard deviations) or median (interquartile interval) was employed for quantitative characteristics, depending on normality distribution. In order to compare groups, the Chi-squared test (for categorical variables) was used. In case of continuous or ordinal variables, the parametric Student t tests or the nonparametric Mann–Whitney test was performed, according to the Kolmogorov–Smirnov normality test.
Multilevel modeling (MLM) was used as an alternative analysis tool for repeated measures data. MLM does not require sphericity, it takes the sampling hierarchy into account, and it is capable of analyzing incomplete data. For that reason, MLM is a better option in comparison with conventional analysis of variance (ANOVA) for repeated measured. In addition, an analysis of trend in the temporal series was described to identify the effects of the treatment. For this aim, we have proposed a graphical analysis and a trend test.
Finally, an intent-to-treat analysis including subjects who dropped out of the trial was carried out to analyze the effect of Multidisciplinary program on 6 MW. The nonparametric Wilcoxon test was calculated in order to compare initial and posttreatment 6 MW.
We rejected the one-tailed null hypotheses when the p value was lower than 0.05. The data were analyzed using StataCorp. 2011. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP and the Statistical Package for the Social Sciences 23.0.
Results
Sample characteristics
In total, 155 women participated in the study. The median (interquartile interval) age of the subjects was 50 (45.0–54.0) years (maximum, 60; minimum, 26), and their body mass index was 26.82 (24.43–30.66) kg/m2 (maximum, 45.31; minimum, 17.26); thus, the population was overweight overall. Their initial 6 MW distance was 381.0 (341.0–423.0) meters, and their scores on the FIQ, 68.0 (53.0–77.0). Finally, the mean (standard deviation) on WONCA PHF and WONCA DA was 3.3 (0.7) and 3.1 (0.8), respectively. The groups showed no significantly different differences (p ≥ 0.05) in any characteristic (Table 1). We lost some participants during the follow-up period (Fig. 1).
Effect of Multidisciplinary program on FIQ values
The baseline FIQ values were higher in the Control group, but the difference was not significant. At 3-, 6-, and 12-month follow-ups, the between-group differences were significant, with the FIQ values lower in the Multidisciplinary group, indicating improvement (Fig. 2). In Table 2, we have performed a multilevel model in order to analyze differences between each time period and between-group treatments. We observe a significant iteration effect; in other words, the evolution of total score of FIQ over time is different for each group.
The percentages of patients achieving the minimum clinically significant FIQ difference were 64.2, 48.1, 42.0, and 27.2% posttreatment and at the 3-, 6-, and 12-month follow-ups, respectively, in the Multidisciplinary group; the corresponding percentages were 24.3, 23.0, 18.9, and 4%, respectively, in the Control group. Significant differences in that proportion were found posttreatment (p < 0.001), at the 3-month follow-up (p < 0.001), at the 6-month follow-up (p < 0.001), and at the 12-month follow-up (p < 0.001). We also analyzed the proportions of patients who went from the severe (FIQ > 59) to moderate (59 ≥ FIQ ≥ 39) or mild (FIQ < 39) impairment classifications according to Bennet et al. [23]. Although the groups started from similar values, the between-group difference was statistically significant at all evaluations (p < 0.050) except the 6-month follow-up (p = 0.061).
Effect of Multidisciplinary program on COOP/WONCA
The between-group differences at baseline were not statistically significant. We found posttreatment differences at the 3-, 6-, and 12-month follow-ups (Fig. 2).
Comparing our results with the reference values from Serrano-Gallardo [27] WONCA 20.7 (5), WONCA PHF 2.9 (standard deviation not published), WONCA DA 1.5 (standard deviation not published), our sample had higher baseline WONCA values although the study populations were similar in terms of health and gender (Fig. 2).
Table 2 shows a multilevel model for repeated values. We observe a significant difference between the group treatment and every moment in which the questionnaires were evaluated.
