Abstract
We hypothesized that serum urate-associated SNPs, individually or collectively, interact with BMI and renal disease to contribute to risk of incident gout. We measured the incidence of gout and associated comorbidities using the original and offspring cohorts of the Framingham Heart Study. We used direct and imputed genotypes for eight validated serum urate loci. We fit binomial regression models of gout incidence as a function of the covariates, age, type 2 diabetes, sex, and all main and interaction effects of the eight serum urate SNPs with BMI and renal disease. Models were also fit with a genetic risk score for serum urate levels which corresponds to the sum of risk alleles at the eight SNPs. Model covariates, age (P = 5.95E−06), sex (P = 2.46E−39), diabetes (P = 2.34E−07), BMI (P = 1.14E−11) and the SNPs, rs1967017 (P = 9.54E−03), rs13129697 (P = 4.34E−07), rs2199936 (P = 7.28E−03) and rs675209 (P = 4.84E−02) were all associated with incident gout. No BMI by SNP or BMI by serum urate genetic risk score interactions were statistically significant, but renal disease by rs1106766 was statistically significant (P = 6.12E−03). We demonstrated that minor alleles of rs1106766 (intergenic, INHBC) were negatively associated with the risk of incident gout in subjects without renal disease, but not for individuals with renal disease. These analyses demonstrate that a significant component of the risk of gout may involve complex interplay between genes and environment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of gout and hyperuricemia in the USA is increasing due partly to changing population age structure and increasing obesity rates [1–3]. Many large-effect genetic risk factors for gout and hyperuricemia are known from GWAS studies, including SLC2A9 and ABCG2, which encode proteins important for urate reabsorption and excretion in the kidney [4, 5]. Hypertension and diuretic use are also risk factors for gout [6, 7]. These observations have stimulated the analysis of interactions between environmental risk factors involving renal function and serum urate genes and their association with gout [8]. Diuretic use has been associated with increased gout risk of individuals homozygous for validated hyperuricemia risk alleles SLC2A9 (rs13129697) and SLC22A11 (rs2078267) [8]. However, the same interaction was not found using a sample from the Nurses Health Study [9]. It is well known that gene–environment interactions are dynamic and with allele frequencies and exposures may vary among populations [10]. Therefore, the interpretation of gene–environment interactions can be difficult. Nevertheless, studies of gene–environment interactions can provide more complete knowledge of associations of environmental exposures and disease and add to our understanding of disease mechanisms [11].
A number of environmental risk factors, most interrelated, associated with gout and hyperuricemia are increasing in prevalence. Diet [12, 13] and traits associated with the metabolic syndrome, including hypertension, high body mass index (BMI) and type 2 diabetes, are also associated with increased serum urate and gout risk [14]. Reduced renal function is associated with gout. Results from the Atherosclerosis Risk in Communities Study (ARIC) showed that low glomerular filtration rate (GFR) was highly associated with incident gout. This result was abrogated when serum urate was included in the multivariable model reflecting the known link between reduced kidney function (whether due to hypertension, or other causes), urate excretion, hyperuricemia and gout risk [6].
In this study, we tested the hypothesis that particular genotype–environment interactions are important risk factors for gout. We report novel findings from analysis of the Framingham Heart Study (FHS) cohorts documenting BMI and renal disease interactions with each of eight validated serum urate loci. We also present results of the interactions of BMI and renal disease with a genetic risk score (GRS) representing the cumulative genetic risk with gout across the eight validated serum urate loci [4].
