Abstract
Cardiac involvement (CI) is a known complication of SSc associated with increased mortality. Our objective was to describe a cohort of patients with SSc and CI and to assess the differences between cutaneous subsets regarding their presentation and survival. Three hundred and ninety-three Spanish patients from a single center, diagnosed with SSc, were retrospectively studied for evidence of CI using noninvasive and invasive tests from 1976 to 2011. Clinical, epidemiological, immunological and therapeutic features of patients with CI were compared to those without it and within the different cutaneous subsets of SSc. CI was present in 173 (44 %) patients. Mitral regurgitation (67 %), conduction alterations (45 %) and left ventricle diastolic dysfunction (40 %) were the most common findings. Pericardial involvement and heart failure were more frequent in diffuse SSc (dcSSc) than in limited or sine scleroderma SSc. CI accounted for 20 % of deaths, and it was an independent mortality risk factor (HR 2.1, P = 0.02), but once CI was established, classical dcSSc mortality risk factors determined mortality. Patients with dcSSc developed CI faster than limited (HR 1.9, P = 0.003) or sine SSc patients (HR 2.5, P = 0.002), specially during the first year after SSc onset. We found statistically significant differences between the 3 SSc subsets in the presentation of pericardial involvement and heart failure. CI increased the mortality and appeared at a higher rate, especially during the first year after SSc onset. Screening for heart involvement should be performed at diagnosis and during follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic sclerosis (SSc) is a systemic disease that may affect many organs; among them, cardiac involvement (CI) has drawn attention in the last years. CI may be a direct consequence of SSc (primary CI) or secondary to other organ involvement, like right ventricular dilatation or hypertrophy due to pulmonary arterial hypertension (PAH). The pathogenesis of primary CI has been related to myocardial fibrosis, but also to coronary vasospasm [1–4] and more recently to coronary artery disease [5–7]. CI may also be caused by concomitant conditions like cardiovascular risk factors among other diseases present in the general population.
A broad variety of clinical and subclinical manifestations have been related to primary CI in SSc patients, including myocarditis, myocardial fibrosis, left ventricular systolic and diastolic dysfunction, myocardial ischemia and coronary artery abnormalities, pericarditis and pericardial effusion, conduction alterations and valvular dysfunction [8].
The prevalence of CI may be significant among patients with CI. Ferri et al. [9] estimated in a study that 32 % of dcSSc patients and 23 % of lcSSc patients had CI. The cumulative risk of death for SSc patients with CI has been reported to be around 3.15, similarly to other important independent mortality risk factors like interstitial lung disease (ILD), PAH or renal involvement. CI usually develops in patients with other organ-specific alterations. It can account for 20–30 % of all the premature deaths in the SSc population [10]. Clinically apparent CI is associated with an increased risk of death, included as one of the items in the Medsger’s severity scale [11]. Therefore, early detection of CI may be essential for appropriate management of SSc patients [12]. However, so far, no consensus assessment strategies have been established. CI can be present in three cutaneous SSc subsets (diffuse dcSSc, limited lcSSc and sine ssSSc), but dcSSc with rapid progression of skin thickness has been associated with an earlier CI onset and with an increased severity of the disease [13].
In first place, this study aimed to assess the prevalence of CI, primary or secondary, in a Spanish cohort of patients with SSc. The second objective was to describe the CI manifestations present in patients classified in dcSSc, lcSSc, ssSSc and pre-scleroderma (preSSc) subsets, according to the modified LeRoy and Medsger classification [14]. Finally, we aimed to determine whether CI was an independent risk factor for mortality in our cohort.
Materials and methods
Patient population
Patients from the Vall d’Hebron Universitary Hospital SSc cohort meeting the criteria for any of the groups included in the modified LeRoy and Medsger classification [14] and under active follow-up (minimum one yearly visit as outpatients) from 1976 to 2011 were included in the study. The institutional review board of our center approved the project, and no external financial funding was received.
Database management
CPS and VFP designed the original database and introduced the data. Data were anonymized in order to preserve patients’ privacy. CPS, VFP and AFC kept all data. AFC and IPF completed the data collection and, along with CPS and VFP, elaborate the design of the final dataset. Data were obtained from the SSc outpatient clinic and from the Internal Medicine ward in the Vall d’Hebron University Hospital, Barcelona, on the basis of our daily clinical practice. Clinical and epidemiological data from the medical records as well as results of the tests performed were included.
SSc subgroups
Patients were divided into four groups (dcSSc, lcSSc, ssSSc and preSSc) according to the extent of skin sclerosis, meeting the modified classification of LeRoy and Medsger, as defined elsewhere [15]:
-
dcSSc: skin thickening extended proximally to elbows and knees or including trunk.
