Abstract
To evaluate a rheumatology outpatient consultation access system for new patients. New patients seen from April 2005 to April 2006 at our rheumatology clinic (n = 4,460) were included and classified according to their appointment type: ordinary appointments (OA) to be seen within 30 days, urgent appointments (UA) and work disability appointments (WDA) to be seen within 3 days. Age, sex, diagnosis, and health-related quality of life (HRQoL) as determined by the Rosser Index were recorded. Logistic regression models were run to identify factors that contribute to each type of appointment. OA was the method of access for 1,938 new patients, while 1,194 and 1,328 patients were seen through WDA and UA appointments, respectively. Younger male patients, and those with microcrystalline arthritis, sciatica, shoulder, back, or neck pain, were more likely to use the faster access systems (UA or WDA), whereas patients with a degenerative disease were mainly seen through OA (<0.001). Subjects with poor (3.96; 95 % CI, 2.8–5.5) or very poor HRQoL (70.8; 95 % CI, 14.9–334) were strongly associated to visiting a rheumatologist through the WDA or UA access systems, respectively, compared to OA. Age, gender, diagnosis, and mainly health-related quality of life are associated with the referral pattern of access to rheumatologic outpatient care. Among new patients subjects with the worst HRQoL were more likely to access with faster methods (UA or WDA) than those with better HRQoL.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent years, several advances have been achieved/made in rheumatology, especially in the development of new drugs and treatment strategies that have sparked a rapid improvement in patients’ care [1–5]. However, despite the higher quality of care, barriers that hinder or delay access to rheumatologic care still exist [6–8]. These include patient- and physician- (i.e. sociodemographics, beliefs, and poor awareness) [9–12] as well as health care delivery- and policy-related factors (i.e. scheduling systems, long waiting lists, insufficient number of rheumatologists, and health insurance) [13–16]. Thus, there is a growing acceptance that patient referral to rheumatologic care needs to be redesigned and improved in order to achieve the timely access that is appropriate to the patients’ real needs.
The rheumatology service at the Hospital Clinico de San Carlos provides rheumatologic care to more than 600,000 inhabitants of Madrid (Spain) as part of a universal health system. However, it is not free from access barriers. In daily practice, the main access barrier is the existence of long waiting lists. Access to our service at the San Carlos Rheumatology outpatient clinic is achieved through one of the three pre-established referral patterns: urgent appointments, which are obtained by patients in the emergency room at our hospital; and ordinary and urgent appointments that are obtained from their primary care physicians. The latter offers a specialized care program to subjects who have been granted work disability status due to musculoskeletal diseases. In this last case, patients are contacted by phone and upon agreement we provide an urgent appointment (work disability appointment). Due to long waiting lists, we give priority to subjects accessing our service through an urgent or work disability appointment. They are to be seen within 72 h, whereas those referred with ordinary appointments wait from 1 to up to 3 months.
The primary objective of this study is to evaluate the management of rheumatology outpatient consultation access for patients who use these services for the first time. We will examine how the new patient’s demographic characteristics, diagnoses, and health-related quality of life (HRQoL) scores affect the different types of access to rheumatology consultations. We hypothesized that new patients with the worst HRQoL have a faster access, despite long waiting lists.
Patients and methods
Setting and practice description
A total of 5.5 million inhabitants of Madrid (98 % of its population) receive universal health coverage. Madrid is organized into 11 health districts, which provide care at two levels: primary and specialized. The primary level of care is provided by primary care physicians, while the second is provided at hospitals and specialized centers.
This study was performed in health district number 7 of Madrid, which provides health care to approximately 600,000 inhabitants. It has 17 primary care centers, 2 specialized centers, and a hospital (Hospital Clinico San Carlos). Our rheumatology service provides care to all inhabitants of health district 7 in the specialized centers and hospital. It has 11 staff rheumatologists, 3 residents, and 3 advanced-practice nurse specialists. Our daily activities include clinical outpatient and inpatient care, education, and research. Demand has dramatically grown in the recent years, which has exceeded our capacity and generated long waiting lists.
