Abstract
The aim of this study is to investigate visfatin levels in both synovial fluid (SF) and plasma of patients with primary knee osteoarthritis (OA) and its relationship with biomarkers of cartilage degradation in SF. Thirty OA patients, 12 SF control, and 12 plasma control subjects were enrolled in this study. Visfatin levels in both SF and plasma were measured using enzyme-linked immunosorbent assay (ELISA). Degradation biomarkers of collagen II and aggrecan in SF were also measured. The radiographic grading of OA in the knee was performed by the Kellgren-Lawrence (KL) criteria. Compared to controls, OA patients had higher SF visfatin concentration (8.95 ± 2.5 vs. 4.48 ± 2.49 ng/ml, P < 0.001). SF visfatin levels in KL grade 4 were significantly elevated compared with those of KL grade 3 (10.57 ± 2.49 vs. 7.54 ± 1.5 ng/ml, P = 0.001). SF visfatin positively correlated with degradation biomarker of collagen II, CTX-II (r = 0.497, P = 0.005), and degradation biomarker of aggrecan, AGG1 (r = 0.451, P = 0.012) and AGG2 (r = 0.434, P = 0.017). These findings suggest that SF visfatin might involved in cartilage matrix degradation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is characterized by the progressive loss of articular cartilage and osteophytes formation that leads to chronic pain and functional restrictions in affected joints [1]. The pathology of OA involves the whole joint in a degenerative process that includes the menisci, ligaments, periarticular muscles, joint capsule, and the infrapatellar fat [2]. Obesity is a potent risk factor for the development and progression of OA [3–5]. Considerable evidence indicates that adipose factors may provide a metabolic link between obesity and OA [6]. Ushiyama et al. [7] found that the potential role of adipose-derived proteins in OA is emphasized by the ability of the infrapatellar fat pad, which is situated intracapsularly and extrasynovially in the knee joint, to produce cytokines.
Adipose tissue expresses and secretes a large number of proteins that often share functional and structural properties of cytokines and are there classified as adipokines [8]. These include leptin, adiponectin, resistin, visfatin, and others. These factors are associated with inflammation and immune response. Recently, many studies suggest that local changes of adipokines concentrations in the joint cavity may have important pathophysiological implications on cartilage metabolism. Leptin, adiponectin, and resistin have been detected in the synovial fluid (SF) obtained from patients with OA. Dumond et al. [9] demonstrated that leptin expression was up-regulated in osteophytes and cartilage of OA, especially in areas of matrix depletion, fibrillations, and chondrocyte clusters. Moreover, Ku et al. [10] reported that SF leptin concentrations were closely related to the radiographic severity of OA, suggesting that SF leptin levels could be used as an effective marker for quantitative detection of OA. Schäffler et al. [11] found a positive correlation between resistin and systemic inflammation markers in SF level. Adiponectin has been shown to exert anti-diabetic, anti-atherogenic, and anti-inflammatory properties [12]. Senolt et al. [13] reported that increased adiponectin is negatively linked to the local inflammatory process in patients with rheumatoid arthritis (RA). In our previous study, we have demonstrated that adiponectin level in SF might involve in the regulation of cartilage degradation in OA [14].
Visfatin, also known as pre-B-cell colony-enhancing factor (PBEF) or nicotinamide phosphoribosyltransferase (NAMP), acts as an insulin analogue on the insulin receptor to exert mimetic insulin actions [15, 16]. Visfatin concentrations have been shown to be elevated in certain conditions. For example, the vast majority of cases of human obesity are associated with high circulating visfatin concentrations. This elevation has also been found in type 2 diabetes mellitus [17], polycystic ovary syndrome [18], and inflammation-related bone disease [19]. Moreover, Moschen et al. [20] had showed the proinflammatory and immunomodulating properties of visfatin. In addition, Rho et al. [21] found that serum visfatin concentrations increased in patients with RA than control subjects and positively correlated with levels of radiographic joint damage. Recent in vitro study investigated that visfatin triggered cartilage destruction by increasing matrix metalloproteinase (MMP)-3 and MMP-13, a disintegrin and metalloproteinase with thrombospondin motifs (ADAMTS)-4 and ADAMTS-5 in a dose-dependent manner in immature mouse articular chondrocytes, suggesting that visfatin affected articular cartilage metabolism [22]. But little is known about the relationship between visfatin and cartilage degradation in vivo. Here, we investigate visfatin levels in knee OA patients and control subjects and correlations between SF visfatin and cartilage degradation biomarkers.