-
lcSSc: skin sclerosis was confined distally to elbows and knees or face.
-
ssSSc: absence of skin sclerosis and presence of Raynaud phenomenon or a peripheral vascular equivalent (digital tip ulcers, abnormal nailfold capillaroscopy), scleroderma clinical features [gastrointestinal hypomotility, interstitial lung disease (ILD), pulmonary hypertension (PH), scleroderma renal crisis (SRC) or typical CI], and antinuclear autoantibodies but without skin sclerosis.
-
preSSc: absence of skin sclerosis and presence of Raynaud phenomenon plus any of the following: abnormal nailfold capillaroscopy and/or SSc specific autoantibodies.
Clinical and epidemiological variables
The analyzed data included the onset (considered as the moment the first symptom appeared, including Raynaud phenomenon) and death dates, the cause of death and other SSc-associated conditions. The cause of death was established by the review by two clinicians of the death certificates and the clinical records. In case there was no agreement or information for a definite cause of death, it was considered unknown. These conditions were assessed every 3 to 6 months depending on the physician criteria. They were:
-
Presence of digital ulcers at physical examination
-
Esophageal involvement that consisted in hypomotility of the lower two-thirds of the oesophagus and/or decreased peristalsis, confirmed by manometry or cine-radiographic studies.
-
Capillaroscopic pattern: slow, active or normal as described by Maricq [16].
-
ILD considered in patients meeting any of the following criteria: restrictive pulmonary pattern with forced vital capacity below 80 % of expected value on respiratory function tests or pulmonary interstitial pattern evidenced by high-resolution computerized tomography or by chest X-ray.
-
PH when systolic pulmonary arterial pressure was estimated to be above 40 mmHg by Doppler echocardiogram [17] or when mean pulmonary arterial pressure was found to be equal or higher than 25 mmHg, determined by right-sided heart catheterization.
-
SRC as defined by Traub et al. [18].
Cardiovascular risk factors like High blood pressure (HBP) diabetes mellitus and dyslipidemia were defined as indicated by the 2007 European consensus [19]. Smoking habit was assessed by asking patients whether they had ever smoked. The prescription of ACEI (angiotensin-converting-enzyme inhibitors) or ARB (angiotensin receptor blockers), both in the same category, and calcium channel blockers (CCB) was reported. The indications for the prescription of these drugs were: SSc manifestations different from CI (Raynaud phenomenon, digital ulcers), SSc CI manifestations and non-SSc comorbidities.
On an immunological level, anti-centromere autoantibodies (ACA) were detected by immunofluorescence assay on Hep-2 cell substrate. Anti-topoisomerase-I antibodies (ATA) were detected by immunoblotting.
Cardiac involvement
Given the large number of cardiac manifestations associated with SSc and the absence of a consensus definition, we considered that a patient had CI if any of the objective cardiologic tests was concordantly altered or if any of the associated medical conditions was reported. A yearly per-protocol transthoracic echocardiography and an electrocardiogram were performed. Myocardial perfusion SPECT (under dipyridamole or cold stress conditions) or coronary angiography was performed if there was clinical suspicion of further CI. Cardiac manifestations associated with primary SSc involvement were included into the dataset.
Complementary procedures
-
Transthoracic echocardiography: left ventricle hypertrophy (LVH) defined by a left ventricle mass index ≥134 g/m2; left ventricle diastolic dysfunction (LVDD) defined by an E/A relation ≤1 and mitral deceleration time >240 ms; and measurement of left ventricle ejection fraction (LVEF) classifying results as ≥50 or <50 % as Allanore et al. [20]; presence of mitral or aortic regurgitation; presence of pericardial effusion.
-
Dipyridamole and cold-induced stress myocardial perfusion SPECT (single-photon emission tomography): presence or absence of pathologic thallium myocardial perfusion [21, 22].
-
Coronary angiography: angiographically significant lesions (a degree of stenosis ≥60 %) or coronary vasospasm (absence of angiographically significant lesions and presence of epicardial spasm after infusion of acetylcholine).
-
Electrocardiogram: the presence of any of the following: atrial fibrillation, ventricular extrasystoles, atrial flutter, supraventricular paroxysmal tachycardia, bundle and fascicular block, atrioventricular block, ventricular tachycardia [23]. Ultrasounds and electrocardiograms were performed by protocol. The rest of procedures were performed under suspicion of CI, suspected either clinically by an expert physician or by alterations in protocol testing.
Medical conditions
-
Pericarditis or cardiac tamponade.
-
Ischemic cardiopathy (documented myocardial infarction, angina, ischemic alterations in myocardial perfusion SPECT or requirement of coronary revascularization, surgical or percutaneous).