New patient access process
New patients come to our rheumatologic outpatient consultations through/via three pre-established referral patterns listed below. (1) Patients who are referred by general practitioners and specialists other than the physicians at the hospital’s emergency room receive OA and are included on a waiting list for an average of 1–3 months. One exception is made for patients whose physicians prefer an urgent rheumatologic evaluation. In such cases, a phone call is placed to our service, and an urgent appointment is given. These patients wait a maximum of 3 days. (2) Patients referred by physicians at the hospital’s emergency room always receive an urgent appointment (UA) and are seen within 3 days. Physicians in the emergency room follow a defined protocol to refer patients with musculoskeletal diseases and fever, weight loss, persistent inflammatory pain, arthritis, and/or rheumatic diseases that cause great disability and/or distress. Individuals with life threatening conditions and/or those needing inpatient care are hospitalized at our service, while the remaining patients are sent back to their primary care physicians. (3) Since 1998, we have provided an early and specialized care program to subjects in our health district with work disability related to musculoskeletal diseases. It improves short- and long-term work disability outcomes and is also cost effective in almost all diagnoses except for knee pain [3, 17]. Every subject with sick leave due to a musculoskeletal disease receives a phone call from our service inviting him/her for an early rheumatologic evaluation. Those who accept obtain a work disability appointment (WDA) and are seen within 3 days.
Study design, patient sample, and data acquisition
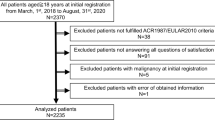
A cross-sectional study was carried out. All new patients over 15 years of age who came to our rheumatology outpatient service at the hospital or the two specialized centers from April 1, 2005 to April 1, 2006 were selected. Afterward, we included in the study those patients that could be grouped in any of these categories according to their work status and age: (a) working subjects aged 64 or less, who may receive any of the three types of appointment; (b) housewives aged 64 or less, who can get OA or UA, but not a WDA; (c) retired patients aged 65 or more, who can be given an OA or UA, but not a WDA.
During their first visit, the patients’ sociodemographic and clinical data were registered in an electronic medical record by their rheumatologist (Medi<LOG>) from which this information was exported for the present study.
Variables
The type of appointment (OA, WDA, and UA) was the dependent variable.
The independent variables were as follows: (1) sex; (2) age, which was classified into eight age groups (15–24, 25–34, 35–44, 45–54, 55–64, 65–74, 75–84, and ≥85 years); and (3) HRQoL as measured by the Rosser Index [18]. This index is a generic measure of HRQoL, which places individuals on a continuum of wellness from death to full asymptomatic function. Its score range is 0–1, where 1 indicates perfect health and 0 indicates death. It encompasses eight levels of disability and four categories of distress. The levels of disability are as follows: 1 = no disability; 2 = mild social disability; 3 = high social disability, ability to do all housework and hobbies except for the heaviest ones, mild limitations at their current job or in their studies; 4 = able to walk outside alone and go shopping, but only able to do the lightest housework and hobbies, and limited in their ability to study and to find other jobs, with lots of limitations at their current job; 5 = not able to walk outside alone or extreme difficulty walking outside, but able to walk at home without help, not able to have a salaried job, study, go shopping, or do most housework or hobbies; 6 = confined to a chair/wheelchair, but able to walk at home with help; 7 = confined to bed; or 8 = in a coma. The four categories of distress are as follows: A = no distress, B = mild distress, C = moderate distress, D = high distress. For the purpose of the present study, we have generated six groups of HRQoL according to the level of disability and distress: group 1 (excellent HRQoL): disability 1 or 2 with distress A; group 2 (good HRQoL): disability 1 or 2 with distress B; group 3 (intermediate HRQoL): disability 3, 4, or 5 with distress B; group 4 (poor HRQoL): disability 3, 4, or 5 with distress C; and group 5 (very poor HRQoL): disability 6 with distress C or D or disability 4 or 5 with distress D; and group 6: unclassified. Patients’ diagnoses using the International Classification of Diseases, 10th edition (ICD-10), were grouped into the following 16 diagnostic categories: rheumatoid arthritis (RA), spondyloarthropathies (SPA), other connective tissue diseases (OCTD), microcrystalline arthritis, knee osteoarthritis, hip osteoarthritis, other osteoarthritis, shoulder tendonitis, other tendonitis, bursitis, neck pain, back pain, sciatica, fibromyalgia, joint pain, and osteoporosis.
