Abstract
To evaluate kidney perfusion and diffusion in patients with systemic lupus erythematosus (SLE) and define any correlation between laboratory features of renal involvement and apparent diffusion coefficients (ADCs). We studied 35 patients with SLE and 30 healthy volunteers. Ten of the patients were diagnosed as having lupus nephritis. Transverse diffusion-weighted multisection echo-planar magnetic resonance imaging was created with the following diffusion gradient b values: 0, 111, 222, 333, 444, 556, 667, 778, 889, and 1,000 s/mm2. Statistical analyses to compare ADCs of kidneys between patients in the study and control groups were done with the independent sample t test. The Pearson correlation analysis was used to evaluate the relation between the renal function variables and the ADCs. There was statistically significant difference between the ADClow values and the urine protein levels (P < 0.05) in the patients with SLE. Also, there was a significant correlation between the duration of nephritis and urine protein levels in the patients with SLE (P < 0.01). There was no statistically significant differences regarding ADCs, serum creatinine levels, and GFRs among patients with SLE and controls. Our patients had mild SLE and this might be the reason that no statistically significant differences were found between ADCs, and laboratory features of renal involvement among patients with SLE and controls. Larger series and more diffusion experience may be valuable for future studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is an autoimmune rheumatic disease involving multiple organ systems. Nephritis is the most significant feature of SLE because kidney damage is a major threat to long-term survival [1]. Diffusion-weighted magnetic resonance imaging is used to show molecular diffusion, which is the Brownian motion of the spins in biologic tissues [2]. The apparent diffusion coefficient (ADC), a quantitative variable calculated from diffusion-weighted magnetic resonance images, combines the effects of capillary perfusion and water diffusion in the extracellular extravascular space [3]. Thoeny and associates [4] presented the feasibility and reproducibility of diffusion-weighted magnetic resonance imaging of kidneys in healthy volunteers and those with renal abnormalities.
The aim of this preliminary report was to evaluate kidney perfusion and diffusion in patients with SLE and define any correlation between laboratory features of renal involvement, glomerular filtration rates (GFR), 24-h urine protein levels, serum creatinine levels, and ADCs and to define if this noninvasive technique might give information about renal damage in SLE in early period of the disease.
Methods
We studied 41 patients with SLE. Nine patients were excluded because they had diabetes mellitus, hypertension, heart disease, and other renal diseases. The study group consists of 35 patients (mean age, 36.9 years; age range, 17–57 years; mean duration of disease, 41 months; range, 1–180 months) and 30 healthy volunteers. The patients with SLE diagnosed according to the American College of Rheumatology criteria for SLE (1997). Ten of the patients were diagnosed as having lupus nephritis as clinically. But none of our patients had renal biopsy, because it was not clinically indicated. The duration of the lupus nephritis ranged from 6 to 84 months. GFR was calculated by Cockcroft-Gault formula. The age of controls was matched with the age of study group.
Renal diffusion magnetic resonance imaging was performed using a magnet operating at 1.5-T MR (Philips Gyroscan, Intera, Holland) with a body coil.
Transverse diffusion-weighted multisection echo-planar magnetic resonance imaging was created with the following diffusion gradient b values: 0, 111, 222, 333, 444, 556, 667, 778, 889, and 1,000 s/mm2. The following parameters were used for this sequence: parallel imaging reduction factor of 2, 3100/74; section thickness, 5 mm; intersection gap, 1 mm; flip angle, 75°; next, 1; matrix size, 128 × 128; field of view, 380 mm × 380 mm; and rectangular field of view, 100. Fat saturation was used to avoid chemical shift artifacts. The whole sequence consisted of 20 sections, with an acquisition time of 2 min 22 s. ADC maps were calculated automatically with the magnetic resonance system. Total pixel area was between 90 and 110 mm2.
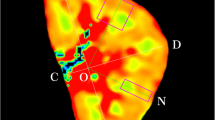
In the transverse ADC map, rectangular regions of interest were placed in the cortex on three parts (upper, middle, and lower poles) in each kidney. ADCs of the kidneys were calculated separately for the low (ADClow; b = 0, 111, 222, and 333 s/mm2), avarage (ADCavg; b = 444, 556, 667 s/mm2), and high (ADChigh; b = 778, 889, and 1,000 s/mm2) b values to allow differentiation between the relative influence of the perfusion fraction and the true diffusion. ADChigh shows almost only diffusion, whereas ADClow is composed of both diffusion and perfusion [2]. One radiologist blinded to the study results calculated the ADCs of each kidney in patients with SLE and volunteers (Figs. 1, 2). In addition, we evaluated the kidneys morphologically with the conventional MR images and excluded other pathologies such as cysts, focal scars, or mild hydronephrosis.