Methods
Clinical variables
The current study was performed using the original and offspring cohorts of the FHS [15]. These cohorts represent the age distribution for reasonable estimates of incident gout, whereas the third generation cohort is much younger, with gout prevalence much lower than observed in the normal population. Incident gout was defined as the presence of a clinical diagnosis of gout where none was present in any prior examination. Gout has been similarly defined and used in numerous published studies from the FHS, e.g., [16–19]. Sex of the subject was noted. Last age known (years) is the age at last follow-up and controls for exposure, or variable observation times to each subject. Type 2 diabetes was defined as present for each subject by searching examinations for patient history of diabetes. Hypertension in gout patients was defined as present for those with systolic or diastolic measurement higher or equal to 140 and 90 mmHg, respectively, at any examination up to gout diagnosis, and for non-gout subjects across all examinations. BMI in gout patients was taken from examination at gout diagnosis and for non-gout subjects, the BMI at the last record. Renal disease at gout was defined as present for individuals with gout if clinical impression of renal disease was recorded at any examination up to gout diagnosis and for non-gout subjects, across all examinations. In addition, the last creatinine measurement was recorded before gout diagnosis or, for non-gout subjects, the last recorded creatinine measurement. These values were used to compute another objective measure of chronic kidney disease (CKD), eGFR. Individuals with eGFR <90 were defined as stage 2 CKD or greater. All variables are defined in detail including the dbGaP accession number in the supplemental materials.
Genetic data
Genetic data for the two cohorts were initially obtained from the Affymetrix 6.0 gene array. Only two SNPs, rs1165196 and rs1106766, were directly genotyped. The other six SNPs, rs1967017, rs780093, rs13129697, rs2199936, rs675209 and rs2078267 were imputed with IMPUTE2, using the 1000 genomes as reference data [20]. Prior to imputation, standard quality control measured was used to eliminate poorly genotyped SNPs and individuals. All eight SNPs had “info” (imputation quality) scores >0.8, indicating a high level of statistical confidence in these imputed genotypes [21]. There were 5109 genotyped individuals with non-missing clinical variables in the sample.
Data analysis
The general modeling strategy was to fit binomial regression models of gout incidence conditional on genetic and environmental covariates and their interactions. A major strength of our approach is the longitudinal nature of the FHS data, as we measured comorbidities as they occurred prior to gout diagnosis. By contrast, in a cross-sectional analysis the chronology of the outcome of interest and its comorbidities is unknown. For example, to estimate a BMI–urate SNP interaction effect, we observed BMI at gout and tested whether the allele frequency difference varied between gout and non-gout cases as a function of BMI. For non-gout cases, the comorbidities and environmental exposures were assessed across all examinations. We evaluated the comorbidities at the last examination time and at the time of maximum BMI of the non-gout cases. Results were similar and we only present results of the last examination time. To test hypotheses related to interaction effects of urate SNPs with BMI and renal disease, we fit six models of gout incidence with relevant covariates and additive genetic effects of the urate SNPs as described below. The analysis approach is depicted in Fig. 1.
Additive model (1)
We modeled the probability of incident gout, using the logit link, as a function of clinical and demographic variables and the eight urate SNPs:
where η i is a linear predictor for subject i of the form,
β 0 is an intercept common to all subjects and p is the number of covariates. The p covariates are as follows: age at last examination, sex, diabetes (Y/N), renal disease (Y/N), hypertension (Y/N), BMI, and the count of copies of reference alleles associated with increased serum urate rs1967017, rs780093, rs13129697, rs2199936, rs675209, rs1165196, rs2078267, rs1106766 accordingly to Yang et al. [4]. In the case of the SNP covariates, the count will yield {x ij = 0, 1, 2} for the ith individual jth covariate. If the SNP was imputed, then the posterior probability weighted by expected number of alleles was used as the allele count.
BMI–SNP interaction model (2)
The additive model (1) was extended by adding eight interaction effects of BMI with each SNP.
RD–SNP interaction model (3)
The additive model (1) was extended by incorporating interaction effects of renal disease and the eight SNPs.
Fitting models with genetic risk score
For every person, we counted number of risk alleles present (the eight urate SNPs) creating a new variable, GRS. For the GRS calculation, reference alleles for all SNPs were used such that increasing dosages of the alleles increased risk of incident gout. In addition, a weighted genetic urate score (GUSw) was calculated in which each SNP was multiplied by its effect on serum urate. The eight SNPs, risk alleles and effect sizes were obtained from Yang et al. [4] a meta-analysis of the CHARGE cohorts.
