Abstract
In this study, the relation between osteoporosis and vitamin D and the disease activity in patients with ankylosing spondylitis (AS) was investigated. A hundred patients with AS and 58 healthy individuals were included in the study. In addition to the routine blood and urine tests, serum 25-(OH)D3, parathormone (PTH), C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), total calcium, ionized calcium, and phosphorous levels of all participants were also measured. Bone mineral density (BMD) measurements were performed at the anterior–posterior and lateral lumbar and femur regions. Anterior–posterior and lateral thoracic and lumbosacral radiography was performed on all participants. The disease activity was evaluated by Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), functional status by Bath Ankylosing Spondylitis Functional Index (BASFI), and mobility by Bath Ankylosing Spondylitis Metrology Index (BASMI). In the patient group, BMD values obtained from the lateral lumbar and femur regions and serum vitamin D levels were lower than the control group. A negative relation was determined between the lateral lumbar BMD values and ESR, CRP, and BASDAI scores of patients with AS. The ESR, CRP levels, and BASMI scores of the AS patients with osteoporosis were significantly higher, when compared to patients without osteoporosis. The negative correlation between serum 25-(OH)D3 level and ESR, CRP levels did not reach a statistically significant level in patients with AS; the positive correlation between PTH levels and ESR, and the negative correlation between CRP and BASDAI also did not reach a statistically significant level. Vitamin D deficiency in AS may indirectly lead to osteoporosis by causing an increase in the inflammatory activity. The present authors believe that it would be beneficial to monitorize vitamin D levels together with BMD measurements in order to determine the patients under osteoporosis risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ankylosing spondylitis (AS) is a chronic, systemic, and inflammatory disease that characteristically involves the axial skeleton, enthesis regions, and in some patients the peripheral joints [1]. In the pathology of AS, inflammation and ossification play a primary role together and cause new bone formations in the spine and ankylosis. Also, osteoporosis accompanies these findings from the early stages of the disease, but the etiology of osteoporosis has not yet been completely clarified. It is thought that the immobilization and not using the spine due to spinal pain and/or movement restriction is causative factors in the development of osteoporosis [2]. Besides, medications used for treatment, hormonal disorders, and genetic factors also contribute to the development of osteopenia/osteoporosis. The relation between inflammatory activity and the loss of bone mass developing at a significant rate during the early stages of disease has been demonstrated [3–5].
It is suggested that high levels of proinflammatory cytokines, known to play a major role in chronic inflammation are also effective on osteoblasts and osteoclasts. It is thought that the inflammatory activity in AS also plays an important role in the pathophysiology of bone loss, this role being controlled by the substances that regulate both the inflammatory process and the bone turnover [6–9]. Another factor that is effective on the development of osteoporosis in AS is vitamin D. It was demonstrated that in patients with AS, the high disease activity was related with the alterations in vitamin D metabolism and increased bone resorption [4, 5]. It is also known that vitamin D plays a regulatory role on the immune system both at the cellular level and by the mediation of cytokines [10–15].
In this study, the relation between disease activity and osteoporosis and vitamin D levels in patients with AS was investigated.
Materials and methods
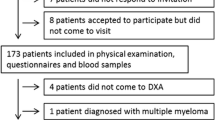
A hundred patients with the diagnosis of AS (75 males, 25 females) according to the Modified New York Criteria [16] and 58 healthy individuals (46 males, 12 females) as the control group were included in the study. The patients and the healthy individuals were informed about the study and informed consent was taken. The approval of the ethics committee was taken.
In the patient group, age, gender, occupation, educational status, duration of disease, peripheral joint involvement, extra-articular involvement, family history, the presence or absence of diabetes, hepatic and renal diseases, and history of operations were recorded.
The exclusion criteria for the patient and the control group were determined as associating inflammatory intestinal disease (Crohn’s disease, ulcerative colitis), malnutrition, hyperparathyroidism, hyperthyroidism, renal and hepatic disease, and medications that might affect bone metabolism and the endocrine system (such as thyroxin, anticonvulsants, glucocorticoids, hormone replacement therapy). The individuals with any inflammatory rheumatic disease were not included in the control group. All patients with AS and the control group were physically active for the last 12 months. All female individuals were in the premenopausal period. The individuals with a history of nonvertebral osteoporosis related fracture were not included in the study.