-
Pacemaker bearing regardless of the type of arrhythmia.
-
Sudden death.
-
Congestive heart failure: as defined by the European Society of Cardiology [24].
Statistical analysis
Qualitative variables were expressed as percentages and absolute frequencies while quantitative variables were expressed as mean and standard deviation. For each specific statistical procedure, we excluded those patients who lacked any of the variables involved in that analysis. Student’s t test and Chi-squared test or Fisher´s exact test, as appropriate, were used to compare quantitative and qualitative variables among clinical groups.
To assess the influence of CI on mortality and of the type of SSc on CI, we compared the time to the onset of CI and the mortality from the onset of CI among SSc clinical subsets. We also analyzed the mortality from SSc onset between patients with and without CI.
The Kaplan–Meier method was used to calculate survival estimates, and Cox proportional-hazards regression analysis was used to estimate hazard ratios (HR) that were adjusted for sex, age at SSc onset, ILD, PH and scleroderma renal crisis as potential confounding factors of the relationship between CI and mortality and also between the type of SSc with CI and death. For all Cox models, we plotted scaled Schoenfeld residuals against follow-up time and found no violation of the proportional-hazards assumption.
Because this was an exploratory study, a two-sided p value of <0.05 was considered significant for these analysis, with no correction for multiple comparisons. Stata/SE 12 was used to perform the statistical analysis.
Results
Baseline characteristics
Three hundred and ninety-three SSc patients (of which 90 % were women) were included in the study, and their distribution by subsets is shown in Table 1. One hundred and seventy-three (43 %) had some type of CI. Overall, nearby 50 % of the patients in the dcSSc group and in the lcSSc group had CI. Patients with CI were older at SSc onset (45.7 years vs. 39.9 years, P < 0.001) and at SSc diagnosis (55.6 years vs. 47 years, P < 0.001) having significantly more SSc manifestations and organ involvement than patients without CI. Regarding SSc cutaneous subsets, a higher percentage of patients in the CI group had lcSSc (67 vs. 53 %, P = 0.004); on the contrary, ssSSc was more frequent in those patients without CI (30 vs. 12 %, P < 0.001) (Table 1). Patients with CI and dcSSc were younger at diagnosis and at death. Moreover, the presence of digital ulcers, ILD, SRC, anti-topoisomerase I positivity and an active capillaroscopy pattern was more frequent in dcSSc. Finally, lcSSc and ssSSc patients with CI presented with anti-centromere antibody positivity and a slow capillaroscopy pattern more frequently than dcSSc and, lcSSc patients, compared to ssSSc, had significantly more digital ulcers and interstitial lung disease (Table 2).
Cardiac involvement among systemic sclerosis subsets
Patients with dcSSc were younger at CI onset, and the time from SSc onset to CI onset was shorter than in those with lcSSc or ssSSc. Moreover, congestive heart failure was more frequent in dcSSc (Table 3). Interestingly, aortic regurgitation was significantly more frequent in lcSSc than in dcSSc (36 vs. 16 %, P = 0.02) and the pericardial involvement frequency was significantly associated with the type of SSc subset, higher in dcSSc than in lcSSc (46 vs. 24 %, P = 0.01) or ssSSc (46 vs. 0 %, P < 0.001) and also in lcSSc, compared to ssSSc (24 vs. 0 %, P = 0.01). Other cardiologic manifestations were not significantly different between clinical subsets.
Cardiovascular treatments and risk factors were homogenously distributed among SSc subsets of patients, except for an increase frequency of treatment with calcium channel blockers in dcSSc patients than in those with lcSSc.
Mortality causes
Out of 173 patients with CI, 60 died during the study follow-up period. PH (13 cases, 22 %) was the most important cause of death, closely followed by cardiovascular disease, the second cause in our cohort (12 patients, 20 %: 9 from heart failure and 3 from ischemic cardiomyopathy) (Table 4). Regarding the causes of death among SSc subsets, ILD and SRC were more frequent in patients with dcSSc than in those with lcSSc, while PH was more frequent in lcSSc than in dcSSc.
Survival study
Regression study confirmed cardiac involvement as an independent risk factor for mortality in SSc patients (adjusted HR 2.1; 95 % CI 1.1 to 3.8; P = 0.02), together with the age at SSc onset and the presence of ILD, PH and SRC (Table 5). Accordingly, unadjusted 10-year survival in patients with cardiac involvement was 90 %, compared to 98 % in patients without this manifestation (Fig. 1).
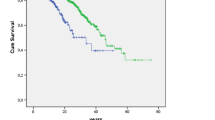
Finally, death risk after the onset of CI was associated with the traditional SSc mortality risk factors: SSc subset (lower in ssSSc than in lcSSc or dcSSc) (Fig. 2), age and presence of ILD, PH and SRC (Table 5).