GRS model (4)
We refit our additive model (1), but replacing the eight SNPs with the GRS variable.
BMI–GRS model (5)
The GRS model was extended by adding an interaction term BMI by GRS.
RD–GRS model (6)
The GRS model was extended by adding the interaction term of renal disease by GRS.
Tests of individual effects from models 1 to 4 were one degree of freedom (1 df) tests whose P values were obtained by the change in deviance (−2 × log likelihood) between the full model and a reduced model without the focal parameter. The test statistics for BMI and renal disease by genetic interactions were calculated as the change in model deviance between models 2 and 1, and models 3 and 1 and are distributed as χ 2 with df = 8. The corresponding test statistics for the GUS models 4 and 5 and models 4 and 6 have 1 df. For the eight df interaction effect tests, we considered the P value significant at the α = 0.05 level. For the 1 df tests of specific gene by environment interactions, P values less than the Bonferroni corrected α level of 6.25E−03 were considered highly significant. All models were fit using the “glm” function in R with logit link function [22]. All tests of significance were performed with log-likelihood ratio tests (LRT) implemented using the “anova” function in R.
Results
The total number of individuals analyzed in the study was 5097. We identified 423 incident gout cases from the original and offspring cohorts with available genetic data (Table 1). Gout patients had a mean age of 77.4 years and mean BMI of 29 kg/m2; 74 % were men, 26 % had diabetes, 61 % had hypertension, and 42 % had renal disease. The total number of individuals for which eGFR was computed was 3687. An eGFR <90 was only available for five incident gout cases with genetic data, and thus, we did not fit genetic models to these data. Non-gout patients differed from gout patients in all but one of these measures (Table 1). In univariate models, age, sex, BMI, type 2 diabetes, eGFR and hypertension were all significantly associated with gout, but a clinical diagnosis of renal disease was not (Table 1).
Hypothesis tests of model 1 demonstrated that the covariates, age (P = 5.95E−06), sex (P = 2.46E−39), BMI (P = 1.14E−11) and diagnosis of diabetes (P = 2.34E−07), were all significantly associated with the risk of gout (Table 2). Hypertension and renal disease were not statistically significantly associated with gout in the multivariable model. Four out of the eight serum urate-associated SNPs were significantly (α level = 0.05) associated with incident gout in the multivariate model: rs1967017 (P value = 6.79E−03), rs13129697 (P value = 4.13E−07), rs2199936 (P value = 1.76E−03) and rs675209 (P value = 2.34E−02) (Table 2).
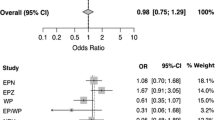
LRT (model 1 vs model 2) demonstrated that interaction effects of these eight SNPs and BMI do not appear to be important explanatory variables for gout incidence (χ 2 = 8.3, df = 8, P value = 0.40). In addition, model 2 was refit with BMI as a dichotomous variable (BMI <30 = 0, BMI ≥30 = 1), and in this case, the deviance of the model exceeded that of model 1 (data analysis not shown). The RD-SNP interaction model (model 3) was significantly different than model 1 (χ 2 = 15.86, df = 8, P value = 4.44E−02) indicating at least one statistically significant interaction effect. A 1 df LRT demonstrated that a single interaction effect, renal disease by rs1106766, was statistically significant (P value = 6.12E−03) (Table 2).
The interaction of renal disease and the INBHC SNP, rs1106766 (OR 1.8, 95 % CI 1.2, 2.7), was visualized by plotting its minor allele frequency in cases and controls by categories of renal disease. As seen in Fig. 2, there is no genetic risk of gout at this locus among individuals with renal disease; however, there is a negative genetic risk of gout (“protective” effect of the INBHC locus), among individuals without renal disease. Based on the frequencies of this SNP observed among those without gout, we would have expected a much lower frequency among incident gout cases with renal disease than that which was observed (0.21).
