Abstract
The purpose of the study was to examine whether rheumatoid arthritis (RA) patients have higher prevalence of metabolic syndrome (MetS) than osteoarthritis (OA) patients in association with a higher level of chronic systemic inflammation in rheumatoid arthritis. A total of 583 RA and 344 OA outpatients were analyzed in this multicentric study. Metabolic syndrome was defined using the National Cholesterol Education Program Adult Treatment Panel III criteria. A 1.6-fold higher prevalence of MetS was found in patients with OA compared with the RA patients. Among the parameters of MetS, patients with OA had significantly higher levels of waist circumference, systolic blood pressure, fasting blood glucose and triglycerides, whereas HDL cholesterol and diastolic blood pressure values were similar in both groups of patients. Higher values of inflammatory markers [C-reactive protein (CRP), erythrocyte sedimentation rate (ESR)] in MetS than in non-MetS patients and higher prevalence of MetS in patients with CRP level ≥5 mg/L in both RA and OA patients were found. In multivariate logistic regression analysis, significant predictors of MetS were type of arthritis (OA vs. RA; OR 2.5 [95 % CI 1.82–3.43]), age (OR 1.04 [95 % CI 1.03–1.06]) and ESR (OR 1.01; [95 % CI 1.00–1.01]). The significant association between OA and MetS was maintained in the regression model that controlled for body mass index (OR 1.87 [95 % CI 1.34–2.61]). The present analysis suggests that OA is associated with an increased risk of MetS, which may be due to a common underlying pathogenic mechanism.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The risk of cardiovascular (CV) events and mortality is increased in rheumatoid arthritis (RA) and seems to be approximately 50 % higher in RA patients compared with the general population [1, 2]. The classical cardiovascular risk factors, including smoking, hypertension, dyslipidemia, insulin resistance and diabetes mellitus, obesity and physical inactivity, do not appear to explain the excess cardiovascular risk in RA [3]. A very important link between RA and cardiovascular disease is inflammation as it plays a key role in all stages of atherosclerosis. It also has an influence on and accentuates some of the traditional cardiovascular risk factors, such as dyslipidemia, obesity and insulin resistance [4]. The exact pathophysiologic mechanism by which this relation between cardiovascular disease and RA could be explained is not completely clear.
Metabolic syndrome (MetS) is a cluster of major risk factors for cardiovascular disease such as dyslipidemia, hypertension, insulin resistance, impaired glucose tolerance or diabetes, and obesity. There are multiple criteria for definitions of MetS; the most commonly used are the NCEP/ATP III and International Diabetes Federation criteria [5, 6]. A recent meta-analysis showed that MetS is associated with a twofold increase in cardiovascular outcome and a 1.5-fold increase in all-cause mortality [7]. In addition to insulin resistance, inflammation is closely associated with the pathogenesis of MetS [8].
An increased prevalence of MetS in RA patients was found in a number of studies [9–15], but not in all [16–18]. A 17–45.2 % prevalence of MetS in RA patients was found in the studies with a large number of patients that used the current definitions of MetS [5, 6].
While both have aging and adiposity as important risk factors, osteoarthritis (OA) and the MetS have only recently been associated with one another. In the vast NHANES III study, MetS was prevalent in 59 % of the OA population and 23 % of the population without OA. Each of the five cardiovascular risk factors that comprise MetS was more prevalent in the OA population [19]. Comparable prevalence of MetS in OA patients (54.9 %) was found in a study by Leite [20]. In the Japanese ROAD study, the risk of knee OA development and progression increased with the presence of each additional component of the MetS [21]. While obesity is a well-recognized risk factor for OA in weight-bearing knee joints, the association of OA with the MetS is not completely explained by an obesity-induced increased biomechanical load. Overweight and obese persons also have an increased risk of OA in hands, which are not weight-bearing, implicating systemic factors in the obesity–OA connection [22]. The pathogenesis of OA and the MetS each involves abnormalities in common metabolic intermediates including glucose, hormones, several growth factors, transcription factors, nitric oxide and reactive oxygen species [23]. Over the last several decades, both OA and the MetS have been increasingly recognized as low-grade inflammatory conditions with elevations in systemic inflammatory markers such as hsCRP (high-sensitivity C-reactive protein) [24]. For both entities, there are clear pathogenic roles for inflammatory mediators and hormones such as IL1β, TNFα and leptin [23].