Risk factors for developing cardiac involvement
dcSSc patients had an increased hazard of CI, compared to both lcSSc (adjusted HR 1.9; 95 % CI 1.2 to 2.9; P = 0.003) and ssSSc (adjusted HR 2.5; 95 % CI 1.4 to 4.6; P = 0.002). It is interesting to point out the rate at which CI increased during the first year after the onset of the disease in dcSSc patients and stabilized afterward, compared to other SSc subsets (Fig. 3). Aside from the SSc subset, SRC and, obviously, age at SSc onset were also hazard factors for CI (Table 5).
Discussion
CI in SSc is a multifaceted problem. Many depictions of CI-related alterations or conditions have been described in medical literature [8]. Despite the fact that definite SSc CI criteria do no exist, and authors have used different definitions in their papers, CI has been strongly related to increased mortality rates by international meta-analysis focusing on death causes [10, 25, 26]. Issues like hypothetical differences between cutaneous subsets are still insufficiently studied.
We performed a retrospective cohort study based on a 393 single-center Spanish cohort of patients. One hundred and seventy-three individuals showed clinical or subclinical CI. The most common CI manifestations were mitral regurgitation, conduction alterations and left ventricle diastolic dysfunction. CI appeared earlier and was more prevalent in dcSSc. Congestive heart failure was more common in dcSSc, and pericardial involvement showed a frequency gradient over SSc subsets (dcSSc > lcSSc > ssSSc). CI accounted directly for 20 % of deaths. A twofold mortality in patients with SSc was observed for those affected by CI. dcSSc proved to be an independent risk factor for CI, specially during the first year of the disease. Once CI was established, classical SSc risk factors (SSc subset, ILD, PH, SRC and age) influenced mortality.
The analysis of the baseline data of all the series, including epidemiology, non-cardiac organic involvement and immunology, was all coherent with results from our own National registry series [15] and the EUSTAR [27] registry. Patients with CI presented other SSc organ involvement more than the non-CI group, SSc started earlier, and less patients presented ssSSc. Therefore, it seems that SSc patients with CI suffer from a more severe disease, as it will be discussed further on. Although autoantibodies may play a determinant role in SSc [28], anti-centromere and anti-topoisomerase I antibodies were evenly distributed among patients with and without CI. Other antibodies could have more influence at this level and may motivate directed studies in the future. Male gender has been associated with a higher incidence of heart involvement [29], but, on the contrary, we did not find this phenomenon in our cohort.
Globally, the prevalence of the diverse CI alterations and explorations in the 393-patient sample are in concordance with the ones reported in 2011 by Desai et al. [12], who collected the prevalence of diverse CI conditions from many separate observational studies in a review article. Again, CI resulted to appear earlier in life and to develop in less time from the SSc onset in the dcSSc subset than in the other groups. These findings correspond to the ones reported in an Italian study in 2014, the only paper in literature that has tried to assess differences between dcSSc and lcSSc in patients with SSc and CI in a series of 171 patients [30]. They found that 63.9–45.7 % (depending if valvular abnormalities were minor or not) of the patients presented CI versus an overall of 44 % in our study. Unlike in that case, we have found significant differences in pericardial involvement and congestive heart failure, already described above. The rest of the CI features did not present differences between SSc subsets.
Decreased LVEF was uncommon, as in other series (4 vs 5.6 %) [20]. The presence of LVDD ranged from 17.7 % in a large cohort using traditional Doppler echocardiography [31] to 63 % in the latest studies performing tissue Doppler echocardiography [32]. Forty percent of our patients had LVDD, the third alteration in frequency after mitral regurgitation and conduction alterations. Although it may be influenced by age or cardiovascular risk factors, it is considered a key feature in SSc CI appearing after myocardial fibrosis and it may be associated with an increased risk of mortality [33]. Mitral and aortic regurgitation were found in a very significant number of patients in our study in comparison with a nationwide French study [30], but in that article, patients with significant valvular disease were excluded. Aortic regurgitation was remarkably more frequent in patients with lcSSc than in those with dcSSc in our study, but these results have to be interpreted with caution known that it was not designed to assess the degree of valvular pathology. Nonetheless, the presence of mild valvular alterations was well described years ago [22], and recent review works confirm their prevalence [33]. Valvular alterations may constitute subclinical manifestations of SSc, and thus, directed studies should be conducted to assess their extent and progression rate.
Conduction alterations were present in 22.9 % of our patients, as in other series [33]. Atrial fibrillation was the most common one, but right bundle branch block, recently described as an independent predictor of mortality [34], was also found in 25 patients (6 %). Only four patients required a pacemaker. Cardiovascular risk factors and drugs were similarly distributed among patients with and without CI with the exception of CCB. CCB were more frequently prescribed in dcSSc, probably because of the greater presence of digital ulcerations in this subgroup of patients.
