Abstract
Osteoarthritis (OA) is a degenerative joint disorder resulting in destruction of articular cartilage, osteophyte formation, and subchondral bone sclerosis. In recent years, numerous genetic factors have been identified and implicated in causing osteoarthritis. One such genetic defect is a single nucleotide polymorphism at position -1612 of matrix metalloproteinase-3 (MMP-3) promoter region, known to lead to three possible genotypes, 5A/5A, 6A/6A, and 5A/6A. The purpose of this study was to investigate the association of MMP-3 -1612 5A/6A gene polymorphism with knee osteoarthritis in Thai population. Genotype distributions and allelic frequencies of MMP-3 -1612 5A/6A polymorphism were investigated in 200 participants (100 patients with knee osteoarthritis and 100 healthy controls). Genotyping was performed using polymerase chain reaction-restriction fragment length polymorphism. There was no statistically significant difference between the groups with respect to genotype distribution (P > 0.05). The 5A allele frequency was indicated as 15.5 %, and 6A allele was as 84.5 % in OA patients, whereas it was 10–90 % in the control group. Accordingly, the present study has indicated that the -1612 5A/6A polymorphism genotypes of MMP-3 gene promoter do not play a role in the development of osteoarthritis in the Thai population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is a degenerative joint disorder resulting in substantial morbidity and disability in the elderly [1]. The genetic etiology of OA is not entirely known. Previously, OA was recognized as a noninflammatory arthropathy. However, recent studies have shown that an inflammatory process plays a part in the pathogenesis of OA [2, 3]. Pro-inflammatory cytokines are implicated as potential mediators in the disease [4]. A number of gene polymorphisms involved in development of knee osteoarthritis have been identified, such as those localized in or adjacent to the encoding sequences for the vitamin D receptor [5], estrogen receptor alpha [6], calcitonin [7], interleukin-6 [8], SMAD3 [9], and matrix metalloproteinase-1 [10].
Matrix metalloproteinases (MMPs), a 28-membered family of zinc-dependent endopeptidases, play essential roles in the processes of tissue remodeling and repair in physiological and pathological conditions [11, 12]. The MMP family is categorized into four main subtypes, consisting of collagenases, gelatinases, stromelysins, and membrane-type matrix metalloproteinases (MT-MMPs) [13]. Increasing evidence has accumulated for their roles in pathogenicity and progression of fibrosis.
MMP-3 is one of the stromelysin expressed in several cell types including human articular chondrocytes and synoviocytes [14]. In addition, MMP-3 is involved in the shedding of protein ectodomains from the cell surface [15] and can degrade a broad spectrum of extracellular matrix substrates, including type III, IV, and V collagens and noncollagenous extracellular matrix components, such as laminins, fibronectin, osteopontin, and proteoglycans [16]. Therefore, MMP-3 can proteolytically activate other MMPs, and pathological conditions may ensue through the overexpression of MMP genes [17]. A common adenosine insertion/deletion polymorphism (5A/6A) at position -1612 upstream of the transcription start site (rs3025039) has been examined within the MMP-3 promoter [18]. The MMP-3 gene possesses a functional promoter polymorphism at position -1612, affecting gene transcription (low-activity 6A allele, high-activity 5A allele) and resulting in low (6A/6A) and high (5A/5A, 5A/6A) promoter activity genotypes [19].
To our knowledge, data on the role of MMP-3 -1612 5A/6A polymorphism in Thai patients with knee OA have as yet not been documented in the literature. In this case–control study, we hypothesized that the -1612 5A/6A single nucleotide polymorphism of the MMP-3 gene promoter would contribute to the susceptibility of knee osteoarthritis. The purpose of this study was to investigate the association between MMP-3 -1612 5A/6A polymorphism and primary knee osteoarthritis in Thai population.
Patients and methods
Study population
This case–control study was approved by the Institutional Review Board on Human Research of the Faculty of Medicine, Chulalongkorn University. The present study was conducted in compliance with the guidelines of the Declaration of Helsinki. All subjects gave written informed consent prior to their participation in the study.
A total of 100 patients aged 51–78 years diagnosed with primary knee osteoarthritis (84 women and 16 men; mean age 65.7 ± 1.1 years) and 100 control individuals who had no symptoms or signs of OA, other arthritis, or any joint diseases (88 women and 12 men; mean age 63.5 ± 2.1 years) were recruited in this study. The diagnosis of knee OA was based on the criteria of the American College of Rheumatology, which included primary OA with any symptoms and radiographic signs of OA according to the Kellgren–Lawrence grading system [20]. Clinical characteristics on disease severity were observed by mean of Kellgren–Lawrence grade and Lequesne’s functional index reflecting functional or symptomatic status of patients [21]. Radiographic findings of OA were categorized into Kellgren–Lawrence grade 1, 2, 3, or 4. Functional or symptomatic statuses of patients were classified into mild (Lequesne’s functional index I ≤ 10) or severe (Lequesne’s functional index I ≥ 10). Control subjects were consecutively selected among people without personal and family history of OA. Participants were excluded on the basis of having arthropathy due to gout, pseudogout, rheumatoid arthritis (RA), systemic lupus erythematosus, psoriasis, hemochromatosis, previous knee injury, or previous joint infection. The patients with any systemic inflammatory or autoimmune disorders, or any type of malignant or chronic illness were not included in this study.