Statistical analysis
A statistical analysis was carried out separately for each of the three subpopulations. A description of each subpopulation was obtained using Student’s t test or chi-square test depending on the type of the variables. Lastly, multiple logistic regression equations were fitted for sociodemographic, diagnostic, and health-related variables associated with the methods of access. To test the effect of diagnostic categories on each method of access, we ran models for each of the diagnostic categories plus the variables remaining in the best explanatory models from previous global analyses. Odds ratios with 95 % confidence intervals were estimated for each of the factors that were included in the models. All analyses were run using SPSS 13.0.
Results
We treated 5,289 new patients during the study period, but in order to guarantee homogeneous study population groups, 829 (15 %) were excluded from this study resulting in only 4,460 patients being included in the analysis; 1,938 patients (43.5 %) accessed care with OA, 1,194 (26.5 %) with WDA, and 1,328 (30 %) with UA. Almost 100 % of the patients seen with UA were referred by emergency room physicians from our hospital.
Most of the patients were women (70 %) in their fifties (mean 55 ± 16 years). The most frequent diagnoses were back pain (19.8 %), tendonitis (19.8 %), and osteoarthritis (18.1 %), followed by the group of inflammatory diseases with a prevalence of 9.9 % (2.3 % for RA, 2.3 % for SPA, and 5.3 % for ODTC), joint pain (9 %), and neck pain (8.6 %). The less frequent diagnoses were sciatica (5.3 %), microcrystalline arthritis (4.7 %), osteoporosis (2.9 %), and fibromyalgia (1.9 %). In relation to the health-related quality of life variables, 13 % of the patients reported excellent HRQol, 30 % reported good HRQol, 29 % reported intermediate HRQol, while 23 % of the patients reported poor or very poor HRQol.
As shown in Table 1, our study included 2,660 working subjects under 65 years of age, who were mostly referred through faster appointments (45 % with WDA and 20 % with UA). These patients were middle aged (mean of 44.7 ± 11 years), and 63 % of them were women. The most frequent diagnosis was back pain (24.5 %), followed by tendonitis (20.5 %), joint pain (12 %), and neck pain (12 %); 42 % reported excellent or good HRQol, whereas 19 % reported poor or very poor HRQoL. This factor was strongly associated with the method of access: subjects with excellent HRQoL were more likely to access using an OA, whereas those reporting regular or poor HRQoL received WDA, and those with very poor HRQoL accessed care through UA. In relation to diagnoses, back and neck pain were mostly observed in patients that were referred with WDA, whereas osteoarthritis and joint pain were mostly observed in subjects seen through OA appointments.
Among the 424 housewives under 65 years old (mean 56 ± 7.5 years), 64.2 % came with OA and 35.8 % had UA. Of them, 22 % had poor or very poor HRQol. The most frequent diagnoses in this group were osteoarthritis (25 %), tendonitis (23 %), and back pain (14 %). No age differences were found associated to the method of access (p = 0.263), and housewives with very poor HRQoL were more likely to access care through UA than those with best HRQoL, who used OA (p < 0.001). Regarding diagnoses and method of access shoulder pain was mostly observed in urgent appointments.
Among the 1,376 new patients that were retired and over 65 years old (30.8 % of the study subjects), 55.7 % came with OA and 44.3 % with UA. Most of them were women (75 %), the mean age was 74.7 ± 5.9 years, and 29 % of the patients reported poor or very poor HRQol). Osteoarthritis (34 %) was the most prevalent diagnosis in this subpopulation (49 % of them due to knee osteoarthritis). Women were more likely than men to have an OA (p < 0.001), but no differences were found across the age groups (p = 0.342). Subjects with the best HRQoL had a tendency to access care through OA, while those with the worst HRQoL accessed care through UA (p < 0.001). Sciatica, microcrystalline arthritis, and shoulder pain were seen more in patients seen with UA than in OA. On the other hand, knee osteoarthritis was similarly distributed between the two methods of access.
Table 2 shows the estimates of the odds ratios of access using UA or WDA compared to access through OA among working subjects under 65 years of age. Men and patients in the 15–24 year age group were more likely than women and older subjects, respectively, to consult through UA or WDA. The most significant and reliable variable associated with the method of access was HRQoL. Subjects with the worst HRQoL were more likely to be seen at our service with an UA or WDA rather than with an OA. In relation to diagnoses, subjects suffering from microcrystalline arthritis and sciatica had a higher tendency to be seen through faster access appointments (UA or WDA). Shoulder tendonitis and bursitis were strongly associated with UA, and neck pain and back pain were more associated with WDA (p < 0.001) when compared to OA.