Methods
Subjects
Thirty patients aged 55–79 years with primary knee OA according to the criteria of the American College of Rheumatology; 12 SF control and 12 plasma control individuals were enrolled in the present study. OA patients underwent total knee arthroplasty (TKA) at Peking Union Medical College Hospital (PUMCH). Twelve cases of SF in controls were from cadavers within 8 h after death, while 12 control plasma samples were obtained from health women, without history of joint disease. All the subjects were women. Ethical approval of this study was obtained from the Ethical Committee of Clinical Investigation of PUMCH. Written informed consent was received from all patients prior to their participation in the study.
The severity of the disease was determined using weight-bearing anteroposterior radiographs of the affected knee. Knee radiographs were evaluated according to the Kellgren-Lawrence (KL) criteria [23]. According to the KL grading scale, 16 patients were KL grade 3, whereas 14 patients were KL grade 4.
Analytical procedures
After aspirated, SF was centrifuged at 2,000×g for 10 min to remove cells and joint debris and stored immediately at −80°C until assayed. Plasma samples were also collected by direct venipuncture after an overnight fast. The concentrations of visfatin and cartilage degradation markers were determined in duplicate by enzyme-linked immunosorbent assay (ELISA). The ELISA kit for visfatin in plasma and SF was purchased from Adipobiotech (Beijing, China). The ELISA kits for SF C-terminal telopeptide of collagen type II (CTX-II), the degenerative fragment of type II collagen, and AGG1(G1-1H11) and AGG2(6D6-G2), two degenerative fragment of aggrecan, were obtained from Nordic Biotech (Beijing, China) as described in detail previously [24]. Dilution and spiking experiments were performed to validate the use of ELISA kits for SF samples. Samples were diluted as appropriate, and paired samples were assayed in the same run. The interassay and intraassay coefficients of variation, detection limits, and dilution factor for the four assays were listed in Table 1. The absorbance was read on an automated ELISA plate reader at 450 nm. Values were calculated from a standard curve. When the measured concentration in either sample was above the upper limit of quantification, the sample was further diluted to fall into the working range and re-measured.
Statistical analysis
The results are shown as mean ± SD. SPSS 13.0 for Windows was used for statistical analysis. Since the samples were not drawn from normally distributed population, comparisons of samples between OA patients and control subjects were made by the nonparametric Wilcoxon signed rank test. The analysis of statistical correlation was performed by the Spearman test of rank correlation. A P value >0.05 was considered to be significant.
Results
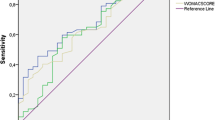
Table 2 showed the characteristics of OA patients and control subjects. The age and BMI had no significant difference between OA patients and control subjects. SF visfatin levels were significantly higher in OA patients than those in control subjects (8.95 ± 2.5 vs. 4.48 ± 2.49 ng/ml, P < 0.001). Plasma visfatin levels were higher in OA patients than those in control subjects, but not statistical significance (5.37 ± 1.45 vs. 4.93 ± 1.4 ng/ml, P = 0.466, Fig. 1).
In OA patients, the SF levels of visfatin were analyzed and compared in relation to radiological KL grading of OA. The SF levels of visfatin from KL grade 3 were 7.54 ± 1.5 ng/ml, and those from KL grade 4 were 10.57 ± 2.49 ng/ml. The data revealed that SF visfatin levels in KL grade 4 were significantly elevated compared with those of KL grade 3 (P = 0.001, Fig. 2).
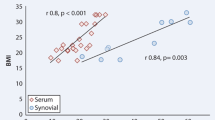
As to correlation analysis between SF visfatin level and cartilage degradation biomarkers, we found that SF visfatin is positively correlated with SF CTX-II (r = 0.497, P = 0.005). SF visfatin also correlated with SF aggrecan fragments AGG1 (r = 0.451, P = 0.012) and AGG2 (r = 0.434, P = 0.017) (Fig. 3).
Discussion
This study revealed a marked increase in visfatin levels in SF of patients with knee OA compared with the controls. With regards to joints, only recent finding demonstrated that articular adipose tissue and synovial fibroblasts from patients with OA are a local source of visfatin [25]. Elevated levels of visfatin in SF are also possibly caused by other inflammation cytokines, e.g., interleukin (IL)-1β [22]. Adipose tissue serves as an endocrine organ and secretes cytokines, interleukins, growth factors, and adipokines in endocrine, autocrine, or paracrine manner. These inflammation mediators are found in SF and are able to influence the cartilage and synovium metabolism [2, 26]. Previous studies demonstrated that OA synovial fibroblasts and chondrocyte express visfatin [22, 27]. Visfatin seems to have a proinflammatory effect on chondrocytes and synovial fibroblasts.