Hypothesis tests of the GRS model, in which an unweighted GRS replaced the individual SNP markers, demonstrated that the GRS alone was significantly associated with gout incidence (P = 1.54E−08) (Table 3). The BMI-GRS interaction was not a significant explanatory variable for gout risk (model 5 vs model 4), but the renal disease–GRS interaction was statistically significant (model 6 vs model 4; P = 3.2E−03). These results generally mirror the results from models 1 to 3. Models 4–6 were also fit using GUSw, and hypothesis tests of the weighted GUS effect, the BMI by GUS and the renal disease by GUS interaction resulted in P values that were highly similar to models fit with the unweighted GUS (Table 3).
Discussion
In this study, we tested the hypothesis that environmental factors affecting serum urate and genetic loci for serum urate concentration may exhibit context-dependent associations with the risk of developing gout. Genes encoding urate transporters have been consistently associated with serum urate concentration and gout in population-based studies [4, 5]. Two loci alone, SLC2A9 and ABCG2, which are the only loci genome-wide significant for gout, account for 50 % of the variance in serum urate explained by the 26 replicated loci identified from GWAS (total variance explained by all loci is 7 %) [5]. The directions of the effect sizes of SNPs for serum urate concentration are consistent with the magnitudes of OR’s observed for gout [5]. We hypothesized that BMI and renal disease, both associated with hyperuricemia, may mask or accentuate the associations of the SNPs with gout. For example, high BMI, perhaps a result of lifestyle or diet, and associated increased serum urate concentration, may increase risk of developing gout, but only when combined with genotypes associated with high serum urate. Therefore, our approach seeks to further our understanding of the environmental sources of variation for gout, mediated by serum urate loci, with implications for gout’s pathogenesis.
We found support for the hypothesis that renal disease and urate-associated SNPs were also non-additive sources of variation for gout risk. BMI and urate SNPs were both highly associated with gout risk, but BMI by urate SNP interaction effects were not. Results from the main effects model demonstrated that neither rs1106776 (INHBC) nor renal disease were statistically significant risk factors for incident gout. However, the INBHC risk with gout appears contextual given the presence of renal disease. Among individuals without renal disease, the INHBC SNP was protective, but there was no protective association evident at this locus for individuals with renal disease. The INHBC SNP has not been validated in GWAS meta-analyses as a genetic risk factor for gout at genome-wide α levels [5]. Interestingly, in New Zealanders of European and Polynesian ancestry, the effect for gout, in rigorously phenotyped cohorts, appears reversed [23]. It is conceivable that renal disease, which reverses rs1106776’s lowered gout risk observed among those with normal renal function, is masking INHBC’s effects on gout from the GWAS meta-analyses. For complex diseases such as gout, more modest genetic effects may frequently be overlooked especially if pervasive genetic and environmental correlation for gout comorbidities exist and obscure findings from simple models of trait-SNP associations.
The role of the renal disease exposure appears to be mediating the direction and magnitude of the SNP’s effect on gout away from that expected based on the SNP’s association with serum urate. We demonstrated that renal disease and urate risk SNPs as a whole contribute to gout risk. Indeed, the interaction of renal disease and the GRS was a significant source of gout risk. However, these context-dependent genetic effects were not observed at all the urate-associated loci. LRT demonstrated that only 1 out of 8 of the individual effects was statistically significant (rs1106766). The renal disease by SNP interaction effects just described involve genetic loci of much more modest effect together explaining <0.3 % of the variance in urate concentration [4, 5]. These results suggest that gout comorbidities related to kidney function can mediate the distribution of genetic effects on gout.