Prognosis for patients with CI seems worse [35–37], accounting for at least 29 % of SSc-related deaths in a 2011 meta-analysis [38], although it may be underestimated due to the difficulty to discern between primary and secondary cardiac involvement. In our study, mortality among patients with SSc and CI due to heart involvement (heart failure and ischemic cardiopathy) represented 20 % of the deceases. According to previous reports, CI doubled the mortality rate in SSc patients, considered an independent mortality risk factor along with ILD, PH, SRC and age [39].
Moreover, CI rate proved to be increased in dcSSc, especially during the first year after SSc onset, stabilizing afterward. Even if it could be argued that the sharp increase in the CI rate during the first year may be due to detection of prevalent undiagnosed CI during the initial workup of dcSSc patients, the same workup was performed for the rest of SSc patients and this effect was not observed. Consequently, we believe this finding can be applied to practice, suggesting that, as in the case of other SSc target organs, during the first year after the onset of disease, dcSSc patients may have a greater risk to develop CI. To this day, solely the combination of annual echocardiography and tissue Doppler with a determination of brain natriuretic peptide has been proposed as screening to detect CI in SSc. The rest of heart-related tests should be performed in the case of concrete clinical manifestations [12]. Further studies are warranted to assess the best initial screening to detect CI in these patients and the optimal therapeutic strategy once it is established.
The long follow-up of our cohort may rise worry about secular trend bias, to assess this point we stratified our cohort between patients with SSc onset before and after 1990 and did not find any difference between the two groups of patients in the analysis contained in this paper (“Electronic Supplementary Material”). The fact that there is no specific treatment for SSc CI, unlike for SRC or PAH, may explain this phenomenon .
The main limitations of our study were: the use of an historic cohort, the absence of a control group, the retrospective collection of data and the limited number of patients. Authors would like to point the low number of men enrolled (10 %) and the high frequency of ssSSc (15 %). Authors used the Maricq capillaroscopic patterns known that newer criteria were not available at the beginning of the study. The lack of an internationally accepted definition of CI in SSc was a strong limitation in terms of establishing strict inclusion criteria. Moreover, the difficulty of establishing the etiology of the CI, related with SSc or unrelated, was another limitation. We tried to include all CI alterations described in literature in order to avoid underestimating SSc heart disease.
Conclusions
In summary, cardiac involvement is a frequent complication in SSc patients and an independent mortality risk factor. Moreover, dcSSc may increase the hazard of early cardiac involvement, predominantly during the first year after the onset of the disease. Therefore, screening for heart involvement should be conducted actively in all SSc subjects in order to assess the progression of the disease.
References
Follansbee WP, Miller TR, Curtiss EI, Orie JE, Bernstein RL, Kiernan JM, Medsger TA Jr (1990) A controlled clinicopathologic study of myocardial fibrosis in systemic sclerosis (scleroderma). J Rheumatol 17:656–662
Bulkley BH, Ridolfi RL, Salyer WR, Hutchins GM (1976) Myocardial lesions of progressive systemic sclerosis: a cause of cardiac dysfunction. Circulation 53:483–490
Kahan A, Allanore Y (2006) Primary myocardial involvement in systemic sclerosis. Rheumatology (Oxford) 45(Suppl 4):14–17
Meier FM, Frommer KW, Dinser R, Walker UA, Czirjak L, Denton CP, Allanore Y, Distler O, Riemekasten G, Valentini G, Müller-Ladner U, EUSTAR Co-authors (2012) Update on the profile of the EUSTAR cohort: an analysis of the EULAR Scleroderma Trials and Research group database. Ann Rheum Dis 71:1355–1360
Chu SY, Chen YJ, Liu CJ, Tseng WC, Lin MW, Hwang CY, Chen CC, Lee DD, Chen TJ, Chang YT, Wang WJ, Liu HN (2013) Increased risk of acute myocardial infarction in systemic sclerosis: a nationwide population-based study. Am J Med 126(11):982–988