Genotyping of MMP-3 gene
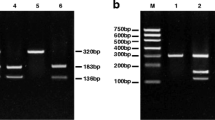
Peripheral venous blood samples of 3 ml were drawn from each individual by standard venipuncture. Genomic DNA was isolated from buffy coats by using the commercially available Qiagen Blood Cell and Culture Midi kit. Polymerase chain reaction (PCR) amplifications were performed for the -1612 5A/6A single nucleotide polymorphism (SNP) using the published primer set: 5′-GATTACAGACAT GGGTCACG-3′ (sense primer) and 5′-TTTCAATCAGGACAAGACGAAGTTT-3′ (antisense primer). The conditions of the PCR were as previously described with some modifications [22]. Briefly, PCR was performed in a 20-μl volume containing 5 μl of genomic DNA template, 2 μl of 10× Taq buffer, 2.5 mmol MgCl2, 2 mmol dNTPs, 200 nmol of forward and reverse primer, and 4 U Taq DNA polymerase (Fermentas Inc., USA). The PCR protocol was 95 °C denaturation followed by 35 cycles: denaturation at 95 °C for 45 s, annealing at 53 °C for 45 s and elongation at 72 °C for 30 s, ending with an additional elongation step of 5 min at 72 °C. The amplified sequence was digested by XmnI restriction enzyme (New England BioLabs, Beverly, Massachusetts, USA) at 37 °C overnight. After digestion, the reaction mixtures were separated by 12 % polyacrylamide gel electrophoresis and visualized by ethidium bromide staining. An example of an electrophoretic gel showing PCR product digestion with XmnI is shown in Fig. 1. The 5A/5A genotype corresponded to the presence of 97 bp fragments. The 6A/6A genotype corresponded to a 120-bp fragment. The 5A/6A genotype corresponded to the presence of 97 and 120 bp fragments.
Genotypes of MMP-3 polymorphism on 12 % polyacrylamide gel electrophoresis with ethidium bromide staining and ultraviolet light transillumination. Lane 1 and 4: 97 bp represent genotype 5A/5A. Lane 2 and 5: 120 bp represent genotype 6A/6A. Lane 3 and 6: 97 and 120 bp represent genotype 5A/6A. Lane M represents DNA standard marker (100 bp)
Statistical analysis
Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS) software, version 16.0 for Windows. The demographic and clinical data were compared between groups by the chi-square test and Student’s t test. Genotype and allelic frequencies were compared by the chi-square test. Allele and genotype proportions were evaluated for Hardy–Weinberg equilibrium. P < 0.05 was considered as indicating statistical significance.
Results
Characteristics of the population studied and the number of individuals in each group are illustrated in Table 1. There were no significant differences between groups in terms of age, gender, and mean body mass index (BMI). In the knee OA patients, the mean age was 65.7 ± 1.1 years. In the healthy controls, the mean age was 63.5 ± 2.1 years (P = 0.4). The female/male ratio was 84/16 in the patients with knee OA and 88/12 in controls (P = 0.2). Furthermore, average BMI value was not significantly different between groups, 25.7 ± 3.3 kg/m2 in the knee OA patients and 25.2 ± 3.8 kg/m2 in the controls, respectively (P = 0.3).
Table 2 presents the genotype and allelic frequencies of MMP-3 -1612 5A/6A polymorphism. 6A/6A was the most frequent genotype in OA patients, and control groups and genotype frequency fell within Hardy–Weinberg equilibrium. There was no statistically significant difference between the groups with respect to genotype distribution (P = 0.19). The 5A allele frequency was indicated as 15.5 %, and 6A allele was as 84.5 % in OA patients, whereas it was 10–90 % in the control group. According to the MMP-3 -1612 5A/6A polymorphism genotypes, there was no association between the genotypes of MMP-3 gene 5A/6A polymorphism and the clinical characteristics of the OA patients and controls.
