Abstract
It is well known that the serum procalcitonin (PCT) levels increase in severe bacterial infections. However, there is little information about the levels of PCT in diverse diseases except mainly the infectious diseases. The aim of this study was to investigate the progress of serum levels of PCT together with traditional acute phase reactants in children with familial Mediterranean fever (FMF) during the attack and attack-free periods and to test whether PCT could help to diagnose the attack in FMF patients. The study group comprised 21 FMF patients (mean age 10 ± 4.6 years) and 19 healthy controls (mean age 10.6 ± 4.2 years). Serum levels of PCT and traditional acute phase reactants were measured during the attack and attack-free periods. Blood samples were obtained within the first 6–24 h of the attack period, 7 days later, and at least 2 months after the attack. Traditional acute phase reactants (hs-CRP, ESR, and fibrinogen) during the attack period were significantly higher than the attack-free levels and controls. PCT levels of the FMF patients during the attack period were also significantly higher than the attack-free and control group levels (median values, 0.044 ng/ml vs. 0.028 ng/ml and 0.031 ng/ml, P = 0.04, respectively). Although this difference was statistically significant (P = 0.04), median PCT values of the attack, attack-free period, and healthy subjects were lower than 0.05 ng/ml. As a result, these findings suggested that PCT levels were not conspicuously affected from inflammation and could not be used as a descriptive marker for attack in FMF patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Familial Mediterranean fever (FMF) is an autosomal recessive and autoinflammatory disease characterized by recurrent inflammatory febrile attacks of serosal and synovial membranes [1]. Inflammation typically involves the peritoneum, pleura, joints, and skin. The typical clinical course of FMF is that of exacerbations and remissions, and the increased acute phase response seen during these attacks that usually returns to normal in attack-free periods [2]. Current pathogenic hypothesis of FMF is based on the mutations in the MEFV gene, encoding the pyrin protein thought to be associated with the inflammation cascade. Mutant pyrin leads to the prevention of apoptosis and persistence of leukocytes which produce increased amounts of cytokines. In addition, during an attack, typical laboratory findings include leukocytosis, elevated erythrocyte sedimentation rate and increased acute phase reactants (e.g. C-reactive protein, fibrinogen, serum amyloid A). To date, levels of many blood cytokines and acute phase reactants other than traditional tests have been measured in FMF patients and the results have provided additional enticing clues for more understanding of its inflammation [3–5].
Procalcitonin (PCT), a 116-amino-acid prohormone of calcitonin, is used a new parameter for the severe bacterial infections and its systemic inflammation. The origin of PCT in the inflammatory response is not yet fully understood, but it is believed that PCT is produced in the liver and peripheral mononuclear cells, modulated by cytokines [6–8]. Serum PCT concentrations are negligible in a healthy population, but rapidly increase after bacterial infections [9]. Recently, the levels of PCT are used for the diagnosis of sepsis and/or evaluation of the response to treatment. Generally, if the level of PCT is the less than 0.5 ng/ml, the test is considered as negative. Although PCT elevation is significant in serious bacterial infections, its levels do not increase or only slightly increase in neoplasms, autoimmune and allergic diseases [10–12]. In other several disorders such as major surgery, heat and burn injury, trauma, shock due to cardiogenic problems, and severe systemic inflammation, PCT can be induced independently of sepsis and infection [13]. Little information is known about the levels of PCT in other diseases except mainly the infectious diseases.
Although PCT levels have been evaluated in patients with FMF in a few studies, none of them showed the progress of the PCT levels during the attack and attack-free periods of FMF patients.
The aim of this study was to investigate the progress of serum PCT levels together with traditional acute phase reactants in patients with FMF during the attack and attack-free periods and also to find whether PCT could help to diagnose the attack in FMF patients.
Materials and methods
A total of 21 consecutive FMF patients who were diagnosed according to the Tel-Hashomer criteria in Pediatric Nephrology division of Ankara University School of Medicine were included to the study. Patients were enrolled during the attack period and followed up closely at least 2 months. FMF patients with documented infections such as respiratory tract and urinary tract infections, sepsis, other systemic diseases, and amyloidosis were excluded. Blood samples were obtained within the first 6–24 h of the attack period, 7 days later, and at least 2 months after the attack. Control group that were matched according to age and sex consisted of completely healthy children without any infection or any other systemic diseases.