Among housewives under 65 years of age (Table 3), access was not associated with age. Women with fibromyalgia or other osteoarthritis were less likely to access through UA than through OA, whereas those diagnosed with shoulder tendonitis were more likely to use an UA. As in the previous group, HRQoL was clearly associated with the method of access, since those with the worst HRQoL had the highest probability of being referred through the emergency room.
Finally, among retired subjects older than 65 years (Table 4), men from 65 to 74 years were more likely to come with an UA than those under 75. Moreover, those diagnosed with microcrystalline arthritis, tendonitis, and sciatica were also more likely to gain access to outpatient care through UA. As in other groups, patients with the worst HRQoL were more likely to access to rheumatologic care using an UA.
Discussion
In the present study, we found that age, sex, diagnosis, and more importantly health-related quality of life are associated with the referral pattern of access to rheumatologic outpatient care. Importantly, among new patients subjects with the worst HRQoL were more likely to access with faster methods (UA or WDA) than those with better HRQoL. Therefore, despite the existence of waiting lists, we give priority to the subgroup of patients who will probably receive more benefit from early access. In addition, the profile of new patients resembled patient populations in other rheumatologic outpatient settings [19, 20], which increases the generalizability of these results.
Patient HRQoL was the single factor most strongly associated with access type among the study population groups. We have used the Rosser Index [18] to assess the HRQoL and systematically recorded it during every patient’s visit. This is a generic measure of HRQoL which examines the physical, psychological, and social dimensions of health that is easy and does not take a long time to register, making it a useful tool for routine analysis in daily practice.
HRQoL is a concept that is increasingly used as a measure of clinical outcome in research as well as in the daily care of chronic diseases. As a matter of fact, the general goal of “curing” people affected with chronic conditions has been displaced by the more realistic aim of maximizing their quality of life. Moreover, patient-centered care should certainly take into account the patient’s perception of their own health. Moreover, in rheumatology, HRQoL has been shown to be an effective predictor of health outcome, including prognosis, mortality, costs, and resources utilization across different diseases [21–24]. Our data support the use of HRQoL (along with other well-defined factors, such as diagnosis) as a useful and relevant component for redesigning and planning rheumatologic care access.
In this context, it is unquestionable that a delay in access to rheumatologic outpatient care for patients with potentially progressive rheumatic diseases, such as rheumatoid arthritis, lupus, or ankylosing spondylitis, would result in a worse outcome [25–27]. Unfortunately, our results did not show a clear association between systemic inflammatory diseases and faster referral patterns. Care should be exerted when interpreting this last result, since we used diagnoses that were made during the first visit and which could have changed after further examination and other diagnostic tests. However, a prompt access for these patients should always be guaranteed. In addition to these patients, subjects with short-term painful and disabling rheumatic diseases, such as regional pain syndromes, would also benefit from early specific therapies or procedures provided by a rheumatology service [17, 28]. In general, these patients were seen at our rheumatology outpatient care facility earlier. In fact, we found that shoulder tendonitis, microcrystalline arthritis, neck pain, back pain and sciatica were associated with faster access (UA or WDA) in the different groups of patients. These clinical problems are usually acute and painful, reflecting that sudden disability is less tolerated than other more progressive diseases such as osteoarthritis, osteoporosis, or fibromyalgia. However, in the long term, the latter diseases may have a higher disabling potential.
Although we have not demonstrated that patients with the worst HRQoL who had early access to our service received greater benefit from rheumatology care, we are confident that this assertion is correct. Nevertheless, further longitudinal studies are necessary to confirm this hypothesis and to establish which subgroups would benefit the most from earlier access.
Along with HRQoL and diagnoses, other demographic variables were examined for possible associations with the method of access to rheumatologic care. Gender was an independent and important source of disparities. Men were more likely to be referred to our service using earlier access methods (UA or WDA) than women. Moreover, housewives mostly accessed with OA (in consequence, they waited according to the waiting list at the moment). Similar results have been published elsewhere [29]. Although multiple factors may contribute to gender differences, this could reflect underlying complex social and cultural behaviors connected to healthcare utilization by men and women. Women, probably due to work and family responsibilities, prefer to seek specialized care from primary care physicians (implying a brief visit), instead of going to a hospital and waiting for hours in the emergency room.