Discussion
Osteoarthritis (OA) is one of the most common causes of joint disease and limitation of physical activity with advancing age. The knee is the most clinically significant affected joint with OA characterized by progressive destruction of articular cartilage, which leads to pain and loss of joint function. Although the multifactorial nature of OA is well recognized, genetic factors have been shown to be strong determinants of this disorder. Previous studies have shown that there are a number of candidate genes associated with the knee OA [5–10].
The matrix metalloproteinase family constitutes more than 20 enzymes that are related with degradation of the extracellular matrix [11]. The expression of MMPs has been demonstrated to be affected by the SNP occurring in MMP gene promoters [23]. MMP-3 is a crucial enzyme that directly degrades extracellular matrix and indirectly affects degradation of extracellular matrix by activating other latent MMPs [24]. Serum and synovial MMP-3 expression have been previously reported in patients with OA or with post-traumatic knee injury [25, 26].
An understanding of the factors influencing the production of MMP-3 may allow better identification of patients at risk of developing destructive disease. According to the reports, a common -1612 5A/6A gene polymorphism of MMP-3 promoter has been identified in a wide variety of diseases, including rheumatoid arthritis [27]. Whether the MMP-3 genetic polymorphism at the -1612 region influences the susceptibility or severity in patients with knee osteoarthritis is not fully determined. To address this issue, we analyzed the influence of MMP-3 -1612 5A/6A polymorphism on the risk of knee OA in the Thai population. In this case–control study, our findings demonstrated that the percentage of the MMP-3 -1612 5A/6A polymorphism allele and the distribution of genotypes were not significantly different between the OA patients and controls.
In contrast with our findings, Abd-Allah et al. [28] have shown that there were significant associations between MMP-3 -1171 5A/6A polymorphism and susceptibility with OA in the Egyptian population. Additionally, MMP-3 5A/6A promoter polymorphism was found to be associated with disease outcome in RA [27, 29]. The explanation for these conflicting results remains unclear, but may be attributed to differences in disease advancement, populations, or assays applied.
It should be pointed out, however, that there are several limitations in our study. First, this pilot study was administered as a single-center trial with a relatively small number of subjects. Additional investigation conducted on a random sample of multiple centers with larger sample sizes is essential to validate the present findings. Nonetheless, a large scale prospective study should be launched to confirm the associative effect of this polymorphism with osteoarthritis patients. Secondly, we examined only one polymorphism in most of the genes, which could have missed an association that was to a specific polymorphism. Haplotype analysis is needed to elucidate the functional variation responsible for MMP-3 expression and may provide further knowledge on the pathways responsible for the association of MMP-3 gene with OA. Another weakness is the lack of data regarding the level and source of MMP-3. More research is needed for future in vitro and in vivo studies of representative cells and tissues to gain insight into MMP-3 production and expression.
In summary, we provide evidence that the -1612 5A/6A polymorphism of the MMP-3 gene promoter is not associated with the susceptibility to knee OA in Thai population. Further studies in different populations and/or in large cohorts of OA patients are warranted to elucidate the definite association between MMP-3 -1612 5A/6A polymorphism and osteoarthritis.
References
Krasnokutsky S, Attur M, Palmer G et al (2008) Current concepts in the pathogenesis of osteoarthritis. Osteoarthritis Cartilage 16S:1–3
Banks SE (2010) Erosive osteoarthritis: a current review of a clinical challenge. Clin Rheumatol 29:697–706
Loeser RF (2009) Aging and osteoarthritis: the role of chondrocyte senescence and aging changes in the cartilage matrix. Osteoarthritis Cartilage 17:971–979
Steinmeyer J (2004) Cytokines in osteoarthritis-current status on the pharmacological intervention. Front Biosci 9:575–580
Keen RW, Hart DJ, Lanchbury JS, Spector TD (1997) Association of early osteoarthritis of the knee with a Taq I polymorphism of the vitamin D receptor gene. Arthritis Rheum 40:1444–1449
Bergink AP, van Meurs JB, Loughlin J et al (2003) Estrogen receptor alpha gene haplotype is associated with radiographic osteoarthritis of the knee in elderly men and women. Arthritis Rheum 48:1913–1922