Nordin A, Jensen-Urstad K, Björnådal L, Pettersson S, Larsson A, Svenungsson E (2013) Ischemic arterial events and atherosclerosis in patients with systemic sclerosis: a population-based case-control study. Arthritis Res Ther 15(4):R87
Ali H, Ng KR, Low AH (2015) A qualitative systematic review of the prevalence of coronary artery disease in systemic sclerosis. Int J Rheum Dis 18(3):276–286
Boueiz A, Mathai SC, Hummers LK, Hassoun PM (2010) Cardiac complications of systemic sclerosis: recent progress in diagnosis. Curr Opin Rheumatol 22:696–703
Ferri C, Valentini G, Cozzi F, Sebastiani M, Michelassi C, La Montagna G, Bullo A, Cazzato M, Tirri E, Storino F, Giuggioli D, Cuomo G, Rosada M, Bombardieri S, Todesco S, Tirri G, Systemic Sclerosis Study Group of the Italian Society of Rheumatology (SIR-GSSSc) (2002) Systemic sclerosis: demographic, clinical, and serologic features and survival in 1,012 Italian patients. Medicine (Baltimore) 81:139–153
Komócsi A, Vorobcsuk A, Faludi R, Pintér T, Lenkey Z, Költo G, Czirják L (2012) The impact of cardiopulmonary manifestations on the mortality of SSc: a systematic review and meta-analysis of observational studies. Rheumatology (Oxford) 51:1027–1036
Medsger TA Jr, Silman AJ, Steen VD, Black CM, Akesson A, Bacon PA, Harris CA, Jablonska S, Jayson MI, Jimenez SA, Krieg T, Leroy EC, Maddison PJ, Russell ML, Schachter RK, Wollheim FA, Zacharaie H (1999) A disease severity scale for systemic sclerosis: development and testing. J Rheumatol 26:2159–2167
Desai CS, Lee DC, Shah SJ (2011) Systemic sclerosis and the heart: current diagnosis and management. Curr Opin Rheumatol 23:545–554
Meune C, Vignaux O, Kahan A, Allanore Y (2010) Heart involvement in systemic sclerosis: evolving concept and diagnostic methodologies. Arch Cardiovasc Dis 103:46–52
LeRoy EC, Medsger TA Jr (2001) Criteria for the classification of early systemic sclerosis. J Rheumatol 28:1573–1576
Simeón-Aznar CP, Fonollosa-Plá V, Tolosa-Vilella C, Espinosa-Garriga G, Ramos-Casals M, Campillo-Grau M, García-Hernández FJ, Castillo-Palma MJ, Sánchez-Román J, Callejas-Rubio JL, Ortego-Centeno N, Egurbide-Arberas MV, Trapiellla-Martínez L, Gallego-Villalobos M, Sáez-Comet L, Velilla-Marco J, Camps-García MT, de Ramón-Garrido E, Esteban Marcos EM, Pallarés-Ferreres L, Hidalgo-Tenorio C, Sabio-Sánchez JM, Gómez-de la Torre R, Salvador-Cervello G, Rios-Blanco JJ, Gil-Aguado A, Vilardell-Tarrés M (2012) Registry of the spanish network for systemic sclerosis: clinical pattern according to cutaneous subsets and immunological status. Semin Arthritis Rheum 41:789–800
Maricq HR, LeRoy EC, D’Angelo WA, Medsger TA Jr, Rodnan GP, Sharp GC, Wolfe JF (1980) Diagnostic potential of in vivo capillary microscopy in scleroderma and related disorders. Arthritis Rheum 23(2):183–189
Hachulla E, Gressin V, Guillevin L, Carpentier P, Diot E, Sibilia J, Kahan A, Cabane J, Francès C, Launay D, Mouthon L, Allanore Y, Tiev KP, Clerson P, de Groote P, Humbert M (2005) Early detection of pulmonary arterial hypertension in systemic sclerosis: a French nationwide prospective multicenter study. Arthritis Rheum 52:3792–3800
Traub YM, Shapiro AP, Rodnan GP, Medsger TA, McDonald RH Jr, Steen VD, Osial TA Jr, Tolchin SF (1985) Hypertension and renal failure (scleroderma renal crisis) in progressive systemic sclerosis. Medicine (Baltimore) 62:335–352
Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R, Dallongeville J, De Backer G, Ebrahim S, Gjelsvik B, Herrmann-Lingen C, Hoes A, Humphries S, Knapton M, Perk J, Priori SG, Pyorala K, Reiner Z, Ruilope L, Sans-Menendez S, Op Reimer WS, Weissberg P, Wood D, Yarnell J, Zamorano JL, Walma E, Fitzgerald T, Cooney MT, Dudina A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Funck-Brentano C, Filippatos G, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Altiner A, Bonora E, Durrington PN, Fagard R, Giampaoli S, Hemingway H, Hakansson J, Kjeldsen SE, Larsen ML, Mancia G, Manolis AJ, Orth-Gomer K, Pedersen T, Rayner M, Ryden L, Sammut M, Schneiderman N, Stalenhoef AF, Tokgözoglu L, Wiklund O, Zampelas A (2007) European guidelines on cardiovascular disease prevention in clinical practice: full text: fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur J Cardiovasc Prev Rehabil 14(Suppl 2):S1–113
