Abstract
Allopurinol is effective for the control of gout and its long-term complications when taken consistently. There is evidence that adherence to allopurinol therapy varies across population groups. This may exacerbate differences in the burden of gout on population groups and needs to be accurately assessed. The aim of this study was to describe the prevalence of allopurinol use in a region of New Zealand using community pharmacy dispensing data and to examine the levels of suboptimal adherence in various population groups. Data from all community pharmacy dispensing databases in a New Zealand region were collected for a year covering 2005/2006 giving a near complete picture of dispensings to area residents. Prevalence of allopurinol use in the region by age, sex, ethnicity and socioeconomic position was calculated. Adherence was assessed using the medication possession ratio (MPR), with a MPR of 0.80 indicative of suboptimal adherence. Multiple logistic regression was used to explore variations in suboptimal adherence across population groups. A total of 953 people received allopurinol in the study year (prevalence 3 %). Prevalence was higher in males (6 %) than in females (1 %) and Māori (5 %) than non-Māori (3 %). The overall MPR during the study was 0.88, with 161 (22 %) of patients using allopurinol having suboptimal adherence. Non-Māori were 54 % less likely to have suboptimal allopurinol adherence compared to Māori (95 % CI 0.30–0.72, p = 0.001). These findings are consistent with those from other studies nationally and internationally and point to the important role for health professionals in improving patient adherence to an effective gout treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gout is one of the most common inflammatory arthritides in males [1, 2]. It occurs when monosodium urate crystals build up in the joints and soft tissues and is primarily characterised by attacks of painful inflammation around these joints [1–3]. Improperly treated, gout can lead to joint deterioration and disability [1, 4]. There is concern that the pain and reduced joint mobility associated with gout may hinder attempts by sufferers to reduce the risks arising from other diseases commonly linked with gout [4, 5]. Gout can have a profound impact on the lives of sufferers and their families, leading to reduced social engagement and increased dependence of the sufferer on their family for care and support [1, 3, 5]. It has also been associated with reduced ability to work and, consequently, increased worker absenteeism [6].
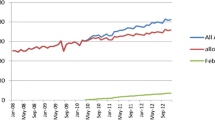
Gout is a common health problem in New Zealand, with a linkage study using national data on hospital, dispensing and laboratory test results estimating the prevalence of gout to be 3.8 % in the population aged 20 and over [7] (although Jackson et al. [8] suggest this might be an underestimate). According to this study, men were 3.6 times as likely to have gout as women. It also identified a clear socioeconomic gradient in prevalence, with people living in the most deprived areas 1.4 times as likely to have gout as people living in the least deprived areas. There were also ethnic differences, with people who identified as Māori (the indigenous people of New Zealand) and those who identified as of the Pacific ethnic group 3.1 and 3.6 times, respectively, as likely to have gout as people identifying as European/other ethnicity. These findings are consistent with other research on the social patterning of gout, both nationally and internationally [1, 2, 9–11].
Allopurinol can be effective in the long-term control of gout and prevention of disability when used consistently and in adequate dosages, and is the most commonly used medicine for this purpose [12–14]. However, international evidence suggests that sufficient levels of adherence for effective control of gout are often not reached [1, 15–18]. In their review of medication adherence in seven chronic conditions, Briesacher et al. [16] found patients with gout had the lowest adherence rates by some margin.
Pharmacy dispensing records have been used by some researchers to study adherence patterns in patients with gout and have been shown to be a valid source of information on adherence [19]. In New Zealand, the Ministry of Health maintains a database (‘Pharms’) containing records of all subsidised medicine dispensings outside of hospitals. This database can be used to examine adherence to medicines in New Zealand. Such analyses, however, will have limitations. This is because dispensings where a subsidy was not paid by the state are not recorded in Pharms, and subsidisation can depend on patient income. How this might bias medicine utilisation studies comparing population groups is not well understood [20, 21]. In contrast, all prescribed medicine dispensings outside of hospitals are recorded by the dispensing pharmacies. The ‘Equity in Prescription Medicines Use Study’ carried out previously by the authors collected data from all of the pharmacies in one region of New Zealand, effectively obtaining a census of prescription medicines use in that population [21].
The current study aimed to describe the prevalence of allopurinol use in a region of New Zealand using data obtained directly from community pharmacy dispensing databases and compare it to what is known about the prevalence of gout in particular population groups. A secondary aim was to determine the levels of suboptimal adherence in these groups. We hypothesised that both prevalence and levels of suboptimal adherence would vary across population groups, particularly between Māori and non-Māori.