Interestingly, the youngest subjects were more likely to use faster access (UA or WDA) on their first visit. In this case, individual factors could result in this behavior. Younger people might not tolerate the disability and/or distress generated by rheumatic diseases, and therefore, they may consider a prompt resolution of the problem to be necessary. Another possible explanation is the delay of a referral by primary care physicians, as has been reported in other specialties [30], which forces younger subjects to utilize other methods of access. The delay in referral in all types of patients may be due to the fact that most rheumatic-related problems are not life threatening. This would be worse in the case of older patients, since rheumatology diseases are considered to be a natural part of the aging process. In addition, the potential difficulties involved in seeking specialized care (transport and waiting at the hospital) may restrict the provision of appropriate access to rheumatology care to the elderly.
Nowadays, there are a wide variety of resources that can drastically improve the lives of subjects suffering from rheumatic diseases. Unfortunately, the current state of rheumatology specialty care in many countries still places barriers to access these resources. Thus, redesigning access to this care in a manner that is centered on patients and that guarantees that patients get the right care at the right time is a main concern among rheumatologists. As we reported, HRQoL is a main factor that is associated with access to rheumatologic care and would be an indication that our access system gives priority to subjects who would probably obtain more benefit. Therefore, there are compelling reasons to include HRQoL in the organization of referral and scheduling systems. Therefore, HRQoL remains a main source of interest for further research. In point, it is important to examine whether subjects with the worst HRQoL that have early access to rheumatologic care draw greater benefit. Moreover, increased emphasis on rheumatic diseases should be encouraged in medical education and society to increase the efficiency of rheumatology referrals.
References
Nixon R, Bansback N, Brennan A (2007) The efficacy of inhibiting tumour necrosis factor {alpha} and interleukin 1 in patients with rheumatoid arthritis: a meta-analysis and adjusted indirect comparisons. Rheumatology (Oxford) 2007
Jois RN, Masding A, Somerville M, Gaffney K, Scott DG (2007) Rituximab therapy in patients with resistant rheumatoid arthritis: real-life experience. Rheumatology (Oxford) 46:980–982
Abasolo L, Blanco M, Bachiller J, Candelas G, Collado P, Lajas C et al (2005) A health system program to reduce work disability related to musculoskeletal disorders. Ann Intern Med 143:404–414
Landewe RB, Boers M, Verhoeven AC, Westhovens R, van de Laar MA, Markusse HM et al (2002) COBRA combination therapy in patients with early rheumatoid arthritis: long-term structural benefits of a brief intervention. Arthritis Rheum 46:347–356
Goekoop-Ruiterman YP, de Vries-Bouwstra JK, Allaart CF, van Zeben D, Kerstens PJ, Hazes JM et al (2007) Comparison of treatment strategies in early rheumatoid arthritis: a randomized trial. Ann Intern Med 146:406–415
Finckh A, Liang MH, van Herckenrode CM, de Pablo P (2006) Long-term impact of early treatment on radiographic progression in rheumatoid arthritis: a meta-analysis. Arthritis Rheum 55:864–872
Korpela M, Laasonen L, Hannonen P, Kautiainen H, Leirisalo-Repo M, Hakala M et al (2004) Retardation of joint damage in patients with early rheumatoid arthritis by initial aggressive treatment with disease-modifying antirheumatic drugs: five-year experience from the FIN-RACo study. Arthritis Rheum 50:2072–2081
Criswell LA, Such CL, Yelin EH (1997) Differences in the use of second-line agents and prednisone for treatment of rheumatoid arthritis by rheumatologists and non-rheumatologists. J Rheumatol 24:2283–2290
Katz JN, Barrett J, Liang MH, Kaplan H, Roberts WN, Baron JA (1998) Utilization of rheumatology physician services by the elderly. Am J Med 105:312–318
Machold KP, Koller MD, Pflugbeil S, Zimmermann C, Wagner E, Stuby U et al. (2007) The public neglect of rheumatic diseases: insights from analyses of attendees in a musculoskeletal disease awareness activity. Ann Rheum Dis 66(5):697–699