Obesity and MetS frequently coexist and define obese individuals “at risk” of adverse health outcomes. Recent studies have identified a subset of obese individuals who have a low burden of adiposity-related metabolic abnormalities compared with “at-risk” obese individuals, the so-called metabolically healthy obese (MHO) phenotype. There is no universally accepted definition of MHO and the extent to which the MHO phenotype is associated with a lower risk of adverse health outcomes remains the subject of debate [25].
There are few studies comparing cardiovascular risk in RA and OA patients. Cardiovascular risk assessment revealed that RA patients exercised more frequently, but they had diabetes more often and their insulin sensitivity and HDL cholesterol concentrations were lower, as compared to OA patients [26]. In another study, prevalence and distribution of known cardiovascular comorbid conditions were similar in RA and OA [27].
The aim of this study was to determine and compare the prevalence of MetS in patients with RA and OA, and to assess the factors associated with MetS. Comparison of the two diseases, both characterized by a chronic course and painful joint involvement, but with either high (RA) or low (OA) levels of chronic systemic inflammation, might reveal the contribution of chronic inflammation on MetS prevalence in these diseases.
Patients and methods
A multicentric cross-sectional study was performed in regional rheumatology medical centers of Croatia. A total of 625 RA and 352 OA patients who attended the outpatient clinics from September 1 to December 31, 2009, were consecutively enrolled in the study. The presence of MetS was defined according to the updated third report of the NCEP-ATP III criteria by the presence of at least three out of five abnormalities: waist circumference (men > 102 cm, women > 88 cm); triglycerides ≥150 mg/dL (1.69 mmol/L) or drug treatment for elevated triglycerides; HDL cholesterol levels (men < 40 mg/dL, 1.03 mmol/L; women < 50 mg/dL, 1.29 mmol/L) or drug treatment for reduced HDL cholesterol; elevated blood pressure (≥130 mmHg systolic blood pressure or ≥85 mmHg diastolic blood pressure or drug treatment for hypertension); and elevated fasting glucose ≥100 mg/dL (5.6 mmol/L) or drug treatment for hyperglycemia [5]. We excluded 42 RA patients and 8 OA patients from the analysis, since they were missing the data necessary for the diagnosis of MetS, which yielded the total of 583 RA and 344 OA patients. The diagnoses of RA and OA (knee, hip and hand) were established by qualified rheumatologists according to the 1987 American College of Rheumatology (ACR) classification criteria for RA [28] and the ACR criteria for OA [29–31]. The study protocol was approved by the Ethical Committee of the Dubrava University Hospital, Zagreb, the coordinative center of the study, and a written informed consent was obtained from all study participants.
All participants underwent a detailed evaluation guided by a questionnaire administered in all collaborative departments. The evaluation included a detailed medical history, physical examination and measurement of body height and weight. Patients with ischemic heart disease were not included in the study. Patients >65 years of age were considered elderly. Body mass index (BMI) was calculated by dividing weight (kg) by height2 (square meters), and patients with BMIs >25 were qualified as overweight (including obesity). “Metabolically healthy obese” was defined as patients with BMI ≥30 kg/m2 and less than three MetS criteria present in OA and RA [25]. Waist and hip circumferences were measured, and the waist-to-hip ratio (WHR) was calculated [32]. Pain and the patients’ general health (GH) were assessed using the appropriate visual analog scales (VAS). Pain VAS (VASP) ranged from 0 to 10, with 10 being the most intensive pain [33]. General health VAS (VASGH) was part of the DAS28-CRP score [34]. VAS was represented by a 100-mm-long line on which the patients evaluated their own health, with 100 mm representing the best health. RA patient functional status and disease activity were assessed by the Croatian translation of the health assessment questionnaire (HAQ) [35] and by the DAS28-CRP score [34].
All antihypertensive and antirheumatic medications taken by the enrolled patients were recorded in detail (indications, dose and duration of treatment). Blood pressure (BP) was measured after a 5-min rest in a sitting position on the right arm with a mercury sphygmomanometer and a standard cuff. The recorded BP value for each patient was the mean of three subsequent measurements at 5-min intervals. Arterial hypertension (HT) was defined according to the European Society of Hypertension and the European Society of Cardiology 2007 guidelines with BP ≥140 mmHg and/or diastolic BP ≥90 mmHg [36] or any BP with antihypertensive treatment.