Methods
Study population and dataset
The study employed a cross-sectional design using data generated by the Equity in Prescription Medicines Use Study. Further detail about that study can be found in Horsburgh et al. [21]. Briefly, data on 619,264 dispensings to 38,027 individuals were obtained from all of the community pharmacies in a New Zealand region (Gisborne) for a year covering 1 October 2005–31 September 2006, giving a near complete picture of dispensings to residents in that area for that year. The Gisborne region had a population of 44,463 people, with nearly half of the resident population identifying as Māori [22].
Pharmacy dispensing records contain information on:
-
Patient demographics (including date of birth, gender, unique health system identifier and address)
-
The medicines dispensed (including generic and brand name, dosage, amount dispensed and instructions for the patient printed on the label).
Information on the patient’s ethnicity was obtained from a central data collection (the National Health Index collection maintained by the Ministry of Health) using the health system identifier in the pharmacy dispensing record. Information on whether the patient died during the study period was also obtained from this collection. The address recorded in the pharmacy dispensing record was geocoded to assign a socioeconomic deprivation score using the NZDep2006 small area index of deprivation [23]. The NZDep2006 is a relative measure of area deprivation, which divides small areas (typically of 90–100 people) into deciles of socioeconomic deprivation. The most deprived ten percent of areas are classified as decile 10, with the least deprived ten percent classified as decile 1. The NZDep2006 decile scores were collapsed into Least (deciles 1 and 2), Middle (deciles 3–8) and Most (deciles 9 and 10) deprived for the purposes of this study. The geocoded address was also used to determine whether the patient resided in an urban or rural area, as classified using Statistic New Zealand’s urban/rural classification system [24]. Patient age was calculated as at the mid-point of the study period, which was also the date of the Census which supplied the population counts for calculating prevalence. Medicines were coded according to the main ingredient using the 2007 version of the ATC–DDD classification system [25].
All dispensing records for residents of the Gisborne area for allopurinol (ATC code M04AA01) for the year covering 1 October 2005–31 September 2006 were selected from the Equity in Prescription Medicines Use Study dataset.Footnote 1 Pharmacy dispensing records do not contain information about the patient’s diagnosis, so it was assumed that all allopurinol dispensings were for the control of hyperuricaemia related to gout. Since the primary indication for allopurinol use in New Zealand is the control of hyperuricaemia [26], this is a reasonable assumption and has been used in other studies [7]. The study population was restricted to those patients aged 25 and over.
Ethical approval for the Equity in Prescription Medicines Use Study was granted by a Ministry of Health accredited ethical review committee (Northern X Committee, approval number NTX/06/09/111). Gisborne Māori health organisations were also consulted.
Calculation of daily dosage
Calculating adherence required that whether a person was in possession of allopurinol on a given day could be identified. Medicines in New Zealand have instructions on how much and how often the patient should take the medicine printed on a label affixed to the medicine container. These instructions are also recorded in the pharmacy dispensing record in textual form, but not in a standardised numeric format, which would allow the calculation of daily allopurinol usage. The textual instructions were therefore manually converted into numeric descriptions of dosing ‘episodes’. Each episode represented a constant dosing regimen, with a new episode beginning when the dosing regimen changed. The number of tablets to be taken at each dosing, the number of dosing events per day and the number of days this regimen was to run for were coded for each episode. Table 1 shows some examples of textual dispensing instructions and how they were represented using this coding system. So, using the second example on the table, if a patient was prescribed 98 100-mg tablets of allopurinol, they would be recorded as having 50 mg of allopurinol (half a 100-mg tablet) for a 28-day period (episode 1), followed by 28 days of 100 mg of allopurinol daily (episode 2) and then 200 mg of allopurinol (two 100 mg tablets) daily until the number of tablets ran out (episode 3). This would lead to the patient being considered to be in possession of allopurinol for 84 days. In the third example, the days in possession if the patient was prescribed 28 100-mg tablets would be 56 days, since the patient was still considered to be in possession of allopurinol on the days when they were directed to skip a dose.
Patients may have collected a new dispensing for their allopurinol before their previously dispensed supply had run out. If this occurred, the new dispensing was assumed to have started when the previous supply would have run out.