Moreover, the ICC, or intraclass correlation coefficient shown in Table 2, can be very in linear mixed models/multilevel models. It can be interpreted as the correlation among observations within the same group. In our case, we observe a high correlation in every questionnaire used, especially in FIQ and total score of WONCA.
Effect of Multidisciplinary program on 6 MW
The 6 MW distance values were higher in the Multidisciplinary than in the Control group at both baseline and posttreatment (Table 3). Since baseline 6 MW distance values were higher in the Multidisciplinary group, it is interesting to analyze difference (posttreatment value − baseline value) (Table 3). Pedometric registration of 6 MW completion showed that the Multidisciplinary group’s improvement resulted from the step length increase and not from an increased number of steps, evidenced by the difference in (posttreatment value − baseline value) between groups. However, the numbers of steps were unchanged, even the final and initial values within the same group (0.695).
According to Enright (1998), the 6 MW distance reference value from a healthy population is 554.5 (53.29) meters [28], significantly higher than our value obtained [mean: 368.5 (SD 54.45)]. While the difference between the baseline and posttreatment values was nearly constant for the Control group, the Multidisciplinary group’s values went from 169.8 (56.62) to 135.8 (57.70) meters (p < 0.001).
Steps/day during treatment
Steps/day data during the 3-month treatment were registered by the patients. Of the 73 total participants who finished the treatment, the 4 who did not present the register were excluded, resulting in 69 remaining participants. The mean number of days of step recording was 77.07 (8.48)/81. Of all participants, 44% collected data for all 81 days.
The average steps/day are classified by week-long periods in Fig. 3. We also analyzed the mean differences between the first week on the one hand and the second, seventh, and four last weeks on the other, finding significant differences (p < 0.05). In addition, the standard deviation of steps/day decreased in variability throughout the study (Fig. 4), with each of the last 5 weeks having a significantly different standard deviations from the first week (p < 0.05).
Discussion
The patients who underwent the Multidisciplinary treatment significantly improved in terms of functional status, physical activity level, and exercise regularity. By all measurements, the functional improvements were maintained 1 year after treatment completion. This study refutes criticism of the clinical significance of our Multidisciplinary program’s results [7]. In this study, we have used multilevel modeling (MLM) for the analysis of repeated measures data. Multilevel modeling for repeated measures data is most often discussed in the context of modeling change over time (in our case growth curve modeling for longitudinal designs). MLM is commonly used for repeated measures designs because it presents an alternative approach to analyzing repeated measures with many advantages over ANOVA for repeated measures (RM-ANOVA): MLM has less stringent assumptions in comparison with RM-ANOVA, allows hierarchical structure, can handle missing data easily, and can handle data in which there is variation in the exact timing of data collection. The analysis of clinically significant differences in total FIQ scores of subjects who underwent the Multidisciplinary treatment showed improvement compared with the subjects who followed only conventional pharmacologic treatment. We obtained similar results using a change cutoff of 14%, as proposed by Benett [23], analyzing the transition, from severe to mild impairment.
The total WONCA score and the WONCA PHF and WONCA DA domains from the Multidisciplinary group increased after treatment, and the gains were maintained 1 year afterward; the WONCA PHF was even raised to normal values described by Serrano-Gallardo [27]. Although the results obtained from each domain can be added to obtain the total WONCA score, Weel et al. [40], the developers of the original test, urged separate evaluation of the domains.
The other functional outcomes, 6 MW and steps/day, also showed improvement during treatment. Unfortunately, these were not recorded in the subsequent 3-, 6-, and 12-month follow-ups; thus, we cannot assess whether such posttreatment improvements were maintained afterward. Besides, because pedometers were considered a treatment tool and thus used only in the Multidisciplinary group, those functional outcomes could not be compared with any corresponding ones from the Control group.