Venous blood samples were collected for laboratory investigations after overnight fasting. The following tests were performed in the laboratories of the collaborative hospitals: erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), total cholesterol (Chol), high-density lipoproteins (HDL), low-density lipoproteins (LDL), triglycerides (TG), creatinine and plasma glucose (Glc). When required, oral glucose tolerant tests (OGTT) were performed. Diabetes (DM) was defined by a history of DM with current use of antidiabetic medication or fasting Glc >126 mg/dL (7 mmol/L) or Glc in OGTT (2 h) >200 mg/dL (11.1 mmol/L) [37]. The same standard methods were used in all laboratories, and biochemical assays were performed using Olympus autoanalyzers according to the manufacturer’s protocol.
Statistical analysis
The distribution of data was assessed for normality using Kolmogorov–Smirnoff test. Values are presented as median [interquartile range (IQR)], mean [standard deviation (SD)] or percentage [confidence interval (CI)], as appropriate. Comparisons were performed using t test, Mann–Whitney U test and Chi-square test, for normally distributed, non-normally distributed and categorical variables, respectively. Binary logistic regression was used to assess the association of various variables with MetS in RA and OA patients, as well as in the entire group. In multivariate models, the variables that were significant at p < 0.2 level in both groups were included, and a multivariate backward-stepwise analysis was performed also with the inclusion of BMI as a continuous covariate. p values <0.05 (two tailed) were considered significant. All statistical analyses were performed using SPSS 17.0 software (SPSS Inc., Chicago, USA). The adjustment of MetS prevalence for age and BMI was made according to [38].
Results
Characteristics of RA and OA patients (Table 1)
The proportion of female patients was higher than that of men in both the RA and OA groups, in a similar ratio. In comparison with OA patients, patients with RA were younger, with a lower proportion of elderly patients, had a longer duration of the disease, a higher proportion of smokers (ever and current), a lower BMI and WHR, a lower proportion of overweight/obese patients, similar VASP and VASGH, lower proportion of dyslipidemic patients and a lower proportion of persons with diabetes and hypertension.
Laboratory investigations showed higher plasma CRP concentrations and ESR in patients with RA, whereas total Chol, LDL and plasma creatinine concentrations were similar in both groups of patients.
Among the parameters of MetS, in comparison with RA patients, patients with OA had significantly higher levels of waist circumference, systolic blood pressure, fasting blood glucose and TG, whereas HDL and diastolic blood pressure values were similar in both groups of patients. Analyzing the frequency of “metabolically healthy obese” patients in OA and RA subgroups, we observed no statistically significant difference (8.4 vs. 7.4 %; p = 0.65).
Prevalence of MetS in RA and OA patients (Tables 2, 3)
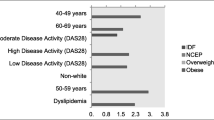
The prevalence of MetS was lower in the RA group than in the OA group and remained lower after adjusting for age and BMI. The prevalence of MetS was lower in RA group in both males and females, while the difference in prevalence of MetS by sex within the RA and OA groups was not statistically significant.
Within the BMI <25 kg/m2 group, the RA group had a lower proportion of participants with MetS and a similar result was found in the BMI ≥25 kg/m2 group. RA group also had a lower proportion of MetS patients in both <65 years and ≥65 years groups. However, in patients with BMI <25 kg/m2, there was no statistically significant difference in the prevalence of MetS within the <65 and 65 and over age strata, owing to the relatively small sample size in this group.
The lower proportion of MetS in RA group in comparison with OA group was also found in both groups regarding the dyslipidemia status (yes/no), in those with no history of anamnestic diabetes, in all strata of smoking status, and both in the participants with normal and high CRP (cutoff value of 5 mg/L). Participants with dyslipidemia in both RA and OA groups had higher frequency of MetS than those without dyslipidemia, and similar result was found for anamnestic diabetes.
The proportion of MetS patients within the RA and OA groups was not statistically significantly different across the smoking strata (current, ex, never).
The participants with CRP concentration of ≥5 mg/L had higher frequency of MetS in both the RA and OA groups.