Cartilage damage is one of the main pathological changes in OA. Knee OA is characterized by depressed cartilage synthesis and increased cartilage degradation. However, this can be monitored by measurement of cartilage-derived synthesis and degradation products of matrix molecules released into SF and serum [28]. SF CTX-II and aggrecan fragments AGG1 and AGG2 levels directly represent articular cartilage status in OA. Our present study showed that SF CTX-II levels were significantly higher in OA patients than those in control subjects. SF aggrecan fragments AGG1 and AGG2 levels in OA patients were also higher than those in control subjects. MMPs and ADAMTs are major mediators of cartilage destruction. The MMPs were especially active in cleaving type II collagen, and the aggrecanases showed preference for cleaving aggrecan [29]. The critical site of aggrecan cleavage occurs within the interglobular domain (IGD) located between the globular domains G1 and G2 to release the glycosaminoglycan (GAG)-rich C terminus, which is important for the mechanical properties of the cartilage. The degenerative fragments of aggrecan in the present study have been identified in the media from bovine cartilage explants or chondrocytes stimulated with oncostatin M and tumor necrosis factor alpha (TNF-α). The results that were not reversed by MMP inhibitors demonstrate the assay’s specificity to the activities of aggrecanase [24]. Our study investigated that SF visfatin levels in OA had a higher concentration compared with controls and a significantly positive correlation with CTX-II and aggrecan fragments, AGG1 and AGG2 levels. These results in vivo are consistent with report that visfatin triggered cartilage destruction by increasing MMP-3 and MMP-13 and ADAMTS-4 (also known as aggrecanase-1) and ADAMTS-5 (aggrecanase-2) in a dose-dependent manner in vitro.
Visfatin was originally cloned by Samal et al. [30] in search of novel cytokine-like molecules isolated from human peripheral blood lymphocytes. They described a 52-kDa secreted PBEF/visfatin that enhanced the effect of IL-7 and stem cell factor on pre-B-cell colony formation. It was re-discovered by Fukuhara et al. [16] using a differential display technique to identify genes that are relatively specifically expressed in human abdominal fat. Visfatin is a highly conserved protein, and the death of mice lacking visfatin during embryogenesis highlights its physiologic importance. Visfatin activates insulin receptor and exerts insulin-mimetic effects in vivo and in vitro, but does not share the binding site with insulin on the insulin receptor. Its synthesis is regulated by cytokines such as TNFα, IL-1β, and IL-6, by lipopolysaccharide (LPS), by hypoxia, and by dexamethasone [31–34]. In addition, visfatin itself induces its own production in RA synovial fibroblasts, indicating the existence of a positive feedback-regulating mechanism [27]. Recent studies have demonstrated that visfatin was expressed in immune cells (e.g., neutrophils and macrophages), adipocytes, chondrocytes, and synovial fibroblasts and induced IL-1β, TNF-α, and IL-6 [20, 22, 27, 30, 35, 36]. Visfatin also have a proinflammatory effect on cartilage. Otero et al. [37] reported that patients with RA showed considerably higher plasma levels of visfatin than healthy controls. Brentano et al. [27] showed that serum and SF levels of visfatin in patients with RA had higher than those in patients with OA and visfatin was associated with serum markers of inflammation as well as clinical disease activity in RA. In addition, visfatin activated the transcription factor NF-κB and activator protein 1 and induced IL-6, IL-8, MMP-1, and MMP-3 in RA synovial fibroblast. Gosset et al. [22] showed that human OA chondrocytes produced visfatin and IL-1β stimulated visfatin mRNA production and protein expression in human articular chondrocyte from OA patients. Our study also investigated that SF visfatin levels in KL grade 4 were significantly elevated compared with those of KL grade 3, suggesting that SF concentration of visfatin is ascending with the progress of OA. These results indicate that visfatin may be a catabolic role in OA and might/may play a significant role in the pathophysiological course of OA.
This study has had several limitations. First, the sample size was not large enough to reach definitive conclusions. Secondly, we focused the investigation of KL grade 3 and 4 of OA. The OA sample collected in our study is only from TKA surgeries and less than grade 2 was none. Therefore, the conclusions are only valid for progression during the late stages of OA. Thirdly, our study was not a multi-central study.
In summary, the present study showed that patients with primary knee OA had higher levels of visfatin in SF compared with control subjects. SF visfatin level was significantly correlated with cartilage degradation markers. Therefore, SF visfatin could possibly serve as a biochemical parameter for reflecting cartilage matrix degradation of OA. Further studies are needed to elucidate the signaling pathways involved in cartilage degradation of OA.