Outcome measures
The primary outcome measure was the prevalence of any allopurinol dispensing during the study year. The medication possession ratio (MPR) was used to assess the secondary outcome measure of suboptimal adherence [27]. The MPR is simply the ratio of days supplied from initial dispensing to the number of days to the end of the study period or the patient’s date of death. A MPR < 0.80 was the threshold for indicating suboptimal adherence to allopurinol, as used in other research on allopurinol adherence [15, 17, 18]. The MPR analysis was restricted to patients who received their first dispensing of allopurinol within the first 6 months of the study period and who received more than 90 days of worth of allopurinol, 90 days being the maximum number of days which can be supplied in a single dispensing in New Zealand. This was to ensure that there was at least 6 months of follow-up for each patient in the analysis and to reduce the impact on the MPR of patients who only took allopurinol briefly (e.g. discontinued at commencement of therapy because of an inability to tolerate the medicine). If patients who initiated allopurinol therapy in the second 6 months of the study period were included, it would be difficult to differentiate patients who discontinued treatment shortly after initiation from patients who were simply being non-adherent. Also, patients dispensed medicines within 90 days of the end of the study period might never appear to be non-adherent if they were dispensed a full 90 days of worth of allopurinol, leading to an overestimation of the MPR through a form of immortal time bias [28]. The algorithm used adjusted for situations where the patient did not take allopurinol every day. In these cases, the patient was considered to possess allopurinol in the days between doses.
Data analysis
Logistic regression was used to determine whether the odds of suboptimal allopurinol adherence varied by age, ethnicity, socioeconomic deprivation level and gender. Regression models were fitted separately to generate crude odds ratios and 95 % confidence intervals. A multivariable logistic regression model containing all of the demographic variables together was fitted to generate adjusted odds ratios and 95 % confidence intervals. The statistical package R was used for data management and analysis [29]. Significance testing and confidence intervals were not used when describing the study sample, since the study included the entire population of the region.
Results
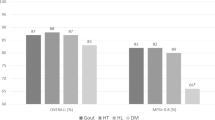
A total of 953 patients aged 25 or over in the study region received one or more dispensings (7,447 total) of allopurinol during the study period, a prevalence of 3 %. Table 2 shows the prevalence of allopurinol use in the study region by age, gender, ethnicity, socioeconomic deprivation and residential location. Prevalence was much higher in males (6 %) than in females (1 %), reflecting the underlying gender difference in gout prevalence. Allopurinol use prevalence was also higher in Māori (5 %) than in non-Māori (3 %), and also increased with age. Prevalence did not vary substantially by socioeconomic deprivation or residential location.
Of the 953 patients receiving allopurinol, eleven (1 %) were removed from the adherence analyses because a dispensing instruction could not be coded (e.g. ‘as directed’). One hundred and twenty-eight (13 %) of these patients were excluded because they did not receive a dispensing in the first six months, while a further 82 (9 %) were excluded because they received 90 or fewer days’ supply. This left a total of 732 (77 %) patients who received a dispensing in the first six months of the study period for a supply longer than 90 days. The overall MPR was 0.88, with 161 (22 %) patients dispensed allopurinol having suboptimal adherence. The percentage of each demographic group with a suboptimal MPR is shown in Table 3.
Table 4 presents the results from the fitted logistic regression models. The crude odds ratios indicated a trend towards lower odds of suboptimal adherence in the older age groups and in non-Māori. A multivariable logistic regression model was also fitted to identify associations between demographic variables and suboptimal adherence while adjusting for potential confounding by other demographic variables. The pattern of odds ratios remained similar after adjustment, with a trend towards lower odds of suboptimal adherence with increasing age and lower odds in the non-Māori population. No statistically significant difference in adherence was found between males and females, between the different tiers of socioeconomic deprivation, or between patients residing in rural or urban locations, although the odds ratio for this latter group did move substantially towards 1.00 after adjustment. The difference between Māori and non-Māori was still marked after adjustment, with non-Māori 54 % less likely to have suboptimal allopurinol adherence compared to Māori (95 % CI 0.30–0.72, p = 0.001).
Discussion
The findings on allopurinol use prevalence are broadly consistent with other studies with regard to the social patterning of gout. It is not surprising that allopurinol use was less than estimated gout prevalence, as people with undiagnosed or untreated gout will not be identifiable through dispensing records. On the basis of the patterns of allopurinol use prevalence presented here, however, it would be difficult to conclude that one group is being treated with allopurinol less than their estimated gout prevalence would suggest they should be relative to other groups.