The 6 MW baseline data agreed with the FM gait pattern observed by other authors: Auvinet et al. [41] and Pankoff et al. [42] found a slower gait in patients with FM, including decreased step length, and cycle frequency and bradykinesia. The present study showed posttreatment 6 MW improvements in terms of both distance walked and step length; consequently, the Multidisciplinary group achieved better functional gait, although they did not reach standard values for women with similar anthropomorphic characteristics [31, 41, 43]. Our results agree with previous studies and with Latorrre-Román et al. [31], who stated that 6 MW parameters could be a clinical relevance in FM. Thus, this study is the first to show gait improvement through step length after our Multidisciplinary program.
There was improvement in steps/day in the second treatment week; as we did not instruct the patients to walk any particular distance, we postulate that it could result from the positive motivation toward treatment or the pedometer adherence effect [36]. This increase was lost in the third week, and the results even showed a slight decrease; then, steps/day continued to decrease through the fourth and fifth weeks; that leveling off could be related to sleep deprivation caused by the CBT [44]. Finally, during the four last weeks of treatment, steps/day increased, and the standard deviation decreased compared with the first week; consequently, we observed an improvement in exercise capacity and regularity in the last weeks compared with the first one.
The main strength of our study is the 12-month follow-up. In spite of participant dropout, that follow-up revealed the preservation of functional improvements over time. We may have induced new positive habits in the participants, which could explain these differences; such improvements might be explained by enhancement of patient activity levels, as both groups started from low baseline 6 MW results, but only the Multidisciplinary returned to an essentially normal physical activity level. That effect may not be reproduced with a population having a higher initial activity level. In the same way, neuroscience also supports that functional improvement. A large body of evidence demonstrates that regular exercise is beneficial for FM [45, 46], and neuroimaging has found that regular exercise restored functional connectivity [47], increased the functional capacity of the pain modulatory system in subjects diagnosed with FM [48], and preserved brain volume in older adults [49].
Our work has some limitations that must be considered. When comparing the Multidisciplinary treatment group to the Control group, despite avoiding coincidence in time and place between groups, we did not consider the possible effect of communication between patients on the treatment received. Besides that, we unfortunately lost 10 Control patients, who were probably not sufficiently interested because they were only cited to be assessed. This loss is more evident in the 6 MW analysis. We could only give 22 patients to the group Control pre-treatment and 13 posttreatment, which weakens our results in this section. This fact could affect some other results because of the different degrees of attention that were dedicated to each of the groups. On the other hand, fewer than half of the patients counted the number of steps made every day using the pedometer, which could be explained by memory alteration characteristics of fibromyalgia patients [1]. However, we must bear in mind that the average number of days in which they counted the number of steps was 77/81, which shows good adherence to treatment [15–17].
Future research should consider motor Control as a main outcome. The gait pattern had changed at the end of the 24-session treatment, which was surprising, because the treatment included no direct gait intervention, but did include motor Control, which some authors have associated with gait or improved functional neuronal connections, evidenced by improved body image [50]. In future research, we recommend the combination of 6 MW and pedometer as functional outcome tools, as the latter promotes adherence and motivation.
Conclusion
In conclusion, the patients who underwent the Multidisciplinary treatment improved in terms of functional status, physical activity level, and exercise regularity. Besides, functional improvement was maintained 1 year after treatment completion.