The ethical committee of our institution approved the study protocol, and all parents of the patients and control group gave written informed consent.
White blood cell counts (WBC), thrombocyte counts, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), fibrinogen, and PCT were measured in the patients (at three different periods as described above) and control group.
A Beckman Coulter Hematology Analyzer was used for WBC and thrombocyte counts. The ESR was evaluated by the westergren method and <20 mm/h was considered to be normal. The measurement of high-sensitive CRP (hs-CRP) was performed by the nephelometric method (Dade, Behring, Germany) and <0.8 mg/dl was accepted as normal.
Serum PCT level was determined by an immunofluorescent assay (B.R.A.H.M.S PCT Sensitive Kryptor, B.R.A.H.M.S AG, Henningsdorf, Germany). The samples were stored at −70°C, and assays were performed at the end of the study. Values of PCT levels >0.5 ng/ml were considered as abnormal [14].
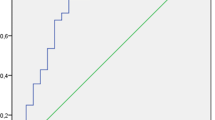
The parameters which were obtained from the patients at three different periods were compared with each other and with the control group. Statistical analysis was performed with SPSS for Windows 11.0. Results were given as median value with range. Differences between the patients and controls were compared by Mann–Whitney U test. A level of P < 0.05 was considered to be statistically significant.
Results
The study group comprised 21 FMF patients (10 males, 11 females; mean age 10 ± 4.6 years) and 19 healthy controls (8 males, 11 females; mean age 10.6 ± 4.2 years). There were no significant differences between the patients and the control group in terms of age and sex distribution. Four of the patients were newly diagnosed. The remaining patients were diagnosed previously (mean follow-up period: 47.7 ± 35.5 months) and were already taking colchicine (0.5–2 mg/day). The most common symptoms seen during the attacks were: abdominal pain (52%), arthritis or arthralgia (52%), chest pain (24%), and fever (24%). When genotypes of the patients were evaluated, M694 V was the most frequent mutation. Ten of the patients had homozygous M694 V, one had homozygous M680I, 5 had compound heterozygous (2 patients had M694 V/V726A, 1 patient had M680I/M694 V, 1 patient had M680I/E148Q, and 1 patient had M694 V/E148Q), and 5 had heterozygous M694 V mutations.
Attack hs-CRP, ESR, and fibrinogen of the FMF patients were significantly higher than the healthy control group. Attack PCT of the FMF patients was also higher than the controls (Table 1).
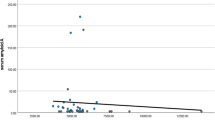
Attack hs-CRP, ESR, fibrinogen levels, WBC, and PCT levels of the patients were also significantly higher than the attack-free period levels (Table 2). Although there were no significant differences between the PCT levels of the attack-free periods and healthy control group, attack-free CRP, ESR, and fibrinogen levels were still significantly higher than the healthy control group levels (Table 3).
During the attack, only two patients had elevated PCT levels as is more than 0.5 ng/dl. The first patient was a 7.5-year-old boy who was followed up for 13 months and treated with colchicine. He was admitted with chest pain and right axillary lymphadenopathy. Other system examination and chest radiographic evaluation were normal. His hemoculture, urine, and throat cultures were negative. His PCT levels were 2.6, 0.29, and 0.05 ng/ml at the 6th hour of the attack, on the 7 days, and on the 3 months after the beginning of attack, respectively.
Second patient was a 3.5-year-old boy who was diagnosed newly. He had diffuse abdominal pain and had been kept under observation for possible appendicitis in the pediatric surgery department. However, abdominal ultrasonographic findings were not consistent with appendicitis. Other system examination was normal. His hemoculture, urine, and throat cultures were negative. His PCT level was 1.63 ng/ml at the 44th hour of attack. The levels of PCT decreased to 0.02 ng/ml on the 7 days. It was detected 0.03 ng/ml on 3 months after the attack.