The patterns of adherence tell a different story, however. Non-Māori were far less likely to have suboptimal adherence than Māori. So while Māori patients may receive allopurinol treatment, many of them were not taking it consistently enough for it to provide effective serum uric acid control. This is consistent with other research, which has found Māori and Pacific gout patients to have higher uric acid levels than non-Māori, non-Pacific patients despite receiving similar dosages of allopurinol [30].
The cost of treatment may have been one of the drivers of non-adherence in Māori gout patients. Other authors have found cost to be one of the reasons cited by gout patients for non-adherence to allopurinol therapy [31, 32]. There is some evidence that the cost of allopurinol therapy may be higher for Māori and Pacific gout patients than non-Māori, non-Pacific patients. Dalbeth et al. [30] found that the mean self-reported personal financial cost of gout treatment per month was around three times higher for Māori and Pacific gout patients (NZ$12.50 versus NZ$3.90), although the authors did not speculate as to why this was so. This is despite Māori and Pacific people having lower median incomes than other groups [33]. Other research has highlighted that Māori and Pacific people are more likely to defer obtaining a prescription because of cost, even after adjusting for a range of demographic, socioeconomic and health-related variables [34, 35]. The markedly lower levels of adherence in Māori, as measured by the possession of allopurinol dispensings, may be due in part to deferment of obtaining or redeeming allopurinol prescriptions because of financial pressures.
Poor health literacy is another theme which has emerged from both local and international literature and which may explain why some population groups have lower adherence than others. Qualitative research from the USA and the UK has highlighted a lack of awareness by patients about the duration of therapy, with some believing that they no longer need to take allopurinol if they have not experienced an attack for a while. The exacerbation of symptoms when initiating allopurinol during an attack was also cited as a barrier to good adherence. Patients often reported feeling insufficiently informed about gout and allopurinol treatment, as well as uncomfortable with seeking clarification from their health provider [31, 32]. These findings have been echoed in similar research in New Zealand, with some patients unclear what role allopurinol played in their treatment (prevention versus pain relief) and the nature and control of gout in general, and many patients reporting being unhappy both with the level of information provided to them by health professionals and uncomfortable seeking clarification [3, 5]. Family and community were often the main sources of information on gout, leading to the propagation of long-standing myths about gout and its treatment. Perceived knowledge about gout has been found to be positively associated with adherence to urate-lowering therapy [36], suggesting a significant, pro-active role for health professionals in engaging with patients and communities on gout and its treatment.
It was anticipated that residing in a rural area might be related to poorer adherence. Other research in the study area has highlighted geographical issues, such as the distance required to travel to collect medicines and poor road conditions, as barriers to the timely collection of medicines [37]. However, this study did not find a relationship between residential location and suboptimal adherence. This may be to a lack of power in the study, with the confidence intervals for residential location and socioeconomic deprivation being quite wide. It may also be that adherence is worse in patients living in highly rural areas but that this effect is masked by the dichotomising of residential location into the coarse categories of rural and urban. Unfortunately, the number of patients residing in highly rural areas was too small to allow finer-grained analyses.
The use of community pharmacy dispensing databases is a strength of this study. Unlike the most viable alternative data source, Pharms, community pharmacy databases record all dispensings regardless of subsidisation. They therefore provide the most accurate picture of prescription medicine access and possession in the community. In particular, the ability to code the dispensing instructions allows greater precision in calculating adherence than possible using Pharms. Analyses based solely on Pharms data, in contrast, may underestimate prescription medicine use and possession, and may do so differentially across population groups. While patients may still not take their medicines despite having collected them, dispensing data from pharmacy records provides the most feasible and accurate means of measuring adherence at a population level.
A limitation with community pharmacy dispensing databases, and many other routinely collected prescription data sources, is the lack of a diagnosis indicator. For this study, it was assumed that allopurinol was being prescribed for gout. This may not have been the case, as allopurinol may also be used in conjunction with other treatments for certain cancers and kidney stones. These uses are likely to be rare and likely to account for very few of the allopurinol users included in this study.
