Abstract
Chronic administration of colchicine remains a mainstay of therapy for patients with Familial Mediterranean Fever (FMF). As this medication is a strong CYP3A4 inhibitor, it has the potential to interact with many routinely used medications. One such medication is clarithromycin, itself a strong inhibitor of the same enzyme, and a typical choice for triple therapy eradication of H. pylori. Various sequelae of colchicine–clarithromycin interaction have been documented and can be expected by prescribing physicians, with rhabdomyolysis, though rare, being among the most serious. Review of cases from a tertiary academic medical center and full PubMed/MEDLINE literature review. Despite the prevalence of diseases treated with clarithromycin and the expected drug interaction with colchicine, only two cases in the literature document clinical rhabdomyolysis due to colchicine–clarithromycin interaction. In neither case, however, were patients undergoing treatment for FMF. Herein, we describe the first two cases in the literature of clinical rhabdomyolysis in FMF patients under colchicine therapy after administration of clarithromycin as part of therapy treating H. pylori infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Colchicine is a mainstay of therapy for patients with Familial Mediterranean Fever (FMF). Chronic administration of colchicine prevents the attacks of FMF, which typically consists of fever, peritonitis, pleuritis, and/or synovitis, and effectively reduces the risk of amyloidosis [1]. Similarly, colchicine is also used routinely in other pro-inflammatory states such as Behcet and gouty arthritis. Colchicine is metabolized via the enzyme CYP3A4 [2], in addition to being a substrate of the P-glycoprotein transporter system [3]. The typical toxidrome for colchicine poisoning consists of gastroenteritis, hypotension, lactic acidosis, and prerenal azotemia [4]. Although exceedingly rare in patients treated orally with maintenance doses, colchicine toxicity may cause considerable morbidity and even mortality due to severe pancytopenia and multiorgan failure [5–8]. Nevertheless, intoxication can occur during interaction with other medications that interfere with colchicine metabolism.
Helicobacter pylori (H. pylori) is a common disease in the USA, with a recent meta-analysis reporting a prevalence of up to 23.7 % [9]. Most cases of H. pylori infection are treated with a therapeutic regime that includes some form of gastric acid control alongside the macrolide antibiotic clarithromycin. Clarithromycin is a strong reversible inhibitor of the cytochrome P450 system [10], specifically CYP3A4, and has also been found to be a clinically important inhibitor of the P-glycoprotein transporter [11]. The combination of these metabolic properties creates the potential for interactions with concomitantly administered medications as a result of competition for common pathways of metabolism or excretion.
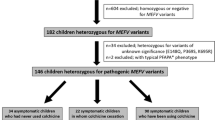
Despite the prevalence of diseases treated with clarithromycin and the expected drug interaction with colchicine, only eight publications documenting serious sequelae were found in our review of the literature [12–19]. The vast majority of these patients had impaired renal function, many were treated with colchicine for gout, and most presented with signs and symptoms consistent with acute colchicine toxicity. Two patients were under treatment with colchicine for FMF, although they too presented with typical colchicine toxicity. Conversely, clinical rhabdomyolysis due to colchicine–clarithromycin interaction was reported in only two cases, wherein patients had been treated chronically with colchicine for either gout [15] or Behcet [18]. Herein, we describe the first two cases in the literature of rhabdomyolysis in colchicine-treated FMF patients after administration of clarithromycin as part of combination therapy for H. pylori.
Case presentation
Case 1
A 43-year-old man presented to the ER complaining of myalgia. He has a past medical history of FMF, diagnosed in childhood, and manifested with periodic bouts of fever, abdominal pain, and arthritis. His disease had been well controlled for the previous 3 years under treatment with colchicine 0.5 mg TID. Sixteen days prior to current admission, the patient was started on triple therapy (clarithromycin, amoxicillin, omeprazole) after gastroenterological workup for H. pylori. A week prior to admission, the patient began experiencing vomiting and diarrhea, which progressed to include myalgias of the hand and feet and generalized weakness. At this point in our evaluation, we suspected the patient was demonstrating typical symptoms of colchicine toxicity.
On admission, he was hemodynamically stable and afebrile. Physical exam was unremarkable save for diffuse muscle weakness. Laboratory studies revealed normal blood counts, normal urea and creatinine, CPK of 31,000 U/L, LDH of 1400 U/L, AST of 860 U/L, and an elevated urine myoglobin. EMG was performed without any gross findings, and he was subsequently diagnosed with rhabdomyolysis. All medications were halted, and aggressive treatment began with fluids and electrolytes. By day six of admission, the patient was without symptoms and CPK had normalized. He was subsequently discharged home with instructions to reintroduce colchicine in 1 week and follow up at the FMF center.