Magaña JJ, Gálvez-Rosas A, González-Huerta C et al (2010) Association of the calcitonin gene (CA) polymorphism with osteoarthritis of the knee in a Mexican mestizo population. Knee 17:157–160
Valdes AM, Arden NK, Tamm A et al (2010) A meta-analysis of interleukin-6 promoter polymorphisms on risk of hip and knee osteoarthritis. Osteoarthritis Cartilage 18:699–704
Valdes AM, Spector TD, Tamm A et al (2010) Genetic variation in the SMAD3 gene is associated with hip and knee osteoarthritis. Arthritis Rheum 62:2347–2352
Barlas IO, Sezgin M, Erdal ME et al (2009) Association of (-1,607) 1G/2G polymorphism of matrix metalloproteinase-1 gene with knee osteoarthritis in the Turkish population (knee osteoarthritis and MMPs gene polymorphisms). Rheumatol Int 29:383–388
Murphy G, Docherty AJ (1992) The matrix metalloproteinases and their inhibitors. Am J Respir Cell Mol Biol 7:120–125
Parsons SL, Watson SA, Brown PD, Collins HM, Steele RJ (1997) Matrix metalloproteinases. Br J Surg 84:160–166
Egeblad M, Werb Z (2002) New functions for the matrix metalloproteinases in cancer progression. Nat Rev Cancer 2:161–174
Inoue K, Masuko-Hongo K, Okamoto M, Nishioka K (2005) Induction of vascular endothelial growth factor and matrix metalloproteinase-3 (stromelysin) by interleukin-1 in human articular chondrocytes and synoviocytes. Rheumatol Int 26:93–98
Arthur MJ (2000) Fibrogenesis II metalloproteinases and their inhibitors in liver fibrosis. Am J Physiol Gastrointest Liver Physiol 279:G245–G249
Woessner JF Jr (1991) Matrix metalloproteinases and their inhibitors in connective tissue remodeling. FASEB J 5:2145–2154
Nagase H, Suzuki K, Morodomi T, Enghild JJ, Salvesen G (1992) Activation mechanisms of the precursors of matrix metalloproteinases 1, 2 and 3. Matrix Suppl 1:237–244
Ye S, Watts GF, Mandalia S, Humphries SE, Henney AM (1995) Preliminary report: genetic variation in the human stromelysin promoter is associated with progression of coronary atherosclerosis. Br Heart J 73:209–215
Ye S, Eriksson P, Hamsten A, Kurkinen M, Humphries SE, Henney AM (1996) Progression of coronary atherosclerosis is associated with a common genetic variant of the human stromelysin-1 promoter which results in reduced gene expression. J Biol Chem 271:13055–13060
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Lequesne MG, Mery C, Samson M, Gerard P (1987) Indexes of severity for osteoarthritis of the hip and knee. Validation-value in comparison with other assessment tests. Scand J Rheumatol Suppl 65:85–89
Dunleavey L, Beyzade S, Ye S (2000) Rapid genotype analysis of the stromelysin gene 5A/6A polymorphism. Atherosclerosis 151:587–589
Zhu C, Odeberg J, Hamsten A, Eriksson P (2006) Allele-specific MMP-3 transcription under in vivo conditions. Biochem Biophys Res Commun 348:1150–1156
Matrisian LM (1990) Metalloproteinases and their inhibitors in matrix remodeling. Trends Genet 6:121–125
Wassilew GI, Lehnigk U, Duda GN, Taylor WR, Matziolis G, Dynybil C (2010) The expression of proinflammatory cytokines and matrix metalloproteinases in the synovial membranes of patients with osteoarthritis compared with traumatic knee disorders. Arthroscopy 26:1096–1104
Bobacz K, Maier R, Fialka C et al (2003) Is pro-matrix metalloproteinase-3 a marker for posttraumatic cartilage degradation? Osteoarthritis Cartilage 11:665–672
Ye S, Patodi N, Walker-Bone K, Reading I, Cooper C, Dennison E (2007) Variation in the matrix metalloproteinase-3, -7, -12 and -13 genes is associated with functional status in rheumatoid arthritis. Int J Immunogenet 34:81–85
Abd-Allah SH, Shalaby SM, Pasha HF, El-Shal AS, Abou El-Saoud AM (2011) Variation of matrix metalloproteinase 1 and 3 haplotypes and their serum levels in patients with rheumatoid arthritis and osteoarthritis. Genet Test Mol Biomarkers. doi:10.1089/gtmb.2011.0003
Mattey DL, Nixon NB, Dawes PT, Ollier WE, Hajeer AH (2004) Association of matrix metalloproteinase 3 promoter genotype with disease outcome in rheumatoid arthritis. Genes Immun 5:147–149
Acknowledgments
This work has been supported by Ratchadapiseksompotch Fund (RA55/22), Faculty of Medicine, Chulalongkorn University. The authors are grateful to Dr. Padet Siriyasathien, Dr. Kanok Preativatanyou, Ms. Piyanuch Bumrungpanichthaworn, Ms. Wanvisa Udomsinprasert, Research facility of Department of Biochemistry and ChulaMRC for kindly providing technical assistance.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Honsawek, S., Malila, S., Yuktanandana, P. et al. Association of MMP-3 (-1612 5A/6A) polymorphism with knee osteoarthritis in Thai population. Rheumatol Int 33, 435–439 (2013). https://doi.org/10.1007/s00296-012-2371-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-012-2371-y