Lewis CL, Wickstrom GC, Kolar MM, Keyserling TC, Bognar BA, Dupre CT et al (2000) Patient preferences for care by general internists and specialists in the ambulatory setting. J Gen Intern Med 15:75–83
Gamez-Nava JI, Gonzalez-Lopez L, Davis P, Suarez-Almazor ME (1998) Referral and diagnosis of common rheumatic diseases by primary care physicians. Br J Rheumatol 37:1215–1219
Newman ED, Harrington TM, Olenginski TP, Perruquet JL, McKinley K (2004) “The rheumatologist can see you now”: successful implementation of an advanced access model in a rheumatology practice. Arthritis Rheum 51:253–257
Harrington JT, Walsh MB (2001) Pre-appointment management of new patient referrals in rheumatology: a key strategy for improving health care delivery. Arthritis Rheum 45:295–300
Pincus T, Gibofsky A, Weinblatt ME (2002) Urgent care and tight control of rheumatoid arthritis as in diabetes and hypertension: better treatments but a shortage of rheumatologists. Arthritis Rheum 46:851–854
Yazdany J, Gillis JZ, Trupin L, Katz P, Panopalis P, Criswell LA et al (2007) Association of socioeconomic and demographic factors with utilization of rheumatology subspecialty care in systemic lupus erythematosus. Arthritis Rheum 57:593–600
Abasolo L, Carmona L, Hernandez-Garcia C, Lajas C, Loza E, Blanco M et al (2007) Musculoskeletal work disability for clinicians: time course and effectiveness of a specialized intervention program by diagnosis. Arthritis Rheum 57:335–342
Rosser R, Kind P (1978) A scale of valuations of states of illness: is there a social consensus? Int J Epidemiol 7:347–358
Cimmino MA, Ugolini D, Cauli A, Mannoni A, Macchioni P, Ciocci A et al (2006) Frequency of musculoskeletal conditions among patients referred to Italian tertiary rheumatological centers. Clin Exp Rheumatol 24:670–676
Vanhoof J, Declerck K, Geusens P (2002) Prevalence of rheumatic diseases in a rheumatological outpatient practice. Ann Rheum Dis 61:453–455
Coste J, Lefrancois G, Guillemin F, Pouchot J (2004) Prognosis and quality of life in patients with acute low back pain: insights from a comprehensive inception cohort study. Arthritis Rheum 51:168–176
Singh JA, Nelson DB, Fink HA, Nichol KL (2005) Health-related quality of life predicts future health care utilization and mortality in veterans with self-reported physician-diagnosed arthritis: the veterans arthritis quality of life study. Semin Arthritis Rheum 34:755–765
Michaud K, Messer J, Choi HK, Wolfe F (2003) Direct medical costs and their predictors in patients with rheumatoid arthritis: a three-year study of 7,527 patients. Arthritis Rheum 48:2750–2762
Ethgen O, Kahler KH, Kong SX, Reginster JY, Wolfe F (2002) The effect of health related quality of life on reported use of health care resources in patients with osteoarthritis and rheumatoid arthritis: a longitudinal analysis. J Rheumatol 29:1147–1155
Morales-Romero J, Gonzalez-Lopez L, Celis A, Rodriguez-Arreola BE, Cabrera-Pivaral CE, Gamez-Nava JI (2006) Factors associated with permanent work disability in Mexican patients with rheumatoid arthritis. A case-control study. J Rheumatol 33:1247–1249
Faurschou M, Starklint H, Halberg P, Jacobsen S (2006) Prognostic factors in lupus nephritis: diagnostic and therapeutic delay increases the risk of terminal renal failure. J Rheumatol 33:1563–1569
Sieper J, Rudwaleit M (2005) Early referral recommendations for ankylosing spondylitis (including pre-radiographic and radiographic forms) in primary care. Ann Rheum Dis 64:659–663
Marshall S, Tardif G, Ashworth N (2002) Local corticosteroid injection for carpal tunnel syndrome. Cochrane Database Syst Rev CD001554
Suominen-Taipale AL, Martelin T, Koskinen S, Holmen J, Johnsen R (2006) Gender differences in health care use among the elderly population in areas of Norway and Finland. A cross-sectional analysis based on the HUNT study and the FINRISK Senior Survey. BMC Health Serv Res 6:110
Steel J, Ellis P (2002) Do demographic variables affect the timing of referral to the nephrologist? EDTNA ERCA J 28:185–187
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leon, L., Jover, J.A., Loza, E. et al. Health-related quality of life as a main determinant of access to rheumatologic care. Rheumatol Int 33, 1797–1804 (2013). https://doi.org/10.1007/s00296-012-2599-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-012-2599-6