It is possible that the same loci associated with gout are also associated with its comorbidities, i.e., the variables considered environmental mediators are themselves genetically correlated with the outcome of interest. For example, the INHBC locus has been found to be associated with eGFR [24]. The SLC2A9 and ABCG2 loci together explain 3.4 % of the variance in serum urate concentration and are the only validated gout risk loci at genome-wide α level [5]. SLC2A9 and ABCG2 have known functional roles in serum urate concentration and gout risk and also have indirect negative effects on GFR and serum creatinine and thus renal function [25]. It appears then that there is positive genetic correlation due to pleiotropy between renal disease and gout at these loci. However, we were not able to find statistically significant main effects of rs13129697 (SLC2A9) or rs2199936 (ABCG2) on renal disease (data not shown) nor did we find interaction effects for gout involving the SLC2A9 and ABCG2 SNPs with BMI or renal disease. In addition, no SNP tested in this study was known to have an association with BMI [26]. Nevertheless, the multivariable models we used to test for significant interactions between the SNPs and genetically correlated exposures could be limited if the genetic effect of the exposure on gout nullifies the SNP’s effect and its interaction. These observations suggest that it would be interesting to study the pairwise genetic correlations of gout comorbidities especially if the results improve the estimates of genetic risk of the disease.
We acknowledge several limitations of the study. First, our measure of renal disease, a clinical diagnostic impression, does not include objective measures of renal function. In this study, we were not able to make a strong link between our eGFR variable and renal disease, which could be due to a mismatch between the time points of creatinine measurement and clinical diagnostic impression of renal disease. However, the results are hypothesis generating and call for future studies of genetic associations with gout and renal function in well-phenotyped prospective studies.
We used measures of incident gout, thus allowing an accurate assessment of risk associated with gout comorbidities. We were not able to establish that BMI, a known risk factor for gout and hyperuricemia, and urate loci interact in their association with gout risk. We were able to conclude that some genetic risk of gout seems to be context dependent on normal kidney function. Finally, we conclude that future studies of gout risk prediction should include multivariate models of genetic and environmental correlations to better understand the connections between gout comorbidities and their joint effects on gout risk.
References
Arromdee E, Michet CJ, Crowson CS et al (2002) Epidemiology of gout: is the incidence rising? J Rheumatol 29:2403–2406
Lawrence RC, Felson DT, Helmick CG et al (2008) Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum 58:26–35
Roddy E, Choi HK (2014) Epidemiology of gout. Rheum Dis Clin N Am 40:155–175
Yang Q, Köttgen A, Dehghan A et al (2010) Multiple genetic loci influence serum urate levels and their relationship with gout and cardiovascular disease risk factors. Circ Cardiovasc Genet 3:523–530
Köttgen A, Albrecht E, Teumer A et al (2013) Genome-wide association analyses identify 18 new loci associated with serum urate concentrations. Nat Genet 45:145–154
McAdams-DeMarco MA, Maynard JW, Baer AN et al (2012) Hypertension and the risk of incident gout in a population-based study: the atherosclerosis risk in communities cohort. J Clin Hypertens 14:675–679
McAdams DeMarco MA, Maynard JW, Baer AN et al (2012) Diuretic use, increased serum urate levels, and risk of incident gout in a population-based study of adults with hypertension: the Atherosclerosis Risk in Communities cohort study. Arthritis Rheum 64:121–129
McAdams-DeMarco MA, Maynard JW, Baer AN et al (2013) A urate gene-by-diuretic interaction and gout risk in participants with hypertension: results from the ARIC study. Ann Rheum Dis 72:701–706
Bao Y, Curhan G, Merriman T et al (2015) Lack of gene–diuretic interactions on the risk of incident gout: the Nurses’ Health Study and Health Professionals Follow-up Study. Ann Rheum Dis 74:1394–1398
Aschard H, Lutz S, Maus B et al (2012) Challenges and opportunities in genome-wide environmental interaction (GWEI) studies. Hum Genet 131:1591–1613
Hunter DJ (2005) Gene–environment interactions in human diseases. Nat Rev Genet 6:287–298
Choi HK, Atkinson K, Karlson EW et al (2004) Alcohol intake and risk of incident gout in men: a prospective study. Lancet 363:1277–1281