References
Lorenz H, Richter W (2006) Osteoarthritis: cellular and molecular changes in degenerating cartilage. Prog Histochem Cytochem 40(3):135–163
Clockaerts S, Bastiaansen-Jenniskens YM, Runhaar J, Van Osch GJ, Van Offel JF, Verhaar JA et al (2010) The infrapatellar fat pad should be considered as an active osteoarthritic joint tissue: a narrative review. Osteoarthritis Cartilage. doi:10.1016/j.joca.2010.03.014
Felson DT, Zhang Y, Hannan MT, Naimark A, Weissman B, Aliabadi P et al (1997) Risk factors for incident radiographic knee osteoarthritis in the elderly: the Framingham Study. Arthritis Rheum 40(4):728–733
Marks R, Allegrante JP (2002) Body mass indices in patients with disabling hip osteoarthritis. Arthritis Res 4(2):112–116
Manek NJ, Hart D, Spector TD, MacGregor AJ (2003) The association of body mass index and osteoarthritis of the knee joint: an examination of genetic and environmental influences. Arthritis Rheum 48(4):1024–1029
Presle N, Pottie P, Dumond H, Guillaume C, Lapicque F, Pallu S et al (2006) Differential distribution of adipokines between serum and synovial fluid in patients with osteoarthritis. Contribution of joint tissues to their articular production. Osteoarthritis Cartilage 14(7):690–695
Ushiyama T, Chano T, Inoue K, Matsusue Y (2003) Cytokine production in the infrapatellar fat pad: another source of cytokines in knee synovial fluids. Ann Rheum Dis 62(2):108–112
Kershaw EE, Flier JS (2004) Adipose tissue as an endocrine organ. J Clin Endocrinol Metab 89(6):2548–2556
Dumond H, Presle N, Terlain B, Mainard D, Loeuille D, Netter P et al (2003) Evidence for a key role of leptin in osteoarthritis. Arthritis Rheum 48(11):3118–3129
Ku JH, Lee CK, Joo BS, An BM, Choi SH, Wang TH et al (2009) Correlation of synovial fluid leptin concentrations with the severity of osteoarthritis. Clin Rheumatol 28(12):1431–1435
Schäffler A, Ehling A, Neumann E, Herfarth H, Tarner I, Schölmerich J et al (2003) Adipocytokines in synovial fluid. JAMA 290(13):1709–1710
Trujillo ME, Scherer PE (2005) Adiponectin–journey from an adipocyte secretory protein to biomarker of the metabolic syndrome. J Intern Med 257(2):167–175
Senolt L, Pavelka K, Housa D, Haluzik M (2006) Increased adiponectin is negatively linked to the local inflammatory process in patients with rheumatoid arthritis. Cytokine 35(5–6):247–252
Hao D, Li M, Wu Z, Duan Y, Li D, Qiu G (2010) Synovial fluid level of adiponectin correlated with levels of aggrecan degradation markers in osteoarthritis. Rheumatol Int. doi:10.1007/s00296-010-1516-0
Busso N, Karababa M, Nobile M, Rolaz A, Van Gool F, Galli M et al (2008) Pharmacological inhibition of nicotinamide phosphoribosyltransferase/visfatin enzymatic activity identifies a new inflammatory pathway linked to NAD. PLoS One 3(5):e2267
Fukuhara A, Matsuda M, Nishizawa M, Segawa K, Tanaka M, Kishimoto K et al (2005) Visfatin: a protein secreted by visceral fat that mimics the effects of insulin. Science 307(5708):426–430
Chen MP, Chung FM, Chang DM, Tsai JC, Huang HF, Shin SJ et al (2006) Elevated plasma level of visfatin/pre-B cell colony-enhancing factor in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab 91(1):295–299
Panidis D, Farmakiotis D, Rousso D, Katsikis I, Delkos D, Piouka A et al (2008) Plasma visfatin levels in normal weight women with polycystic ovary syndrome. Eur J Intern Med 19(6):406–412
Moschen AR, Geiger S, Gerner R, Tilg H (2009) Pre-B cell colony enhancing factor/NAMPT/visfatin and its role in inflammation-related bone disease. Mutat Res Fundam Mol Mech Mutagen. doi:10.1016/j.mrfmmm.2009.06.012
Moschen AR, Kaser A, Enrich B, Mosheimer B, Theurl M, Niederegger H, Tilg H (2007) Visfatin, an adipocytokine with proinflammatory and immunomodulating properties. J Immunol 178(3):1748–1758