Discussion
How PCT changes during the attack of FMF and after it is largely unknown. This is the first study which investigated the progress of PCT concentrations in the same FMF population during the attacks and attack-free periods. We showed that PCT levels increased slightly during the attacks of FMF patients. Meanwhile, increase of the traditional acute phase reactants such as CRP, fibrinogen, WBC, and ESR was much more significant.
During the last decade, PCT has become increasingly popular as a novel marker of inflammation which particularly is caused by severe infection. Recent studies showed that, under normal conditions, the levels of PCT in healthy subjects are very low (<0.05 ng/ml) [14]. The highest concentrations (≥10 ng/ml) are seen in systemic bacterial infections but have also been reported in multi-organ dysfunction as seen following trauma [8, 15, 16]. PCT concentrations between 2 and 10 ng/ml are suggestive of sepsis while levels between 0.5 and 2 ng/ml make sepsis possible but are also seen in other conditions. Although sepsis is unlikely with concentrations less than 0.5 ng/ml, such levels may still be consistent with localized infections [8]. In lower respiratory tract infections, PCT concentrations between 0.25 and 0.5 ng/ml may be seen [17].
However, a mild increase of PCT values could be observed in the patients with non-infectious inflammatory diseases such as systemic lupus erythematosus [18]. Until today, two studies which were evaluated PCT levels in patients with FMF have been reported. However, these studies did not compare PCT levels in same FMF patients during the attack and after the attack. One of the studies was performed by Colak et al. [19] and consisted of 41 adult FMF patients during the attack-free period and 31 healthy subjects. In this study, statistically significant difference between PCT levels of the FMF patients and healthy subjects was not found. PCT levels which were measured with LUMItest PCT kit (BRAHMS) were within the normal range in all patients and healthy control group (0.04 ng/ml vs. 0.045 ng/ml). As a result, the authors emphasized that the high PCT levels might be seen in FMF attacks [19]. The second study that was performed by Kisacik et al. [20] consisted of 28 FMF patients with acute abdominal attacks and 29 patients with acute appendicitis proven by clinical and pathologic examination. PCT levels were also measured by the BRAHMS PCT kit. They found that median PCT value of the FMF patients with attack was 0.1 ng/ml (range 0.06–0.21). Whereas, the median PCT value of the patients with acute appendicitis (0.55 ng/ml, range 0.26–0.70) was higher than the FMF patients with attack. PCT levels of the patients were not evaluated after the attack in this study [20].
We found that PCT levels during the attack were significantly higher than both PCT levels of the same patients during attack-free period and healthy control group. Although this difference was statistically significant (P = 0.04), median PCT values during the attack, after the attack, and in healthy subjects were lower than 0.05 ng/ml (Tables 1, 2, and 3). On the other hand, traditional acute phase reactants such as CRP, ESR, and fibrinogen were markedly higher than the controls. These results showed us that PCT cannot be used as a descriptive marker for attack in FMF patients instead of traditional acute phase reactants. However, we are aware of the limitation of our study such as small sample size.
In conclusion, we suggested that PCT values were far from useful for identification of FMF attacks, and PCT level was not conspicuously affected from inflammation of FMF. PCT might be useful in the differential diagnosis of some crucially state that might mimic FMF attacks such as severe bacterial infections. But, further studies should elucidate whether using the PCT could help in differential diagnosis of severe infections and FMF attacks.