Case 2
A 52-year-old female was admitted to our hospital due to diarrhea, severe myalgia, and weakness. Her past medical history was significant for long-standing FMF treated with colchicine 1.5 mg per day. One week prior to admission, the patient started triple therapy (omeprazole, clarithromycin, and amoxicillin) for eradication of H. pylori after positive C14 urea breath test. Three days into her treatment, the patient began experiencing nonbloody diarrhea and nausea, followed by diffuse myalgias and weakness which increased in intensity as treatment continued. The patient presented 1 day after completing triple therapy regimen, and due to the constellation of her symptoms, we began investigation into possible colchicine toxicity.
Physical examination on admission revealed diffuse muscular tenderness without obvious weakness. No focal findings were present on abdominal examination. Laboratory studies showed a creatinine kinase of 1016 U/L, with CK-MB fraction of 5.6 %, lactate dehydrogenase level of 537 U/L, aspartate aminotransferase level of 105 U/L, and alanine aminotransferase level of 101 U/L. Blood count, creatinine, bilirubin, alkaline phosphatase, and thyroid-stimulating hormone levels were normal. Myoglobin was not detected in urine. With the diagnosis now shifted toward rhabdomyolysis, colchicine was withdrawn, and treatment began with intravenous fluids and electrolyte replacement. On the second day of admission, her CK, LDH, and AST levels peaked, reaching 2805 U/L (CK-MB fraction of 3.6 %), 806 U/L, and 173 U/L, respectively. Over the following 4 days, the patient’s weakness and myalgias persisted, and she began complaining of limb paresthesias. On day ten of admission, CPK and AST levels returned to normal limits. Colchicine treatment was resumed, and the patient discharged. One year later, the patient remains asymptomatic.
Discussion
Although rare in patients treated orally with maintenance, colchicine is well known for its classic toxidrome of gastroenteritis characterized by nausea, vomiting, and diarrhea. Cases of colchicine-induced myopathy and neuropathy have also been reported, however, mostly in patients with preexisting impairment in renal or liver function [20–22]. Additionally, the entity of colchicine-induced rhabdomyolysis has been well documented in several case reports [23–27], specifically with concomitant use of bezafibrate [28], gemfibrozil [29], and especially statins [29–34] and cyclosporine [35, 36]. Nevertheless, in a literature review of 82 documented cases of colchicine-induced myotoxicity, none were attributed to interaction with clarithromycin [22]. Further, the ability of omeprazole, amoxicillin, and/or clarithromycin in combination or alone to cause rhabdomyolysis is much less established, with only two case reports describing patients with rhabdomyolysis due to omeprazole [37, 38].
To the best of the authors’ knowledge, this article represents the only report of colchicine–clarithromycin-induced rhabdomyolysis in FMF patients. Colchicine is the first-line treatment of FMF in many countries and is a well-tolerated long-term therapy. Additionally, clarithromycin is considered the standard first-line treatment for H. pylori as part of the classic triple therapy. This article highlights a common clinical issue that of treatment for acute disease in the chronically ill. Both medication regimens can be first line for each of their respective pathologies, however, when combined, they should be used cautiously and alternatives should be considered. Pathophysiologically, these medications are just two of many which utilize common metabolic pathways; therefore, this interaction may be extrapolated to other medication combinations. Both medications represent the stereotypical strong dual-inhibitor (inhibiting both CYP3A4 and P-glycoprotein/ABCB1), which are common pathways for hepatic metabolism and are involved in many other drug interactions. Combination of colchicine and clarithromycin is categorized as risk D, necessitating a consideration of therapy modification in select patients. The increased levels of colchicine and resulting elevated distribution to tissues such as muscle, as caused by its interaction with clarithromycin, most likely represent the culprit of these acquired events of rhabdomyolysis. As both patients had previously normal hepatic and renal function, the combination could have been safely administered with a colchicine dose reduction.