Choi HK, Atkinson K, Karlson EW et al (2004) Purine-rich foods, dairy and protein intake, and the risk of gout in men. N Engl J Med 350:1093–1103
Choi HK, Ford ES, Li C et al (2007) Prevalence of the metabolic syndrome in patients with gout: the Third National Health and Nutrition Examination Survey. Arthritis Rheum 57:109–115
Dawber TR, Meadows GF, Moore FEJ (1951) Epidemiological approaches to heart disease: the Framingham Study. Am J Public Health Nations Health 41:279–286
Wang W, Bhole VM, Krishnan E (2015) Chronic kidney disease as a risk factor for incident gout among men and women: retrospective cohort study using data from the Framingham Heart Study. BMJ Open 5:e006843
Wang W, Krishnan E (2015) Cigarette smoking is associated with a reduction in the risk of incident gout: results from the Framingham Heart Study original cohort. Rheumatology 54:91–95
Rasheed H, Phipps-Green A, Topless R et al (2013) Association of the lipoprotein receptor-related protein 2 gene with gout and non-additive interaction with alcohol consumption. Arthritis Res Ther 15:R177
Krishnan E (2012) Gout and the risk for incident heart failure and systolic dysfunction. BMJ Open 2:e000282
Howie B, Marchini J, Stephens M (2011) Genotype imputation with thousands of genomes G3(1):457–470
Marchini J, Howie B (2010) Genotype imputation for genome-wide association studies. Nat Rev Genet 11:499–511
R Development Core Team (2009) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Phipps-Green AJ, Merriman ME, Topless R et al (2014) Twenty-eight loci that influence serum urate levels: analysis of association with gout. Ann Rheum Dis. doi:10.1136/annrheumdis-2014-205877
Chasman DI, Fuchsberger C, Pattaro C et al (2012) Integration of genome-wide association studies with biological knowledge identifies six novel genes related to kidney function. Hum Mol Genet 21:5329–5343
Hughes K, Flynn T, de Zoysa J et al (2014) Mendelian randomization analysis associates increased serum urate, due to genetic variation in uric acid transporters, with improved renal function. Kidney Int 85:344–351
Speliotes EK, Willer CJ, Berndt SI et al (2010) Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat Genet 42:937–948
Grant support
This study was supported by K01 AR060848 (R.J.R.) and P30 DK056336 (D.B.A., A.I.V.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Y.C.K. was supported by NIH grant K01 DK095032. A.I.V. was supported by R01 DK062148. J.A.S. is supported by grants from the Agency for Health Quality and Research Center for Education and Research on Therapeutics (AHRQ CERTs) U19 HS021110, National Institute of Arthritis, Musculoskeletal and Skin Diseases (NIAMS) P50 AR060772 and U34 AR062891, National Institute on Aging (NIA) U01 AG018947, National Cancer Institute (NCI) U10 CA149950, the resources and the use of facilities at the VA Medical Center at Birmingham, Alabama and research contract CE-1304-6631 from the Patient Centered Outcomes Research Institute (PCORI). The Framingham Heart Study is conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with Boston University (Contract No. N01-HC-25195). This manuscript was not prepared in collaboration with investigators of the Framingham Heart Study and does not necessarily reflect the opinions or views of the Framingham Heart Study, Boston University, or NHLBI. Funding for SHARe Affymetrix genotyping was provided by NHLBI Contract N02-HL-64278. SHARe Illumina genotyping was provided under an agreement between Illumina and Boston University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J.A.S. has received research grants from Takeda and Savient and consultant fees from Savient, Takeda, Regeneron and Allergan. J.A.S. is a member of the executive of OMERACT, an organization that develops outcome measures in rheumatology and receives arms-length funding from 36 companies; a member of the American College of Rheumatology’s Guidelines Subcommittee of the Quality of Care Committee; and a member of the Veterans Affairs Rheumatology Field Advisory Committee. Dr. Allison has received grants, donations, or consulting fees from Pfizer, Arena and Eisai pharmaceuticals.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Reynolds, R.J., Vazquez, A.I., Srinivasasainagendra, V. et al. Serum urate gene associations with incident gout, measured in the Framingham Heart Study, are modified by renal disease and not by body mass index. Rheumatol Int 36, 263–270 (2016). https://doi.org/10.1007/s00296-015-3364-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-015-3364-4