Regarding the prevalence of MetS by the classes of drugs given in the treatment of arthritis, there was a statistically significantly higher prevalence of MetS in the OA group, regardless of NSAID or other analgesics consumption. Within the OA group, those patients who were not taking analgesic (acetaminophen) had a higher prevalence of MetS than those who did (p = 0.019), while in the RA group, there were no significant differences according to the type of treatment used.
Comparison of risk factors, patients’ characteristics and laboratory measurements between RA and OA patients (Table 4)
Within the RA group, participants with MetS were older, had a higher systolic and diastolic blood pressure and higher BMI and WHR. They also scored higher on the VAS scale, had higher CRP and ESR, higher total Chol, LDL cholesterol and TG as well as lower HDL cholesterol. Their creatinine and blood glucose values were also higher, respectively.
Within the OA group, participants with MetS were older, had a higher systolic and diastolic blood pressure, higher BMI and WHR. They had higher CRP and ESR, higher TG and blood glucose and lower HDL cholesterol.
Participants with MetS and RA in comparison with participants with MetS and OA were younger, had higher disease duration, lower BMI (with no significant difference in WHR), higher CRP and ESR, lower HDL cholesterol, higher LDL cholesterol, lower TG and lower blood glucose. There were no differences both between and within the arthritis subgroups according to the pack-years of smoking.
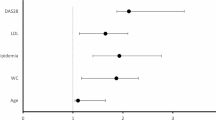
Logistic regression analysis
In univariate logistic regression models done separately for RA and OA groups, significant predictors of MetS were age, duration of disease, BMI and ESR for RA patients, and age and BMI for OA patients. The variables that were significant at p < 0.2 level in both groups were included in backward-stepwise multivariate analyses for the entire pool of participants with disease (RA/OA) added as binary variable. Another model was performed by excluding BMI in order to assess the impact of BMI on the association of arthritis type with MetS. The results are shown in Tables 5 and 6. Significant predictors of MetS were OA (in comparison with RA), higher ESR values and older age. The inclusion of BMI in the model (higher BMI being significant predictor of MetS) somewhat diminished the association of the type of arthritis with MetS; however, it remained significant.
Discussion
In this study, prevalence of MetS in RA patients is consistent with reported prevalence [9, 13, 17], whereas the prevalence of MetS in OA patients was somewhat higher than earlier reported prevalence [19, 20]. This difference can be, at least partially, attributed to disparities in the study design, the population studied and the OA criteria used.
A 1.6-fold higher prevalence of MetS was found in the patients with OA compared with the RA patients (68.6 vs. 43.1 %; p < 0.001) and remained higher after adjusting for age and BMI (68.6 vs 59.3 %, p = 0.005), with higher prevalence in both males and females. The prevalence was higher across the subgroups of age and BMI, with the exception of patients with BMI <25 kg/m2 owing to the relatively small sample size in this group. In NHANES III study, the crude prevalence of MetS was >twofold higher in the population with OA compared with control group, regardless of sex, and it was limited to the population ≤18–65 years [19].
The overall reported prevalence of MetS in Croatia in persons older than 40 years is 38.7 % [39]. When age was taken into account (we compared our data for the 40–59 and 60+ age groups with the published data) according to 95 % CI, there was no difference in the prevalence of MetS in 40–59 group of patients with RA compared with the prevalence in the general Croatian population (35.8 % [95 % CI 30.3–41.8] vs. 36.2 % [95 % CI 33.7–38.9]), while in the 60+ age group patients with RA, higher prevalence of MetS (53.7 % [95 % CI 47.9–59.4] vs. 41.6 % [95 % CI 38.7–44.5]) could be assumed. In the OA group, prevalence of MetS was higher than in general population both in 40–59 age group (58.3 % [95 % CI 48.3–67.7]) and in 60 + age group (73.4 % [95 % CI 67.5–78.5]). However, this indirect comparison of prevalence is rather insufficient, and investigations with proper control groups are needed.
Among the parameters of MetS, in comparison with RA patients, patients with OA had significantly higher levels of waist circumference, systolic blood pressure, fasting blood glucose and TG, whereas HDL cholesterol and diastolic blood pressure values were similar in both groups of patients. Therefore, four of the six individual cardiovascular risk factors values assessed were significantly higher in patients with OA in comparison with RA patients. In NHANES III study, four (hypertension, abdominal obesity, elevated TG and elevated fasting blood glucose) of the five MetS constituent risk factors were significantly more prevalent in the population with OA than in the general population without OA. Low HDL-C levels were not significantly more prevalent in the population with OA [19].