Rho YH, Solus J, Sokka T, Oeser A, Chung CP, Gebretsadik T et al (2009) Adipocytokines are associated with radiographic joint damage in rheumatoid arthritis. Arthritis Rheum 60(7):1906–1914
Gosset M, Berenbaum F, Salvat C, Sautet A, Pigenet A, Tahiri K et al (2008) Crucial role of visfatin/pre-B cell colony-enhancing factor in matrix degradation and prostaglandin E2 synthesis in chondrocytes: possible influence on osteoarthritis. Arthritis Rheum 58(5):1399–1409
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Wang B, Chen P, Jensen AC, Karsdal MA, Madsen SH, Sondergaard BC et al (2009) Suppression of MMP activity in bovine cartilage explants cultures has little if any effect on the release of aggrecanase-derived aggrecan fragments. BMC Res Notes. doi:10.1186/1756-0500-2-259
Chen WP, Bao JP, Feng J, Hu PF, Shi ZL and Wu LD (2010) Increased serum concentrations of visfatin and its production by different joint tissues in patients with osteoarthritis. Clin Chem Lab Med. doi:10.1515/cclm.2010.230
Toussirot E, Streit G, Wendling D (2007) The contribution of adipose tissue and adipokines to inflammation in joint diseases. Curr Med Chem 14(10):1095–1100
Brentano F, Schorr O, Ospelt C, Stanczyk J, Gay RE, Gay S et al (2007) Pre-B cell colony-enhancing factor/visfatin, a new marker of inflammation in rheumatoid arthritis with proinflammatory and matrix-degrading activities. Arthritis Rheum 56(9):2829–2839
Fraser A, Fearon U, Billinghurst RC, Ionescu M, Reece R, Barwick T et al (2003) Turnover of type II collagen and aggrecan in cartilage matrix at the onset of inflammatory arthritis in humans: relationship to mediators of systemic and local inflammation. Arthritis Rheum 48(11):3085–3095
Little CB, Meeker CT, Golub SB, Lawlor KE, Farmer PJ, Smith SM et al (2007) Blocking aggrecanase cleavage in the aggrecan interglobular domain abrogates cartilage erosion and promotes cartilage repair. J Clin Invest 117(6):1627–1636
Samal B, Sun Y, Stearns G, Xie C, Suggs S, McNiece I (1994) Cloning and characterization of the cDNA encoding a novel human pre-B-cell colony-enhancing factor. Mol Cell Biol 14(2):1431–1437
Jia SH, Li Y, Parodo J, Kapus A, Fan L, Rotstein OD et al (2004) Pre-B cell colony-enhancing factor inhibits neutrophil apoptosis in experimental inflammation and clinical sepsis. J Clin Invest 113(9):1318–1327
Kralisch S, Klein J, Lossner U, Bluher M, Paschke R, Stumvoll M et al (2005) Hormonal regulation of the novel adipocytokine visfatin in 3T3–L1 adipocytes. J Endocrinol 185(3):R1–R8
Kralisch S, Klein J, Lossner U, Bluher M, Paschke R, Stumvoll M et al (2005) Interleukin-6 is a negative regulator of visfatin gene expression in 3T3–L1 adipocytes. Am J Physiol Endocrinol Metab 289(4):E586–E590
Bae SK, Kim SR, Kim JG, Kim JY, Koo TH, Jang HO et al (2006) Hypoxic induction of human visfatin gene is directly mediated by hypoxia-inducible factor-1. FEBS Lett 580(17):4105–4113
McGlothlin JR, Gao L, Lavoie T, Simon BA, Easley RB, Ma SF et al (2005) Molecular cloning and characterization of canine pre-B-cell colony-enhancing factor. Biochem Genet 43(3–4):127–141
Luk T, Malam Z, Marshall JC (2008) Pre-B cell colony-enhancing factor (PBEF)/visfatin: a novel mediator of innate immunity. J Leukoc Biol 83(4):804–816
Otero M, Lago R, Gomez R, Lago F, Dieguez C, Gomez-Reino JJ et al (2006) Changes in plasma levels of fat-derived hormones adiponectin, leptin, resistin and visfatin in patients with rheumatoid arthritis. Ann Rheum Dis 65(9):1198–1201
Acknowledgments
The authors would like to thank Dr. Jin Lin, Jin Jin, and Xisheng Weng for their help in sample collections.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Duan, Y., Hao, D., Li, M. et al. Increased synovial fluid visfatin is positively linked to cartilage degradation biomarkers in osteoarthritis. Rheumatol Int 32, 985–990 (2012). https://doi.org/10.1007/s00296-010-1731-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-010-1731-8