To date, eight case studies have described colchicine intoxication in patients treated concomitantly with clarithromycin [12–19]. All patients had received maintenance doses of colchicine (range 1–1.5 mg/day) for treatment of FMF, gouty arthritis, or AA amyloidosis. The vast majority of cases described presentations of typical colchicine toxicity, manifesting as gastrointestinal symptoms (abdominal pain, vomiting, and diarrhea) shortly after concomitant administration of macrolides prescribed for management of a variety of conditions. Rollot et al. [13] described a 76-year-old patient with FMF on chronic colchicine therapy who had undergone H. pylori eradication therapy and subsequently presented with fever, abdominal pain, diarrhea, and later alopecia, attributed to colchicine intoxication. The patient’s symptoms were completely resolved after hydration and lowering of colchicine dose. Akdag et al. [16] described two patients with renal failure who developed colchicine toxicity due to combination with clarithromycin. van der Velden et al. [19] described acute neurotoxicity due to clarithromycin and colchicine in patient with renal failure treated with simvastatin. Cheng et al. [14] described two patients with fatal agranulocytosis attributed to a combination of clarithromycin and colchicine.
There is only one retrospective study on patients who were prescribed clarithromycin and colchicine during the same clinical admission [17]. Case–control comparisons were made between 116 patients who received concomitant two-drug therapy and patients who received sequential therapy. Assessment of the clinical presentations and outcomes of the two patient groups and analysis the risk factors associated with fatal outcomes was recorded. Nine (10.2 %) of the 88 patients who received concomitant two drugs died, and only 1 (3.6 %) of the 28 patients who received the drugs sequentially died. Multivariate analysis of the 88 patients who received concomitant therapy showed that longer overlapped therapy, the presence of baseline renal impairment, and the development of pancytopenia were independently associated with death. The authors concluded that these drugs should not be administered together.
As opposed to the previous cases that described classic symptoms of colchicine toxicity due colchicine–clarithromycin interactions, only two cases exist of patients suffering rhabdomyolysis. McKinnell et al. [15] described a 48-year-old patient on colchicine treatment for gout who developed rhabdomyolysis after beginning treatment with clarithromycin for pneumonia. Kim et al. [18] described colchicine-induced rhabdomyolysis caused by interaction with clarithromycin in a patient with Behcet disease. Both patients in our review carried the diagnosis of FMF and were treated with colchicine for many years without side effects until receiving triple combination therapy for the eradication of H. pylori. Initially, both our patients presented with symptoms concerning for acute colchicine toxicity, although their clinical picture progressed to rhabdomyolysis. These manifestations resolved promptly after the discontinuation of colchicine, the abnormal values of CK, LDH, AST, and ALT returned to normal levels. Both patients had normal kidney function at baseline, and neither presented with pancytopenia. The role of muscle biopsy in rhabdomyolysis has been discussed in a review article by Nance and Mammen [39]. The authors describe the test’s utility in revealing metabolic disturbances such as various mitochondrial diseases, enzyme deficiencies, fatty acid oxidation disorders, and glycogen storage diseases. The review highlights that muscle biopsy should be undertaken only after resolution of acute rhabdomyolysis to observe inherent underlying disease. In the cases presented in this article, muscle biopsies were not preformed as each represented an isolated event for the patients and a temporally related culprit for acquired disease had been identified; suspicion of rhabdomyolysis predisposing diseases, other than FMF and the drug interaction discussed, was very low.
As part of a broad differential to drug-related rhabdomyolysis, inherent myalgias of FMF must be considered. Rigante et al. [40] have discussed this topic in a review highlighting noncanonical manifestation of FMF. These myalgias may be divided into three categories: spontaneous, exercise-induced, or protracted (which have been associated with various vasculitides and infections). Nonetheless, a temporal association between the combination therapy initiation and the onset of myopathy in our patients whom had been treated uneventfully with colchicine for a long time strongly suggests an interaction between colchicine and one of the drugs the patient received for the eradication of H. pylori. To date, no interactions between omeprazole and colchicine or amoxicillin and colchicine have been reported in the literature. Our case report is the first to describe rhabdomyolysis due to colchicine–clarithromycin interaction in FMF patients with normal renal functions. Both patients received clarithromycin as part of the triple therapy for eradication of H. pylori. We hypothesize that clarithromycin brought about toxic levels of colchicine on the basis of its ability to inhibit CYP3A4 and the P-glycoprotein transport system. Previous reports of colchicine intoxication in patients treated with macrolide antibiotics concur with our assumption. Triple combination therapy for eradication of H. pylori including clarithromycin is frequently prescribed. Physicians should be aware of interaction-induced rhabdomyolysis in FMF patients under stable long-term management with colchicine when considering antibiotic treatment with clarithromycin.