Significant predictors of MetS were age, duration of disease, BMI and ESR for RA patients, and age and BMI for OA patients. The fact that age was independently associated with the presence of MetS is not surprising because this is a variable known to increase the frequency of comorbidities, MetS among them [14, 17]. However, in NHANES III study, the population with OA at a young age had a substantially increased risk of having MetS relative to the general population without OA, but as age increased, this relative risk diminished, until age 78 years, at which point the risk of having MetS became equal in the two populations [19]. In a study by Chung et al., the prevalence of MetS was 30 % in RA patients with long-standing disease, 22 % in patients with RA patients with early arthritis and 10 % in controls, respectively [10]. Disease duration was similar in RA patients with and without MetS in some studies [9, 14, 18].
Higher values of inflammatory markers (CRP, ESR) in MetS than in non-MetS patients and higher prevalence of MetS in patients with CRP level >5 mg/L in both RA and OA patients indicate an association of chronic inflammation and MetS. However, the prevalence of MetS in RA patients is lower than in OA patients although the values of inflammatory markers are higher in the former than in the latter. Probably this is due to rather weak association of chronic inflammation and MetS, and the effect of chronic inflammation is overwhelming by other factors, as indicated by regression analyses where association between CRP and MetS was not expressed (Table 5).
Unlike some previous studies [9–11, 13], there was no association between RA disease activity and MetS assessed by the DAS28-CRP (Tables 4, 5). However, Sahebari et al. [17] found no association between DAS 28 and the presence of MetS components by either definition. The association between higher ESR and the presence of MetS in patients with RA in our study was previously reported [11, 15]. These findings further support the role of chronic inflammation in insulin resistance development [40]. However, in two recent studies, no relationship between the MetS and ESR was observed [12, 41].
Logistic regression incorporating the type of arthritis showed that of all variables analyzed, having OA (in comparison with RA) was the most influential predictive factor for having MetS (OR 2.502, 95 % CI 1.824–3.431), with age (OR 1.044, 95 % CI 1.030–1.057) and ESR (OR 1.007, 95 % CI 1.000–1.014). The significant association between OA and MetS was maintained in the regression model that controlled for BMI (Table 6), and the risk of having MetS was also significantly associated with higher ESR values and older age. In NHANES study, having OA was the most influential predictive factor for having MetS [19]. The influence of OA on the probability of having MetS was dependent on age, being more significant at younger ages, unlike in our study.
In some studies, methotrexate therapy was associated with reduced prevalence of MetS in patients with RA [11, 12, 42]. However, these findings are not consistent with other studies [13, 18]. In addition, the use of glucocorticoids did not significantly contribute to the presence of MetS in patients with RA in previous reports (10, 11, 18). Our results showed no significant association of MetS with NSAID use in RA and OA and no association of MetS with any disease-modifying drug (DMARD) or glucocorticoid use in RA.
The current view is that OA is a group of disease that can be differentiated based on the risk factors involved and mechanisms underlying the joint damage (aging, obesity, genetic factors, or injury). The association between obesity and hand osteoarthritis suggests a role for circulating mediators released by the adipose tissue known as adipokines [22]. Thus, osteoarthritis may have a systemic metabolic component. Converging evidence from epidemiological and biological studies support the concept of metabolic osteoarthritis, defined as a broad clinical phenotype that includes obesity-related osteoarthritis and OA related to hypertension, type 2 diabetes and dyslipidemia [43, 44].
The commonalities in pathogenic mechanism between MetS and OA are supported by epidemiological data. As a result of the finding that having OA at the mean age of the general population is itself associated with a 5.26-fold increased risk of MetS even when controlling for obesity, it has been suggested that the finding of OA, alone, should prompt evaluation for cardiovascular disease [19]. Also, Kornaat et al. [45] found an association between popliteal artery wall thickness and generalized OA which persisted even after correction for sex, age and BMI suggesting that OA is a part of MetS and not solely correlated with obesity.