In the patient group, medication history was recorded. In order to determine the level of disease activity, Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) was used [17]. With the aim of identifying the patients’ functional levels, they were asked to complete the questionnaire of Bath Ankylosing Spondylitis Functional Index (BASFI) [18]. The validity and reliability of the Turkish versions of these forms have been approved [19, 20].
Heights and body weights of the patient and the control groups were measured and recorded and then their body mass indexes (BMI) were calculated. The physical examinations of the patients were performed and their spinal mobility was evaluated. For mobility evaluation, the criteria of Bath Ankylosing Spondylitis Metrology Index (BASMI) were used [21].
Laboratory analysis
Intact PTH (n = 1.6–6.9 pmol/l), bone-specific alkaline phosphatase (bone ALP, n = 9–116 IU/l), 25-(OH)D3 (n = 20–120 mmol/l) levels in the patient and the control groups were analyzed with standard methods. Also, C-reactive protein (CRP) with the nephelometric method (n = 0–5.0 mg/l), erythrocyte sedimentation rate (ESR) with the Westergren method, serum total calcium, ionized calcium, urea, creatinine, phosphorous, ALT, AST, total protein, and albumin levels were measured with the standard autoanalyzer.
Radiologic examinations and BMD measurement
In all participants, plain radiographs of lumbar and thoracic vertebras in lateral and anterior–posterior aspects were taken. All radiographs were evaluated by one radiologist and vertebral fractures were diagnosed by quantitative assessment method. According to this, if the height of the anterior, posterior, or mid-vertebra had decreased by least 15%, vertebral fracture would be diagnosed [22, 23].
Bone mineral density (BMD) of all participants was measured at the anteroposterior lumbar 1–4th, lateral lumbar 2–3rd vertebras and femur neck, Ward’s triangle, and total hip regions with the Hologic Discovery W series DEXA device and the results were evaluated as g/cm2.
Statistical analysis
All data were analyzed by SPSS 13.0 software. With the aim of evaluating the differences between groups, Student’s t test for the variables with a normal distribution and nonparametric Mann–Whitney U test for the variables with abnormal distribution were used. While studying the relations between the variables in the patient group, Pearson correlation test was used for parametric variables and Spearman correlation test was used for nonparametric variables. A P value of <0.05 was accepted as statistically significant.
Results
In this study, there were a total of 100 patients, 75 males and 25 females in the patient group and a total of 58 individuals, 46 males and 12 females, in the control group. The mean age of the patients was 39.9 ± 10.9 years old and the mean age of the control group was 38.1 ± 9.6 years old. The mean BMI of the patients was 26.05 ± 4.38 kg/cm2 while being 25.90 ± 4.50 kg/cm2 in the control group. No statistically significant difference was detected between groups in terms of age, gender distribution, and BMI (P > 0.05). In the patient group, duration of disease ranged between 6 months and 40 years (average 10.50 ± 7.84 years). Extra-articular involvement was present at 27 patients and in 49 patients, peripheral joint involvement particularly at the lower extremities was observed.
Among the investigated laboratory parameters, the mean ESR of patients was 26.31 ± 20.54 mm/h and the mean serum CRP level was 21.43 ± 19.90 mg/l. ESR and CRP values were significantly higher in the patient group, when compared with the control group (P < 0.0001). In the patient group, the mean 25-(OH)D3 level was 21.70 ± 12.17 mmol/l and in the control group, it was found as 32.70 ± 8.77 mmol/l, being significantly lower in the patient group (P < 0.0001). No statistically significant difference was found between groups in terms of PTH and bone-specific ALP values (P > 0.05). Total calcium and ionized calcium values were significantly lower in the patient group (P < 0.05 and P < 0.01, respectively). The demographic features and laboratory parameters of the patient and control groups are shown in Table 1.
When the characteristics of medications were investigated, all patients were receiving a nonsteroidal anti-inflammatory drug (NSAID). Ten patients were receiving only NSAIDs, while 68 patients were also receiving sulphasalazine (SSZ), 14 patients were receiving SSZ and methotrexate (MTX), 7 patients were receiving a biological agent, and 1 patient was receiving SSZ together with a biological agent. Twenty-eight patients had a past history of glucocorticoid intake, but for the last 12 months none of the patients had received such a medication.