Allanore Y, Meune C, Vonk MC, Airo P, Hachulla E, Camaraschi P, Riemekasten G, Cozzi F, Beretta L, Derk CT, Komócsi A, Farge D, Balbir A, Riccieri V, Distler O, Chialà A, Del Papa N, Simic KP, Ghio M, Stamenkovic B, Rednic S, Host N, Pellerito R, Zegers E, Kahan A, Walker UA, Matucci-Cerinic M, EUSTAR co-authors (2010) Prevalence and factors associated with left ventricular dysfunction in the EULAR Scleroderma Trial and Research group (EUSTAR) database of patients with systemic sclerosis. Ann Rheum Dis 69:218–221
Castell J, Fraile M, Candell J, Simeón CP, Fonollosa V, Alonso F, Armadans V (1992) Myocardial perfusion imaging in scleroderma and Raynaud’s phenomenon. Eur J Nucl Med 19:660
Candell-Riera J, Armadans-Gil L, Simeón CP, Castell-Conesa J, Fonollosa-Pla V, Garcia-Del-Castillo H, Vaqué-Rafart J, Vilardell M, Soler-Soler J (1996) Comprehensive noninvasive assessment of cardiac involvement in limited systemic sclerosis. Arthritis Rheum 39:1138–1145
Plastiras SC, Toumanidis ST (2012) Systemic sclerosis: the heart of the matter. Hellenic J Cardiol 53:287–300
Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, Strömberg A, van Veldhuisen DJ, Atar D, Hoes AW, Keren A, Mebazaa A, Nieminen M, Priori SG, Swedberg K, ESC Committeefor Practice Guidelines (CPG) (2008) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the task force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology: developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J 29(19):2388–2442
Ioannidis JP, Vlachoyiannopoulos PG, Haidich AB, Medsger TA Jr, Lucas M, Michet CJ, Kuwana M, Yasuoka H, van den Hoogen F, Te Boome L, van Laar JM, Verbeet NL, Matucci-Cerinic M, Georgountzos A, Moutsopoulos HM (2005) Mortality in systemic sclerosis: an international meta-analysis of individual patient data. Am J Med 118:2–10
Komócsi A, Vorobcsuk A, Faludi R, Pintér T, Lenkey Z, Költo G, Czirják L (2012) The impact of cardiopulmonary manifestations on the mortality of SSc: a systematic review and meta-analysis of observational studies. Rheumatology (Oxford) 51:1027–1036
Walker UA, Tyndall A, Czirják L, Denton C, Farge-Bancel D, Kowal-Bielecka O, Müller-Ladner U, Bocelli-Tyndall C, Matucci-Cerinic M (2007) Clinical risk assessment of organ manifestations in systemic sclerosis: a report from the EULAR Scleroderma Trials And Research group database. Ann Rheum Dis 66:754–763
Steen VD (2008) The many faces of scleroderma. Rheum Dis Clin North Am 34(1):1–15
Elhai M, Avouac J, Walker UA, Matucci-Cerinic M, Riemekasten G, Airò P, Hachulla E, Valentini G, Carreira PE, Cozzi F, Balbir Gurman A, Braun-Moscovici Y, Damjanov N, Ananieva LP, Scorza R, Jimenez S, Busquets J, Li M, Müller-Ladner U, Kahan A, Distler O, Allanore Y, EUSTAR co-authors (2014) A gender gap in primary and secondary heart dysfunctions in systemic sclerosis: a EUSTAR prospective study. Ann Rheum Dis. doi:10.1136/annrheumdis-2014-206386
Faccini A, Franchini S, Sabbadini MG, Camici PG (2014) Cardiac involvement at rest in patients with systemic sclerosis: differences between the limited and the diffuse form of the disease. G Ital Cardiol (Rome). 15(1):44–50
de Groote P, Gressin V, Hachulla E, Carpentier P, Guillevin L, Kahan A, Cabane J, Francès C, Lamblin N, Diot E, Patat F, Sibilia J, Petit H, Cracowski JL, Clerson P, Humbert M, Investigators ItinerAIR-Scleroderma (2008) Evaluation of cardiac abnormalities by Doppler echocardiography in a large nationwide multicentric cohort of patients with systemic sclerosis. Ann Rheum Dis 67:31–36
Faludi R, Költő G, Bartos B, Csima G, Czirják L, Komócsi A (2014) Five-year follow-up of left ventricular diastolic function in systemic sclerosis patients: determinants of mortality and disease progression. Semin Arthritis Rheum 44:220–227
Parks JL, Taylor MH, Parks LP, Silver RM (2014) Systemic sclerosis and the heart. Rheum Dis Clin North Am 40:87–102
Draeger HT, Assassi S, Sharif R, Gonzalez EB, Harper BE, Arnett FC, Manzoor A, Lange RA, Mayes MD (2013) Right bundle branch block: a predictor of mortality in early systemic sclerosis. PLoS ONE 8(10):e78808