Osteoarthritis may be associated with either MetS or each of its components [43], although published data are somewhat conflicting [44]. In the NHANES III cohort, a 1-point increase in HOMA-IR was associated with an increase in the knee OA risk of 18 % in non-obese males and 34 % in obese males after adjustment on several factors including age [46]. In the ROAD study, glucose intolerance was independently associated with the development and progression of radiographic knee OA [47]. Although independent associations between OA and type 2 diabetes were demonstrated in other populations, negative studies have been reported [48, 49]. An independent association between hypertension and OA has been reported [46]. In our study population, as previously reported, a robust association of age and BMI with HT prevalence in both RA and OA was shown. Higher HT prevalence in OA patients in comparison with RA patients was rather due to age and BMI than due to features of the disease [50].
At present, a prevailing hypothesis regarding MetS is that chronic low-grade inflammation may be responsible, at least in part, for the development of systemic abnormalities such as glucose and lipid dysregulation, hypertension and OA [43].
Several limitations are to be recognized. First, the cross-sectional design can establish association but not causality. Second, the non-inclusion of a healthy control group may weaken the conclusions of the study. Third, RA inflammation fluctuates, and CRP and DAS28-CRP as a cross-sectional markers may not capture the long-term cumulative inflammatory burden. Fourth, patients with different localizations of OA (knee, hip or hand) were studied as a group, whereas the systemic impact of MetS may depend on the localization of OA. Fifth, the extent of radiographic severity of RA or OA was not analyzed in the study. Finally, we cannot exclude the possibility of patient selection bias in both RA and OA, as most of the centers from which patients were recruited are a secondary care centers.
In conclusion, the present analysis suggests that OA is associated with increased risk of MetS. Cause-and-effect relationship cannot be determined from an analysis of cross-sectional data; our analysis does not suggest that OA leads to MetS or vice versa. However, our findings strongly suggest that common pathogenic mechanism may be active in patients with OA and patients with MetS.
References
Avina-Zubieta J, Choi H, Sadatsafavi M, Etminan M, Esdaile J, Lacaille D (2008) Risk of cardiovascular mortality in patients with rheumatoid arthritis: a meta-analysis of observational studies. Arthritis Rheum 59:1690–1697
Avina-Zubieta J, Thomas J, Sadatsafavi M, Lehman A, Lacaille D (2012) Risk of incident cardiovascular events in patients with rheumatoid arthritis: a meta-analysis of observational studies. Ann Rheum Dis 71:1524–1529
Ku IA, Imboden JB, Hsue PY, Ganz P (2009) Rheumatoid arthritis: model of systemic inflammation driving atherosclerosis. Circ J 73:977–985
Liao K, Solomon D (2013) Traditional cardiovascular risk factors, inflammation and cardiovascular risk in rheumatoid arthritis. Rheumatology (Oxford) 52:45–52
Grundy SM, Cleeman JI, Merz CN, Brewer HB Jr, Clark LT, Hunninghake DB et al (2004) Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation 110:227–239
Alberti KG, Zimmet P, Shaw J et al (2005) The metabolic syndrome: a new worldwide definition. Lancet 366:1059–1062
Mottillo S, Filion KB, Genest J et al (2010) The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol 56:1113–1132
Dandona P, Aljada A, Chaudhuri A, Mohanty P, Garg R (2005) Metabolic syndrome: a comprehensive perspective based on interactions between obesity, diabetes, and inflammation. Circulation 111:1448–1454
Da Cunha VR, Brenol CV, Brenol JC, Fuchs SC, Arlindo EM et al (2012) Metabolic syndrome prevalence is increased in rheumatoid arthritis patients and is associated with disease activity. Scand J Rheumatol 41:186–191
Chung CP, Oeser A, Solus JF, Avalos I, Gebretsadik T et al (2008) Prevalence of the metabolic syndrome is increased in rheumatoid arthritis and is associated with coronary atherosclerosis. Atherosclerosis 196:756–763