References
Livneh A, Langevitz P (2000) Diagnostic and treatment concerns in familial Mediterranean fever. Baillieres Best Pract Res Clin Rheumatol 14:477–498
Ben-Chetrit E, Levy M (1998) Familial Mediterranean fever. Lancet 351:659–664
Korkmaz C, Ozdogan H, Kasapçopur O, Yazici H (2002) Acute phase response in familial Mediterranean fever. Ann Rheum Dis 61:79–81
Schaner PE, Gumucio DL (2005) Familial Mediterranean fever in the post-genomic era: how an ancient disease is providing new insights into inflammatory pathways. Curr Drug Targets Inflamm Allergy 4:67–76
Yalçinkaya F, Cakar N, Acar B, Tutar E, Güriz H, Elhan AH, Oztürk S, Kansu A, Ince E, Atalay S, Girgin N, Doğru U, Aysev D, Ekim M (2007) The value of the levels of acute phase reactants for the prediction of familial Mediterranean fever associated amyloidosis: a case control study. Rheumatol Int 27:517–522
Nijsten MW, Olinga P, The TH, de Vries EG, Koops HS, Groothuis GM, Limburg PC, ten Duis HJ, Moshage H, Hoekstra HJ, Bijzet J, Zwaveling JH (2000) Procalcitonin behaves as a fast responding acute phase protein in vivo and in vitro. Crit Care Med 28:458–461
Oberhoffer M, Stonans I, Russwurm S, Stonane E, Vogelsang H, Junker U, Jäger L, Reinhart K (1999) Procalcitonin expression in human peripheral blood mononuclear cells and its modulation by lipopolysaccharides and sepsis-related cytokines in vitro. J Lab Clin Med 134:49–55
Schneider HG, Lam QT (2007) Procalcitonin for the clinical laboratory: a review. Pathology 39:383–390
Breda L, Nozzi M, De Sanctis S, Chiarelli F (2010) Laboratory tests in the diagnosis and follow-up of pediatric rheumatic diseases: an update. Semin Arthritis Rheum 40:53–72
Eberhard OK, Haubitz M, Brunkhorst FM, Kliem V, Koch KM, Brunkhorst R (1997) Usefulness of procalcitonin for differentiation between activity of systemic autoimmune disease (systemic lupus erythematosus/systemic antineutrophil cytoplasmic antibody-associated vasculitis) and invasive bacterial infection. Arthritis Rheum 40:1250–1256
Gendrel D, Raymond J, Coste J, Moulin F, Lorrot M, Guérin S, Ravilly S, Lefèvre H, Royer C, Lacombe C, Palmer P, Bohuon C (1999) Comparison of procalcitonin with C-reactive protein, interleukin 6 and interferon-alpha for differentiation of bacterial versus viral infections. Pediatr Infect Dis J 18:875–881
Schwenger V, Sis J, Breitbart A, Andrassy K (1998) CRP levels in autoimmune disease can be specified by measurement of procalcitonin. Infection 26:274–276
Meisner M (2000) Procalcitonin. Georg Theime Verlag, Stuttgart
http://www.procalcitonin.com/. Accessed 18 June 2011
Delèvaux I, André M, Colombier M, Albuisson E, Meylheuc F, Bègue RJ, Piette JC, Aumaître O (2003) Can procalcitonin measurement help in differentiating between bacterial infection and other kinds of inflammatory processes? Ann Rheum Dis 62:337–340
Wanner GA, Keel M, Steckholzer U, Beier W, Stocker R, Ertel W (2000) Relationship between procalcitonin plasma levels and severity of injury, sepsis, organ failure, and mortality in injured patients. Crit Care Med 28:950–957
Christ-Crain M, Jaccard-Stolz D, Bingisser R, Gencay MM, Huber PR, Tamm M, Müller B (2004) Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster-randomised, single-blinded intervention trial. Lancet 363:600–607
Quintana G, Medina YF, Rojas C, Fernandez A, Restrepo JF, Rondon F, Iglesias A (2008) The use of procalcitonin determinations in evaluation of systemic lupus erythematosus. J Clin Rheumatol 14:138–142
Colak B, Gurlek B, Yegin ZA, Deger SM, Elbek S, Pasaoglu H, Dogan I, Ozturk MA, Unal S, Guz G (2008) The relationship between the MEFV genotype, clinical features, and cytokine-inflammatory activities in patients with familial mediterranean fever. Ren Fail 30:187–191
Kisacik B, Kalyoncu U, Erol MF, Karadag O, Yildiz M, Akdogan A, Kaptanoglu B, Hayran M, Ureten K, Ertenli I, Kiraz S, Calguneri M (2007) Accurate diagnosis of acute abdomen in FMF and acute appendicitis patients: how can we use procalcitonin? Clin Rheumatol 26:2059–2062
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yüksel, S., Ekim, M., Özçakar, Z.B. et al. The value of procalcitonin measurements in children with familial Mediterranean fever. Rheumatol Int 32, 3443–3447 (2012). https://doi.org/10.1007/s00296-011-2206-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-011-2206-2