References
Schweinhardt P, Fitzcharles MA, Boomershine C, Vierck C, Yunus MB (2012) Fibromyalgia as a disorder related to distress and its therapeutic implications. Pain Res Treat 2012:950602. doi:10.1155/2012/950602
Häuser W, Thieme K, Turk DC (2010) Guidelines on the management of fibromyalgia syndrome: a systematic review. Eur J Pain 14:5–10. doi:10.1016/j.ejpain.2009.01.006
Hamnes B, Mowinckel P, Kjeken I, Hagen KB (2012) Effects of a one week multidisciplinary inpatient self-management programme for patients with fibromyalgia: a randomised controlled trial. BMC Musculoskelet Disord 13:189. doi:10.1186/1471-2474-13-189
Clauw DJ (2014) Fibromyalgia: a clinical review. JAMA 311:1547–1555. doi:10.1001/jama.2014.3266
Castel A, Fontova R, Montull S, Periñán R, Poveda MJ, Miralles I, Cascón-Pereira R, Hernández P, Aragonés N, Salvat I, Castro S, Monterde S, Padrol A, Sala J, Añez C, Rull M (2013) Efficacy of a multidisciplinary fibromyalgia treatment adapted for women with low educational levels: a randomized controlled trial. Arthritis Care Res (Hoboken) 65:421–431. doi:10.1002/acr.21818
Casanueva-Fernández B, Llorca J, Rubió JBI, Rodero-Fernández B, González-Gay MA (2012) Efficacy of a multidisciplinary treatment program in patients with severe fibromyalgia. Rheumatol Int 32:2497–2502. doi:10.1007/s00296-011-2045-1
Marcus D, Bernstein CD, Haq A, Breuer P (2014) Including a range of outcome targets offers a broader view of fibromyalgia treatment outcome: results from a retrospective review of multidisciplinary treatment. Musculoskelet Care 12:74–81. doi:10.1002/msc.1056
Wilson IB, Cleary PD (1995) Linking clinical variables with health-related quality of life. JAMA 273(59–65):59–65
Burckhardt CS, Clark SR, Bennett RM (1991) The fibromyalgia impact questionnaire: development and validation. J Rheumatol 18:728–733
Ángel García D, Martínez Nicolás I, Saturno Hernández PJ (2016) Clinical approach to fibromyalgia: synthesis of Evidence-based recommendations, a systematic review. Reumatol Clin 12:65–71. doi:10.1016/j.reuma.2015.06.001
Pankoff BA, Overend TJ, Lucy SD, White KP (2000) Reliability of the six-minute walk test in people with fibromyalgia. Arthritis Care Res 13:291–295
Pankoff B, Overend T, Lucy D, White K (2000) Validity and responsiveness of the 6 minute walk test for people with fibromyalgia. J Rheumatol 27:2666–2670
Fontaine KR, Haaz S (2007) Effects of lifestyle physical activity on health status, pain, and function in adults with fibromyalgia syndrome. J Musculoskelet Pain 15:3–9
Nelson E, Wasson J, Kirk J, Keller A, Clark D, Dietrich A, Stewart A, Zubkoff M (1987) Assessment of function in routine clinical practice: description of the COOP Chart method and preliminary findings. J Chronic Dis. doi:10.1016/S0021-9681(87)80033-4
De Cocker KA, De Bourdeaudhuij IM, Cardon GM (2008) The effect of pedometer use in combination with cognitive and behavioral support materials to promote physical activity. Patient Educ Couns 70:209–214. doi:10.1016/j.pec.2007.10.008
Kang M, Marshall SJ, Barreira TV, Lee JO (2009) Effect of pedometer-based physical activity interventions: a meta-analysis. Res Q Exerc Sport 80:648–655. doi:10.5641/027013609X13088500160000
Heesch KC, Dinger MK, McClary KR, Rice KR (2005) Experiences of women in a minimal contact pedometer-based intervention: a qualitative study. Women Health 41:97–116. doi:10.1300/J013v41n02_07
Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, Tugwell P, Campbell SM, Abeles M, Clark P, Fam AG, Farber SJ, Fiechtner JJ, Franklin CM, Gatter RA, Hamaty D, Lessard J, Lichtbroun AS, Masi AT, Mccain GA, Reynolds WJ, Romano TJ, Russell IJ, Sheon RP (1990) The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Report of the multicenter criteria committee. Arthritis Rheum 33:160–172. doi:10.1002/art.1780330203
Rosenstiel K, Keefe FJ (1983) The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain 17:33–44. doi:10.1016/0304-3959(83)90125-2
Hays RD, Martin S, Sesti AM, Spritzer KL (2005) Psychometric properties of the medical outcomes study sleep measure. Sleep Med 6:41–44. doi:10.1016/j.sleep.2004.07.006
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:61–70
Esteve-Vives J, Rivera J, Salvat MI, Gracia MD (2007) Propuesta de una versión de consenso del Fibromyalgia Impact Questionnaire (FIQ) para la población española. Reumatol Clin 3:21–24
Bennett RM, Bushmakin AG, Cappelleri JC, Zlateva G, Sadosky AB (2009) Minimal clinically important difference in the fibromyalgia impact questionnaire. J Rheumatol 36:1304–1311. doi:10.3899/jrheum.081090
Monterde S, Salvat I, Montull S, Fernández-Ballart J (2004) Validación de la versión española del Fibromyalgia Impact Questionnaire. Rev Esp Reum 31(9):507–513
Lennon OC, Carey A, Creed A, Durcan S, Blake C (2011) Reliability and validity of COOP/WONCA functional health status charts for stroke patients in primary care. J Stroke Cerebrovasc Dis 20:465–473. doi:10.1016/j.jstrokecerebrovasdis.2010.02.020
Lizán Tudela L, Reig Ferrer A (1999) Cross cultural adaptation of a health related quality of life measurement: the Spanish version of the COOP/WONCA cartoons. Aten Primaria 24:75–82
Serrano-Gallardo P, Lizán-Tudela L, Díaz-Olalla JM, Otero Á (2009) Valores poblacionales de referencia de la versión española de las viñetas COOP/WONCA de calidad de vida en población adulta urbana. Med Clin (Barc) 132:336–343. doi:10.1016/j.medcli.2008.04.009
Enright PL (2003) The six-minute walk test. Respir Care 48:783–785
King S, Wessel J, Bhambhani Y, Maikala R, Sholter D, Maksymowych W (1999) Validity and reliability of the 6 minute walk in persons with fibromyalgia. J Rheumatol 26:2233–2237
Ayán C, Martín V, Alonso-Cortés B, Alvarez MJ, Valencia M, Barrientos MJ (2007) Relationship between aerobic fitness and quality of life in female fibromyalgia patients. Clin Rehabil 21:1109–1113. doi:10.1177/0269215507077365
Latorre-Román P, Santos-Campos M, Heredia-Jimenez J, Delgado-Fernández M, Soto-Hermoso V (2014) Analysis of the performance of women with fibromyalgia in the six-minute walk test and its relation with health and quality of life. J Sport Med Phys Fit 54:51–57
Crapo RO, Casaburi R, Coates AL, Enright P, Macintyre NR, McKay RT, Johnson D, Wagner J, Zeballos RJ (2002) ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 166:111–117. doi:10.1164/rccm.166/1/111
Enright PL, Sherrill DL (1998) Reference equations for the six-minute walk in healthy adults. Am J Respir Crit Care Med 158:1384–1387. doi:10.1097/00008483-199903000-00015
Dourado VZ (2011) Reference equations for the 6-minute walk test in healthy individuals. Arq Bras Cardiol 96:128–138
Tudor-Locke C, Williams JE, Reis JP, Pluto D (2002) Utility of pedometers for assessing physical activity: convergent validity. Sports Med 32:795–808
Tudor-Locke C, Williams JE, Reis JP, Pluto D (2004) Utility of pedometers for assessing physical activity: construct validity. Sport Med 34:281–291
Bassett DR, John D (2010) Use of pedometers and accelerometers in clinical populations: validity and reliability issues. Phys Ther Rev 15:135–142. doi:10.1179/1743288X10Y.0000000004