Dao HH, Do QT, Sakamoto J (2010) Increased frequency of metabolic syndrome among Vietnamese women with early rheumatoid arthritis: a cross-sectional study. Arthritis Res Ther 12:R218
Zonana-Nacach A, Santana-Sahagún E, Jiménez-Balderas FJ, Camargo-Coronel A (2008) Prevalence and factors associated with metabolic syndrome in patients with rheumatoid arthritis and systemic lupus erythematosus. J Clin Rheumatol 14:74–77
Karvounaris SA, Sidiropoulos PI, Papadakis JA, Spanakis EK, Bertsias GK et al (2007) Metabolic syndrome is common among middle-to-older aged Mediterranean patients with rheumatoid arthritis and correlates with disease activity: a retrospective, cross-sectional, controlled, study. Ann Rheum Dis 66:28–33
Salinas MJ, Bertoli AM, Lema L, Saucedo C, Rosa J, Quintana R et al (2013) Prevalence and correlates of metabolic syndrome in patients with rheumatoid arthritis in Argentina. J Clin Rheumatol. 19:439–443
Rostom S, Mengat M, Lahlou R, Hari A, Bahiri R, Hajjaj-Hassouni N (2013) Metabolic syndrome in rheumatoid arthritis: case control study. BMC Musculoskelet Disord 14:147
Karimi M, Mazloomzadeh S, Kafan S, Amirmoghadami H (2011) The frequency of metabolic syndrome in women with rheumatoid arthritis and in controls. Int J Rheum Dis 14:248–254
Sahebari M, Goshayeshi K, Mirfeizi Z et al (2011) Investigation of the association between metabolic syndrome and disease activity in rheumatoid arthritis. Sci World J 11:1195–1205
Lee SG, Kim JM, Lee SH, Kim KH, Kim JH et al (2013) Is the frequency of metabolic syndrome higher in South Korean women with rheumatoid arthritis than in healthy subjects? Korean J Intern Med 28:206–215
Puenpatom RA, Victor TW (2009) Increased prevalence of metabolic syndrome in individuals with osteoarthritis: an analysis of NHANES III data. Postgrad Med 121:9–20
Leite AA, Costa AJ, Lima Bde A, Padilha AV, Albuquerque EC, Marques CD (2011) Comorbidities in patients with osteoarthritis: frequency and impact on pain and physical function. Rev Bras Reumatol 51:118–123
Yoshimura N, Muraki S, Oka H, Kawaguchi H, Nakamura K, Akune T (2011) Association of knee osteoarthritis with the accumulation of metabolic risk factors such as overweight, hypertension, dyslipidemia, and impaired glucose tolerance in Japanese men and women: the ROAD study. J Rheumatol 38:921–930
Carman WJ, Sowers M, Hawthorne VM, Weissfeld LA (1994) Obesity as a risk factor for osteoarthritis of the hand and wrist: a prospective study. Am J Epidemiol 139:119–129
Velasquez MT, Katz JD (2010) Osteoarthritis: another component of metabolic syndrome? Metab Syndr Relat Disord 8:295–305
Sowers M, Jannausch M, Stein E, Jamadar D, Hochberg M, Lachance L (2002) C-reactive protein as a biomarker of emergent osteoarthritis. Osteoarthr Cartil 10:595–601
Roberson LL, Aneni EC, Maziak W et al (2014) Beyond BMI: the ‘metabolically & healthy obese’ phenotype & its association with clinical/subclinical cardiovascular disease and all-cause mortality—a systematic review. BMC Public Health 14:14
Dessein PH, Stanwix AE, Joffe BI (2002) Cardiovascular risk in rheumatoid arthritis versus osteoarthritis: acute phase response related decreased insulin sensitivity and high-density lipoprotein cholesterol as well as clustering of metabolic syndrome features in rheumatoid arthritis. Arthritis Res 4:R5
Erb N, Pace AV, Douglas KMJ, Banks MJ, Kitas GD (2004) Risk assessment for coronary heart disease in rheumatoid arthritis and osteoarthritis. Scand J Rheumat 33:293–299
Arnett FC, Edworthy SM, Bloch DA et al (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324
Altman R, Alarcon G, Appelrouth D, Bloch D et al (1991) The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum 34:505–514
Altman R, Alarcon G, Appelrouth D, Bloch D et al (1990) The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hand. Arthritis Rheum 33:1601–1610
Altman R, Asch E, Bloch D et al (1986) The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the knee. Arthritis Rheum 29:1039–1049
See R, Abdullah SM, McGuire DK et al (2007) The association of differing measures of overweight and obesity with prevalent atherosclerosis: the Dallas Heart Study. J Am Coll Cardiol 50:752–759