Adherence may have been overestimated in this study due to the conservative exclusion criteria adopted. By excluding 82 patients because they received less than three months of supply of allopurinol, patients who commenced allopurinol and experienced an exacerbation of symptoms were likely to be removed from the adherence analyses. If these patients were included in the analyses, the overall MPR would have been 0.83, with 29 % of patients having an MPR < 0.80. However, the pattern of odds ratios obtained in the logistic regression would not have changed, with Māori still having substantially lower odds of being adherent (see Supplementary Tables 5 and 6 for the full adherence results with the 82 patients included). It is likely that the 82 patients will have been a mixture of patients not adhering to allopurinol treatment and patients stopping treatment on their clinician’s advice due to side effects or intolerance of allopurinol.
The findings from this study fit with those from other studies both locally and internationally and highlight the importance of further research into the causes of non-adherence in allopurinol users, particularly Māori. Indigenous people in other countries, such as Australia and Taiwan, have seen explosive increases in gout prevalence in the previous century. It is important that research is undertaken to identify whether these groups are also suffering greater burden through insufficient control of their condition. The findings from this study also highlight the crucial role for health professionals, both with individual patients and the wider community, in improving allopurinol adherence.
Notes
There were no medicines in ATC category M04AA51 (allopurinol, combinations) dispensed. No other urate-lowering medicine was available in New Zealand during the study period.
References
Brook RA, Forsythe A, Smeeding JE, Lawrence Edwards N (2010) Chronic gout: epidemiology, disease progression, treatment and disease burden. Curr Med Res Opin 26:2813–2821. doi:10.1185/03007995.2010.533647
Smith EUR, Díaz-Torné C, Perez-Ruiz F, March LM (2010) Epidemiology of gout: an update. Best Pract Res Clin Rheumatol 24:811–827. doi:10.1016/j.berh.2010.10.004
Lindsay K, Gow P, Vanderpyl J et al (2011) The experience and impact of living with gout: a study of men with chronic gout using a qualitative grounded theory approach. J Clin Rheumatol 17:1–6. doi:10.1097/RHU.0b013e318204a8f9
Winnard D, Kake T, Gow P et al (2008) Debunking the myths to provide 21st Century management of gout. N Z Med J 121:79–85
Martini N, Bryant L, Te Karu L et al (2012) Living with gout in New Zealand: an exploratory study into people’s knowledge about the disease and its treatment. J Clin Rheumatol 18:125–129. doi:10.1097/RHU.0b013e31824e1f6f
Kleinman NL, Brook RA, Patel PA et al (2007) The impact of gout on work absence and productivity. Value Heal 10:231–237. doi:10.1111/j.1524-4733.2007.00173.x
Winnard D, Wright C, Taylor WJ et al (2012) National prevalence of gout derived from administrative health data in Aotearoa New Zealand. Rheumatology 51:901–909. doi:10.1093/rheumatology/ker361
Jackson G, Wright C, Thornley S et al (2012) Potential unmet need for gout diagnosis and treatment: capture-recapture analysis of a national administrative dataset. Rheumatology 51:1820–1824. doi:10.1093/rheumatology/kes147
Trifirò G, Morabito P, Cavagna L et al (2012) Epidemiology of gout and hyperuricaemia in Italy during the years 2005–2009: a nationwide population-based study. Ann Rheum Dis. doi:10.1136/annrheumdis-2011-201254
Mikuls TR, Saag KG (2006) New insights into gout epidemiology. Curr Opin Rheumatol 18:199–203. doi:10.1097/01.bor.0000209435.89720.7c
Robinson PC, Taylor WJ, Merriman TR (2012) A systematic review of the prevalence of gout and hyperuricemia in Australia. Intern Med J 42:997–1007. doi:10.1111/j.1445-5994.2012.02794.x
Rothenbacher D, Primatesta P, Ferreira A et al (2011) Frequency and risk factors of gout flares in a large population-based cohort of incident gout. Rheumatology 50:973–981. doi:10.1093/rheumatology/keq363
Dalbeth N, So A (2010) Hyperuricaemia and gout: state of the art and future perspectives. Ann Rheum Dis 69:1738–1743. doi:10.1136/ard.2010.136218
Schlesinger N, Dalbeth N, Perez-Ruiz F (2009) Gout–what are the treatment options? Expert Opin Pharmacother 10:1319–1328. doi:10.1517/14656560902950742