Evangelista LS, Hamilton MA, Fonarow GC, Dracup K (2010) Is exercise adherence associated with clinical outcomes in patients with advanced heart failure? Phys Sportsmed 38:28–36. doi:10.3810/psm.2010.04.1759
Martín-Borràs C, Giné-Garriga M, Martínez E, Martín-Cantera C, Puigdoménech E, Solà M, Castillo E, Beltrán AM, Puig-Ribera A, Trujillo JM, Pueyo O, Pueyo J, Rodríguez B, Serra-Paya N, SEDESTACTIV Study Group (2014) Effectiveness of a primary care-based intervention to reduce sitting time in overweight and obese patients (SEDESTACTIV): a randomized controlled trial; rationale and study design. BMC Public Health 14:228. doi:10.1186/1471-2458-14-228
Van Weel C, König-Zahn C, Touw-Otten FWMM, Van Duijn NP, Meyboom-de Jong B (2012) Measuring functional status with the COOP/WONCA charts: a manual, 2nd edn. UMCG/University of Groningen, Research Institute SHARE, Groningen
Auvinet B, Bileckot R, Alix AS, Chaleil D, Barrey E (2006) Gait disorders in patients with fibromyalgia. Jt Bone Spine 73:543–546. doi:10.1016/j.jbspin.2005.10.020
Pankoff BA, Overend TJ, Lucy SD, White KP (2000) Reliability of the six-minute walk test in people with fibromyalgia. Arthritis Care Res 13:291–295
Heredia Jiménez JM, Aparicio García-Molina VA, Porres Foulquie JM, Delgado Fernández M, Soto Hermoso VM (2009) Spatial-temporal parameters of gait in women with fibromyalgia. Clin Rheumatol 28:595–598. doi:10.1007/s10067-009-1101-7
Espie CA (2006) Overcoming insomnia and sleep problems: a self- help guide using cognitive-behavioral techniques. Robinson, London
Bidonde J, Busch AJ, Bath B, Milosavljevic S (2014) Exercise for adults with fibromyalgia: an umbrella systematic review with synthesis of best evidence. Curr Rheumatol Rev 10:45–79. doi:10.2174/1573403X10666140914155304
Ramel J, Bannuru R, Griffith M, Wang C (2009) Exercise for fibromyalgia pain: a meta-analysis of randomized controlled trials. Curr Rheumatol Rev 5:188–193. doi:10.2174/157339709790192459
Flodin P, Martinsen S, Mannerkorpi K, Löfgren M, Bileviciute-Ljungar I, Kosek E, Fransson P (2015) Normalization of aberrant resting state functional connectivity in fibromyalgia patients following a three month physical exercise therapy. Neuroimage Clin 9:134–139. doi:10.1016/j.nicl.2015.08.004
Ellingson L, Stegner A, Schwabacher I, Koltyn KF, Cook DB (2016) Exercise strengthens central nervous system modulation of pain in fibromyalgia. Brain Sci 6:8. doi:10.3390/brainsci6010008
Smith JC, Nielson KA, Woodard JL, Seidenberg M, Durgerian S, Hazlett KE, Figueroa CM, Kandah CC, Kay CD, Matthews MA, Rao SM (2014) Physical activity reduces hippocampal atrophy in elders at genetic risk for Alzheimer’s disease. Front Aging Neurosci. doi:10.3389/fnagi.2014.00061
Bray H, Moseley GL (2011) Disrupted working body schema of the trunk in people with back pain. Br J Sport Med 45:168–173. doi:10.1136/bjsm.2009.061978
Acknowledgements
The authors gratefully acknowledge Joan Fernández Ballart and Eva Maria Andrés Esteban for their support with statistical analysis.
Funding
Supported by the Foundation Marató TV3 Grant number 070910.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Salvat I, Zaldivar P, Montull S, Monterde S, Miralles I, and Castel A declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Salvat, I., Zaldivar, P., Monterde, S. et al. Functional status, physical activity level, and exercise regularity in patients with fibromyalgia after Multidisciplinary treatment: retrospective analysis of a randomized controlled trial. Rheumatol Int 37, 377–387 (2017). https://doi.org/10.1007/s00296-016-3597-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-016-3597-x