Ferri C, Valentini G, Cozzi F, Sebastiani M, Michelassi C, La Montagna G, Bullo A, Cazzato M, Tirri E, Storino F, Giuggioli D, Cuomo G, Rosada M, Bombardieri S, Todesco S, Tirri G, Systemic Sclerosis Study Group of the Italian Society of Rheumatology (SIR-GSSSc) (2002) Systemic sclerosis: demographic, clinical, and serologic features and survival in 1012 Italian patients. Medicine (Baltimore) 81:139–153
Steen VD, Medsger TA (2007) Changes in causes of death in systemic sclerosis 1972–2002. Ann Rheum Dis 66:940–944
Tyndall AJ, Bannert B, Vonk M, Airò P, Cozzi F, Carreira PE, Bancel DF, Allanore Y, Müller-Ladner U, Distler O, Iannone F, Pellerito R, Pileckyte M, Miniati I, Ananieva L, Gurman AB, Damjanov N, Mueller A, Valentini G, Riemekasten G, Tikly M, Hummers L, Henriques MJ, Caramaschi P, Scheja A, Rozman B, Ton E, Kumánovics G, Coleiro B, Feierl E, Szucs G, Von Mühlen CA, Riccieri V, Novak S, Chizzolini C, Kotulska A, Denton C, Coelho PC, Kötter I, Simsek I, de la Pena Lefebvre PG, Hachulla E, Seibold JR, Rednic S, Stork J, Morovic-Vergles J, Walker UA (2010) Causes and risk factors for death in systemic sclerosis: a study from the EULAR Scleroderma Trials and Research (EUSTAR) database. Ann Rheum Dis 69:1809–1815
Elhai M, Meune C, Avouac J, Kahan A, Allanore Y (2012) Trends in mortality in patients with systemic sclerosis over 40 years: a systematic review and meta-analysis of cohort studies. Rheumatology (Oxford) 51:1017–1026
Rubio-Rivas M, Royo C, Simeón CP, Corbella X, Fonollosa V (2014) Mortality and survival in systemic sclerosis: systematic review and meta-analysis. Semin Arthritis Rheum 44(2):208–219
Acknowledgments
We would like to thank Dr. Jaume Candell-Riera (Cardiology Department, Vall d’Hebron University Hospital, Universitat Autònoma de Barcelona, Barcelona, Spain) for his substantial contributions to this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors state that they have no conflict of interest and that no financial support was received to make this manuscript.
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s00296-016-3470-y.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Figure 4
Kaplan Meier curves and hazard ratios for survival depending on cardiac involvement in patients diagnosed with SSc before 1990. Survival probability and the number of participants who were at risk at the beginning of each interval are shown below the graph. (TIFF 6172 kb)
Figure 5
Kaplan Meier curves and hazard ratios for survival depending on cardiac involvement in patients diagnosed with SSc after 1990. Survival probability and the number of participants who were at risk at the beginning of each interval are shown below the graph (TIFF 6160 kb)
Figure 6
Kaplan Meier curves and hazard ratios for survival in patients with SSc diagnosed before 1990 and cardiac involvement divided by cutaneous subsets. Survival probability and the number of participants who were at risk at the beginning of each interval are shown below the graph. (TIFF 6162 kb)
Figure 7
Kaplan Meier curves and hazard ratios for survival in patients with SSc diagnosed after 1990 and cardiac involvement divided by cutaneous subsets. Survival probability and the number of participants who were at risk at the beginning of each interval are shown below the graph. (TIFF 6151 kb)
Figure 8
Kaplan Meier curves for the rate of developing cardiac involvement since the onset of SSc divided by cutaneous subsets in patients diagnosed with SSc before 1990. Survival probability and the number of participants who were at risk at the beginning of each interval are shown below the graph. (TIFF 6197 kb)
Figure 9
Kaplan Meier curves for the rate of developing cardiac involvement since the onset of SSc divided by cutaneous subsets in patients diagnosed with SSc after 1990. Survival probability and the number of participants who were at risk at the beginning of each interval are shown below the graph. (TIFF 6194 kb)
Rights and permissions
About this article
Cite this article
Fernández-Codina, A., Simeón-Aznar, C.P., Pinal-Fernandez, I. et al. Cardiac involvement in systemic sclerosis: differences between clinical subsets and influence on survival. Rheumatol Int 37, 75–84 (2017). https://doi.org/10.1007/s00296-015-3382-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-015-3382-2