Abbreviations
- FMF:
-
Familial Mediterranean Fever
- H. pylori :
-
Helicobacter pylori
References
Zemer D, Pras M, Sohar E, Modan M, Cabili S, Gafni J (1986) Colchicine in the prevention and treatment of the amyloidosis of familial Mediterranean fever. New Engl J Med 314(16):1001–1005
Tateishi T, Soucek P, Caraco Y, Guengerich FP, Wood AJ (1997) Colchicine biotransformation by human liver microsomes. Identification of CYP3A4 as the major isoform responsible for colchicine demethylation. Biochem Pharmacol 53(1):111–116
Schinkel AH, Jonker JW (2003) Mammalian drug efflux transporters of the ATP binding cassette (ABC) family: an overview. Adv Drug Deliv Rev 55(1):3–29
Donovan JW (2007) Colchicine. In: Shannon MW, Borron SW, Burns MJ (eds) Haddad and Winchester’s clinical management of poisoning and drug overdose. Saunders/Elsevier, Philadelphia
Neuss MN, McCallum RM, Brenckman WD, Silberman HR (1986) Long-term colchicine administration leading to colchicine toxicity and death. Arthritis Rheum 29(3):448–449
Goldbart A, Press J, Sofer S, Kapelushnik J (2000) Near fatal acute colchicine intoxication in a child. A case report. Eur J Pediatr 159(12):895–897
Dixon AJ, Wall GC (2001) Probable colchicine-induced neutropenia not related to intentional overdose. Ann Pharmacother 35(2):192–195
Tanios MA, El Gamal H, Epstein SK, Hassoun PM (2004) Severe respiratory muscle weakness related to long-term colchicine therapy. Respir Care 49(2):189–191
Calvet X, Ramirez Lazaro MJ, Lehours P, Megraud F (2013) Diagnosis and epidemiology of Helicobacter pylori infection. Helicobacter 18(Suppl 1):5–11
Dresser GK, Spence JD, Bailey DG (2000) Pharmacokinetic-pharmacodynamic consequences and clinical relevance of cytochrome P450 3A4 inhibition. Clin Pharmacokinet 38(1):41–57
Wandel C, Kim RB, Kajiji S, Guengerich P, Wilkinson GR, Wood AJ (1999) P-glycoprotein and cytochrome P-450 3A inhibition: dissociation of inhibitory potencies. Cancer Res 59(16):3944–3948
Dogukan A, Oymak FS, Taskapan H, Guven M, Tokgoz B, Utas C (2001) Acute fatal colchicine intoxication in a patient on continuous ambulatory peritoneal dialysis (CAPD). Possible role of clarithromycin administration. Clin Nephrol 55(2):181–182
Rollot F, Pajot O, Chauvelot-Moachon L, Nazal EM, Kelaidi C, Blanche P (2004) Acute colchicine intoxication during clarithromycin administration. Ann Pharmacother 38(12):2074–2077
Cheng VCC, Ho PL, Yuen KY (2005) Two probable cases of serious drug interaction between clarithromycin and colchicine. South Med J 98(8):811–813
McKinnell J, Tayek JA (2009) Short term treatment with clarithromycin resulting in colchicine-induced rhabdomyolysis. J Clin Rheumatol 15(6):303–305
Akdag I, Ersoy A, Kahvecioglu S, Gullulu M, Dilek K (2006) Acute colchicine intoxication during clarithromycin administration in patients with chronic renal failure. J Nephrol 19(4):515–517
Hung IF, Wu AK, Cheng VC et al (2005) Fatal interaction between clarithromycin and colchicine in patients with renal insufficiency: a retrospective study. Clin Infect Dis 41(3):291–300
Kim JB, Kim S, Lee T et al (2013) Colchicine-induced rhabdomyolysis caused by interaction with clarithromycin in a patient with Behcet disease. J Clin Rheumatol Pract Rep Rheum Musculoskelet Dis 19(2):108–109
van der Velden W, Huussen J, Ter Laak H, de Sevaux R (2008) Colchicine-induced neuromyopathy in a patient with chronic renal failure: the role of clarithromycin. Neth J Med 66(5):204–206
Altiparmak MR, Pamuk ON, Pamuk GE, Hamuryudan V, Ataman R, Serdengecti K (2002) Colchicine neuromyopathy: a report of six cases. Clin Exp Rheumatol 20(4 Suppl 26):S13–S16
Kuncl RW, Duncan G, Watson D, Alderson K, Rogawski MA, Peper M (1987) Colchicine myopathy and neuropathy. New Engl J Med 316(25):1562–1568
Wilbur K, Makowsky M (2004) Colchicine myotoxicity: case reports and literature review. Pharmacotherapy 24(12):1784–1792