The ADCs (low, average, and high) of 130 kidneys were compared, and the relation between glomerular filtration rates (GFRs), 24-h urine protein levels (mg/24 h), serum creatinine levels (mg/dL), and ADCs were calculated. Statistical analyses to compare ADCs of kidneys between patients in the study and control groups were done with the independent sample t test. The Pearson product moment correlation analysis was used to evaluate the relation between the renal function variables (i.e., GFR, urine protein values, creatinine values, and duration of nephritis) and the ADCs. The Local Ethical Committee approved the study protocol, and written informed consent was obtained from all subjects before the study initiation.
Results
Table 1 shows the mean values of the different variables in the patients with SLE and controls. There were no statistically significant differences regarding ADCs, serum creatinine levels, and GFRs among the patients with SLE and controls. The only statistically significant difference between the patients with SLE and controls was based on the urine protein levels, which were higher in the patients with SLE (P < 0.01).
There was statistically significant difference between the ADClow values (both right and left) and the urine protein levels (P < 0.05) in the patients with SLE. If the urine protein levels increased, right ADClow and left ADClow values decreased in the patients with SLE. There was no significant correlation between creatinine values and GFRs and ADCs. In addition, there was a significant positive correlation between the values for right ADClow, right ADChigh, and the right ADCavg, and between the left ADClow, left ADChigh, and the left ADCavg (P < 0.001). There were statistically significant differences between creatinine levels and GFRs (P < 0.01) and between the duration of nephritis and the GFRs in the patients with SLE (P < 0.05). Also, there was a significant correlation between the duration of nephritis and urine protein levels in the patients with SLE (P < 0.01).
Discussion
Renal disease is one of the most significant causes of morbidity and mortality in patients with SLE. Glomerulonephritis is a major determinant of the course and prognosis of SLE [5]. Clinical and serologic indicators of renal involvement are proteinuria; active urinary sediment (i.e., pyuria, hematuria, or red cell casts in the absence of infection or other cause); accelerated hypertension; increased serum creatinine levels; decreased GFR, serum albumin, or C3 or C4 levels; increased anti-dsDNA antibody levels, and positive results on renal biopsy [6].
Diffusion-weighted magnetic resonance imaging is an established method routinely used to diagnose acute stroke. Diffusion-weighted magnetic resonance imaging of the kidneys gives information on renal function and the presence and degree of obstruction or inflammation. Fukuda and associates [7] showed decreased ADCs in patients with high serum creatinine levels when compared with those of normal values. In pigs with renal artery stenosis or ureteral obstruction, Müller and associates [8] observed a decrease in ADC. Similar findings were confirmed by Thoeny and associates in three human patients with ureteral obstruction. In a patient with acute pyelonephritis, Thoeny and associates [4] showed lower ADCs in the cortex and the medulla when compared with the normal kidney; this corresponds to zones of inflammation involving the papilla and the cortex. Namimoto and associates [9] reported that the cortexes of kidneys with renal artery stenosis had lower ADCs than those of the contralateral kidneys. Reduced blood perfusion, particularly in the cortex, may have caused this result. Yildirim previously reported a significant correlation between degree of stenosis and all ADCs, and that ADCs were lower in kidneys with renal artery stenosis than they were in the contralateral kidney [10].
To the best of our knowledge, our investigation is the first preliminary diffusion-weighted magnetic resonance imaging study to evaluate perfusion and diffusion of the kidneys in patients with SLE and healthy volunteers. Because of low creatinine levels and high GFRs, our patients were considered to have mild SLE. We found no statistically significant difference of ADCs, serum creatinine levels, GFRs between patients with SLE and controls. Thoeny and associates showed that when patients with renal failure were divided into two groups according to serum creatinine level (an arbitrary threshold of 2.5 mg/dL was used), that patients with levels lower than 2.5 mg/dL had lower ADC values (except the ADC high in medulla) than did controls. ADC values (except for the ADChigh in the medulla) were significantly higher in patients with creatinine levels greater than 2.5 mg/dL than the threshold than they were in controls [4]. The low serum creatinine levels in patients and controls demonstrate an overlap of the ADCs for the kidneys in the Thoeny study and our study.
GFR is the best indicator of the level of kidney function [11, 12]. The GFR must decline to about one half of its normal level before the serum creatinine concentration rises above the upper limit of normal. National Kidney Foundation definition of chronic kidney disease includes a GFR below 60 mL/min for 3 months or more. Minor elevations in serum creatinine concentration may represent a substantial reduction in GFR. Thus, using only serum creatinine as the measure of kidney function, it is difficult to estimate the level of kidney function and to detect the early stages of chronic kidney disease [12].