Mannion AF, Balague F, Pellise F, Cedraschi C (2007) Pain measurement in patients with low back pain. Nat Clin Pract Rheumatol 3:610–618
The DAS calculator. http://www.das-score.nl/dasculators.html. Accessed 21 March 2011
Kirwan JR, Reeback JS (1986) Stanford health assessment questionnaire modified to assess disability in British patients with rheumatoid arthritis. Br J Rheumatol 25:206–209
Mancia G, De Backer G, Dominiczak A et al (2007) Guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 28:1462–1536
World Health Organization. Department of Noncommunicable Disease Surveillance (1999) Definition and diagnostic criteria for diabetes mellitus and other categories of glucose intolerance. In: Definition, diagnosis and classification of diabetes mellitus and its complications. Report of a WHO consultation. Part 1, Diagnosis and classification of diabetes mellitus. World Health Organization, Geneva, pp 2–8
Zhang J, Yu KF (1998) What’s the relative risk? JAMA 280:1690–1691
Ivezic-Lalic D, Bergman Markovic B, Kranjcevic K, Kern J, Vrdoljak D, Vucak J (2013) Diversity of metabolic syndrome criteria in association with cardiovascular diseases—a family medicine-based investigation. Med Sci Monit 19:571–578
Shahin D, Eltoraby E, Mesbah A, Houssen M (2010) Insulin resistance in early untreated rheumatoid arthritis patients. Clin Biochem 43:661–665
Karakoc M, Batmaz I, Sariyildiz MA, Tahtasiz M, Cevik R et al (2012) The relationship of metabolic syndrome with disease activity and the functional status in patients with rheumatoid arthritis. Clin Med Res 4(4):279–285
Abourazzak FE, Mansouri S, Najdi A, Tahiri L, Nejjari C, Harzy T (2014) Prevalence of metabolic syndrome in patients with rheumatoid arthritis in Morocco: a cross-sectional study of 179 cases. Clin Rheumatol 33:1549–1555
Sellam J, Berenbaum F (2013) Is osteoarthritis a metabolic disease? Joint Bone Spine 80:568–573
Zhuo Q, Yang W, Chen J, Wang Y (2012) Metabolic syndrome meets osteoarthritis. Nat Rev Rheumatol 8:729–737
Kornaat PR, Sharma R, van der Geest RJ et al (2009) Positive association between increased popliteal artery vessel wall thickness and generalized osteoarthritis: is OA also part of the metabolic syndrome? Skeletal Radiol 38:1147
Karvonen-Gutierrez CA, Sowers MR, Heeringa SG (2012) Sex dimorphism in the association of cardiometabolic characteristics and osteophytes-defined radiographic knee osteoarthritis among obese and non-obese adults: NHANES III. Osteoarthr Cartil 20:614–621
Yoshimura N, Muraki S, Oka H et al (2012) Accumulation of metabolic risk factors such as overweight, hypertension, dyslipidaemia, and impaired glucose tolerance raises the risk of occurrence and progression of knee osteoarthritis: a 3-year follow-up of the ROAD study. Osteoarthr Cartil 20:1217–1226
Frey MI, Barrett-Conner E, Sledge PA et al (1996) The effect of noninsulin dependent diabetes on the prevalence of clinical osteoarthritis. A population based study. J Rheumatol 23:716–722
Anderson JJ, Felson DT (1988) Factors associated with osteoarthritis of the knee in the first national Health and Nutrition Examination Survey (HANES I). Evidence for an association with overweight, race, and physical demands of work. Am J Epidemiol 128:179–189
Morovic-Vergles J, Salamon L, Marasovic-Krstulovic D, Kehler T, Sakic D, Badovinac O, Vlak T et al (2013) Is the prevalence of arterial hypertension in rheumatoid arthritis and osteoarthritis associated with disease? Rheumatol Int 33:1185–1192
Acknowledgments
This work was supported by a grant from the Ministry of Science, Education and Sport, the Republic of Croatia (198-1081874-0183) to Jadranka Morović-Vergles).
Conflict of interest
The authors declare no conflicts of interest.
Ethical standard
A written informed consent was obtained from all study participants.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Šalamon, L., Morović-Vergles, J., Marasović-Krstulović, D. et al. Differences in the prevalence and characteristics of metabolic syndrome in rheumatoid arthritis and osteoarthritis: a multicentric study. Rheumatol Int 35, 2047–2057 (2015). https://doi.org/10.1007/s00296-015-3307-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-015-3307-0