Reach G (2011) Treatment adherence in patients with gout. Joint, Bone, Spine 78:456–459. doi:10.1016/j.jbspin.2011.05.010
Briesacher BA, Andrade SE, Fouayzi H, Chan KA (2008) Comparison of drug adherence rates among patients with seven different medical conditions. Pharmacotherapy 28:437–443. doi:10.1592/phco.28.4.437
Solomon DH, Avorn J, Levin R, Brookhart MA (2008) Uric acid lowering therapy: prescribing patterns in a large cohort of older adults. Ann Rheum Dis 67:609–613. doi:10.1136/ard.2007.076182
Harrold LR, Andrade SE, Briesacher BA et al (2009) Adherence with urate-lowering therapies for the treatment of gout. Arthritis Res Ther 11:R46. doi:10.1186/ar2659
Dunbar J, Dunning EJ, Dwyer K (1989) Compliance measurement with arthritis regimen. Arthritis Care Res (Hoboken) 2:A8–A16. doi:10.1002/anr.1790020309
Horsburgh S, Malik M, Norris P et al (2009) Prescribing and dispensing data sources in New Zealand: their usage and future directions. School of Pharmacy, Dunedin
Horsburgh S, Norris P, Becket G et al (2010) The equity in prescription medicines use study: using community pharmacy databases to study medicines utilisation. J Biomed Inform 43:982–987. doi:10.1016/j.jbi.2010.08.004
Statistics New Zealand (2009) QuickStats about Gisborne District. Statistics New Zealand, Wellington
Salmond C, Crampton P, Atkinson J (2007) NZDep2006 index of deprivation. Department of Public Health, University of Otago, Wellington
Statistics New Zealand (2013) Urban/rural profile (experimental) classification categories. http://www.stats.govt.nz/methods/classifications-and-standards/urban-rural-profile-experimental-class-categories.aspx. Accessed 13 Feb 2013
WHO Collaborating Centre for Drug Statistics Methodology (2007) Guidelines for ATC classification and DDD assignment. WHO Collaborating Centre for Drug Statistics Methodology, Oslo
Apotex NZ Ltd (2011) New Zealand data sheet: Apo-Allopurinol. Apotex NZ Ltd, Auckland
Andrade SE, Kahler KH, Frech F, Chan KA (2006) Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf 15:565–574; discussion 575–577. doi: 10.1002/pds.1230
Rothman KJ, Greenland S, Lash TL (2008) Modern epidemiology, 3rd edn. Lippincott Williams & Wilkins, Philadelphia
R Core Team (2012) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Dalbeth N, House ME, Horne A et al (2012) The experience and impact of gout in Māori and Pacific people: a prospective observational study. Clin Rheumatol. doi:10.1007/s10067-012-2110-5
Harrold LR, Mazor KM, Velten S et al (2010) Patients and providers view gout differently: a qualitative study. Chronic Illn 6:263–271. doi:10.1177/1742395310378761
Spencer K, Carr A, Doherty M (2012) Patient and provider barriers to effective management of gout in general practice: a qualitative study. Ann Rheum Dis 71:1490–1495. doi:10.1136/annrheumdis-2011-200801
Ministry of Social Development (2010) The social report. Ministry of Social Development, Wellington
Jatrana S, Crampton P, Norris P (2011) Ethnic differences in access to prescription medication because of cost in New Zealand. J Epidemiol Community Health 65:454–460. doi:10.1136/jech.2009.099101
Jatrana S, Crampton P (2009) Primary health care in New Zealand: who has access? Health Policy (New York) 93:1–10. doi:10.1016/j.healthpol.2009.05.006
Dalbeth N, Petrie KJ, House M et al (2011) Illness perceptions in patients with gout and the relationship with progression of musculoskeletal disability. Arthritis Care Res (Hoboken) 63:1605–1612. doi:10.1002/acr.20570
Davis A (2012) Geographical access to medicines in Te Tairawhiti. University of Otago
Acknowledgments
This work is based on a study funded by the Health Research Council of New Zealand (Grant Number 07/139). The authors would like to thank the pharmacists and people of Gisborne for their advice and the use of their data, as well as the support of Ngati Porou Hauora and Turanga Health. The authors would also like to acknowledge the Local Advisory Committee to the project for their extremely useful insights and comments.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Horsburgh, S., Norris, P., Becket, G. et al. Allopurinol use in a New Zealand population: prevalence and adherence. Rheumatol Int 34, 963–970 (2014). https://doi.org/10.1007/s00296-013-2935-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-013-2935-5