In our preliminary study, there was no significant correlation between GFRs and ADCs. A statistically significant difference was found between creatinine level and GFR (P < 0.01) and between the duration of nephritis and GFR (P < 0.05). The highest creatinine level found in our patients with SLE was 1.1 mg/dL, which may have been related to the fact that there was no significant correlation between creatinine values and ADCs or between GFRs and ADCs. In addition, GFRs greater than 56 mL/min might have contributed to these results.
We found a statistically significant difference between values for right and left ADClow and urine protein levels (P < 0.05) in patients with SLE. In addition, there was significant correlation between the duration of nephritis and the urine protein levels in patients with SLE (P < 0.01). In our patients with SLE, if urine protein levels increased, the values for right ADClow and left ADClow decreased. In our patients, the highest proteinuria level was 1,495 mg/dL and the lowest level was 24 mg/dL. This strong relation between the values for ADClow and the urine protein levels may show that values for ADClow are more sensitive than values for ADChigh or ADCavg when evaluating kidney involvement in patients with SLE, and values for ADClow, which give information on both perfusion and diffusion, may change firstly than other ADC values. This might help demonstrate of initially period of kidney involvement in patients with SLE had normal serum creatinine levels and normal GFRs but with proteinuria which may be more important than serum creatinine levels and GFR levels.
There was a significant positive correlation between the right values for ADClow, right ADChigh, and right ADCavg and between values for left ADClow, left ADChigh, and left ADCavg (P < 0.001). These results show a concordance between measurements of the right and left kidneys in the patients with SLE.
There are limitations of our study. First, the number of patients studied was small. According to renal function parameters, our patients had mild SLE. This might have been the reason that no statistically significant differences were found regarding ADCs, serum creatinine levels, and GFRs among patients with SLE and controls. In addition, only confirmation of renal lupus was proteinuria in our study.
This preliminary study reports our initial experience. Larger series and more diffusion experience may be valuable for future studies using diffusion-weighted magnetic resonance imaging to evaluate kidney involvement in patients with SLE.
References
Hahn BH (1993) Management of systemic lupus erythematosus. In: Kelley WN, Harris ED, Ruddy S, Sledge CB (eds) Textbook of rheumatology, 4th edn. WB Saunders, Philadelphia, pp 1043–1049
Schoenberg SO, Rieger JR, Michaely HJ, Rupprecht H, Samtleben W, Reiser MF (2006) Functional magnetic resonance imaging in renal artery stenosis. Abdom Imaging. 31(2):200–212
Le Bihan D, Breton E, Lallemand D, Aubin ML, Vignaud J, Laval-Jeantet M (1988) Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging. Radiology 168(2):497–505
Thoeny HC, De Keyzer F, Oyen RH, Peeters RR (2005) Diffusion-weighted MR imaging of kidneys in healthy volunteers and patients with parenchymal diseases: initial experience. Radiology 235(3):911–917
Lefkowith JB, Gilkeson GS (1996) Nephritogenic autoantibodies in lupus: current concepts and continuing controversies. Arthritis Rheum 39(6):894–903
Hay EM, Bacon PA, Gordon C, Isenberg DA, Maddison P, Snaith ML, Symmons DP, Viner N, Zoma A (1993) The BILAG index: a reliable and valid instrument for measuring clinical disease activity in systemic lupus erythematosus. Q J Med 86(7):447–458
Fukuda Y, Ohashi I, Hanafusa K, Nakagawa T, Ohtani S, An-naka Y, Hayashi T, Shibuya H (2000) Anisotropic diffusion in kidney: apparent diffusion coefficient measurements for clinical use. J Magn Reson Imaging 11(2):156–160
Müller MF, Prasad PV, Bimmler D, Kaiser A, Edelman RR (1994) Functional imaging of the kidney by means of measurement of the apparent diffusion coefficient. Radiology 193(3):711–715
Namimoto T, Yamashita Y, Mitsuzaki K, Nakayama Y, Tang Y, Takahashi M (1999) Measurement of the apparent diffusion coefficient in diffuse renal disease by diffusion-weighted echo-planar MR imaging. J Magn Reson Imaging 9(6):832–837
Yildirim E, Kirbas I, Teksam M, Karadeli E, Gullu H, Ozer I (2008) Diffusion-weighted MR imaging of kidneys in renal artery stenosis. Eur J Radiol 65(1):148–153
Johnson CA, Levey AS, Coresh J, Levin A, Lau J, Eknoyan G (2004) Clinical practice guidelines for chronic kidney disease in adults: part I. Definition, disease stages, evaluation, treatment, and risk factors. Am Fam Physician 70(5):869–876
National Kidney Foundation (2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39(21):S1–S266
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karadeli, E., Ulu, E.M.K., Yildirim, E. et al. Diffusion-weighted MR imaging of kidneys in patients with systemic lupus erythematosus: initial experience. Rheumatol Int 30, 1177–1181 (2010). https://doi.org/10.1007/s00296-009-1124-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-009-1124-z