Altman A, Szyper-Kravitz M, Shoenfeld Y (2007) Colchicine-induced rhabdomyolysis. Clin Rheumatol 26(12):2197–2199
Boomershine KH (2002) Colchicine-induced rhabdomyolysis. Ann Pharmacother 36(5):824–826
Chattopadhyay I, Shetty HG, Routledge PA, Jeffery J (2001) Colchicine induced rhabdomyolysis. Postgrad Med J 77(905):191–192
Debie K, Conraads V, Vrints C (2003) Colchicine-induced rhabdomyolysis in a patient with chronic heart failure. Acta Cardiol 58(6):561–562
Dawson TM, Starkebaum G (1997) Colchicine induced rhabdomyolysis. J Rheumatol 24(10):2045–2046
Sugie M, Kuriki A, Arai D, Ichikawa H, Kawamura M (2005) [A case report of acute neuromyopathy induced by concomitant use of colchicine and bezafibrate]. No to shinkei =Brain Nerve 57(9):785–790
Atmaca H, Sayarlioglu H, Kulah E, Demircan N, Akpolat T (2002) Rhabdomyolysis associated with gemfibrozil-colchicine therapy. Ann Pharmacother 36(11):1719–1721
Hsu W-C, Chen W-H, Chang M-T, Chiu H-C (2002) Colchicine-induced acute myopathy in a patient with concomitant use of simvastatin. Clin Neuropharmacol 25(5):266–268
Justiniano M, Dold S, Espinoza LR (2007) Rapid onset of muscle weakness (rhabdomyolysis) associated with the combined use of simvastatin and colchicine. J Clin Rheumatol Pract Rep Rheum Musculoskelet Dis 13(5):266–268
Alayli G, Cengiz K, Canturk F, Durmus D, Akyol Y, Menekse EB (2005) Acute myopathy in a patient with concomitant use of pravastatin and colchicine. Ann Pharmacother 39(7–8):1358–1361
Sarullo FM, Americo L, Di Franco A, Di Pasquale P (2010) Rhabdomyolysis induced by co-administration of fluvastatin and colchicine. Monaldi Arch Chest Dis = Archivio Monaldi per le malattie del torace/Fondazione clinica del lavoro, IRCCS [and] Istituto di clinica tisiologica e malattie apparato respiratorio, Universita di Napoli, Secondo ateneo. 74(3):147–149
Tufan A, Dede DS, Cavus S, Altintas ND, Iskit AB, Topeli A (2006) Rhabdomyolysis in a patient treated with colchicine and atorvastatin. Ann Pharmacother 40(7–8):1466–1469
Garrouste C, Philipponnet C, Kaysi S, Enache I, Tiple A, Heng AE (2012) Severe colchicine intoxication in a renal transplant recipient on cyclosporine. Transplant Proc 44(9):2851–2852
Eleftheriou G, Bacis G, Fiocchi R, Sebastiano R (2008) Colchicine-induced toxicity in a heart transplant patient with chronic renal failure. Clin Toxicol 46(9):827–830
Bebarta VS, King JA, McDonough M (2008) Proton pump inhibitor-induced rhabdomyolysis and hyponatremic delirium. The American journal of emergency medicine. 26(4):519e1–e2
Nozaki M, Suzuki T, Hirano M (2004) Rhabdomyolysis associated with omeprazole. J Gastroenterol 39(1):86–86
Nance JR, Mammen AL (2015) Diagnostic evaluation of rhabdomyolysis. Muscle Nerve 51(6):793–810. doi:10.1002/mus.24606
Rigante D, Lopalco G, Tarantino G, Compagnone A, Fastiggi M, Cantarini L (2015) Non-canonical manifestations of familial Mediterranean fever: a changing paradigm. Clin Rheumatol. doi:10.1007/s10067-015-2916-z
Author contributions
O.C.—Study design, author; G.L.—Study design, author; A.H.—Patient selection, case presentation; A.G.—Patient selection, case presentation; Y.L.—Study design, editorial review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare they have no conflicting interests.
Informed consent
This study was approved by the IRB 0314-14-MMC. Written informed consent was not required from the patients for publication of this case report. A copy of the IRB exemption is available for review by the editor of this journal.
Additional information
Oren Cohen and Garrett Locketz have equally contributed to this work.
Rights and permissions
About this article
Cite this article
Cohen, O., Locketz, G., Hershko, A.Y. et al. Colchicine–clarithromycin-induced rhabdomyolysis in Familial Mediterranean Fever patients under treatment for Helicobacter pylori . Rheumatol Int 35, 1937–1941 (2015). https://doi.org/10.1007/s00296-015-3325-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-015-3325-y