In BMD measurements with the DEXA method, BMD values of the patient group obtained from lateral lumbar, femur total, neck, and Ward’s triangle regions were found to be significantly lower, when compared with the control group (P < 0.0001, P < 0.0001, P < 0.01, and P < 0.0001, respectively). No significant difference was noted between anterior–posterior lumbar measurements (P > 0.05). Results are shown in Table 2.
Plain radiographies of thoracic and lumbar vertebras revealed that in the patient group, compression fracture was found in at least one vertebra of the thoracic region in 16% and of the lumbar region in 3%. No fractures were detected in the control group.
Patients with AS were observed by further dividing into two groups as with or without osteoporosis according to lateral lumbar BMD values. A lateral lumbar BMD value of 0.650 g/cm2 was taken as the threshold and the patients who had lower values were accepted as osteoporosis (According to Hologic Inc., it corresponds to −2.5 T score for the age group of 30–40 years old). According to this, osteoporosis was found in 32% of patients with AS. In the AS patients with osteoporosis, ESR and CRP values were higher at a statistically significant level, when compared with the patients without osteoporosis (P < 0.05). No difference was found between groups in terms of 25-(OH)D3, PTH, and bone-specific ALP (P > 0.05), whereas total and ionized calcium levels were significantly lower in patients with osteoporosis (P < 0.05, P < 0.01). BASDAI scores were higher in patients with osteoporosis, but the difference between groups was not statistically significant (P > 0.05). The BASMI scores of patients with osteoporosis were significantly higher (P < 0.05). On the other hand, there was no difference between groups in terms of BASFI scores (P > 0.05). The results are given in Table 3.
In patients with AS, a negative correlation without statistical significance was noted between the serum 25-(OH)D3 level and ESR, CRP levels determining disease activity (r = −0.181, and r = −0.095, P > 0.05, respectively). However, no significant correlation was detected between 25-(OH)D3 and BASDAI scores (r = 0.011, P > 0.05). In patients, a positive correlation between PTH levels and ESR and a negative correlation without statistical significance between PTH levels, and CRP and BASDAI scores were found (r = 0.025, r = −0.067, and r = −0.066, P > 0.05, respectively).
While a negative correlation between duration of disease and bone-specific ALP (r = −0.228, P < 0.05) was detected, no significant relation with other laboratory parameters was found. There was a negative correlation between duration of disease and femur Ward’s triangle BMD values (r = −0.198, P < 0.05), and there was a positive correlation between anterior–posterior lumbar BMD values (r = 0.245, P < 0.05). Correlation was found between BASFI (r = 0.325, P < 0.01) and BASMI (r = 0.440, P < 0.0001) of Bath indexes and duration of disease. The laboratory parameters that correlated with duration of disease, Bath indexes, and BMD values are given in Table 4.
In terms of BMD measurements, a negative correlation was found only between parameters that are used to evaluate disease activity, namely ESR, CRP, and BASDAI scores and the lateral lumbar BMD values (r = −0.255, P < 0.05, r = −0.221, P < 0.05, r = −0.298, and P < 0.01, respectively). A negative correlation was found between BASDAI scores and anterior–posterior lumbar, femur neck, and femur total BMD values (r = −0.242, P < 0.05, r = −0.201, P < 0.05, r = −0.241, and P < 0.05, respectively). Except the lateral lumbar measurements, none of the other regions revealed a significant correlation with ESR and CRP values (P > 0.05). The results are summarized in Table 5.
Discussion
AS is a chronic, systemic, inflammatory disease with an unknown etiology, it belongs to the spondyloarthopathies group and is related with HLA-B27. Characteristically, it involves the axial skeleton and the enthesis regions and in some patients peripheral joints are also affected. AS has several extra-skeletal findings. Among these, eye involvement, cardiac, pulmonary, renal, and neurological involvement, and osteoporosis are important [1].
Bone mineral loss is a common finding in inflammatory rheumatic diseases. With the studies performed in recent years, osteoporosis, which is defined as the disorder of bone tissue microarchitecture and low bone mass, is accepted as a well-known finding of AS. Osteoporosis is frequently seen in both the early and the late stages of AS and may cause vertebral fractures [2, 24–27]. The prevalence of osteoporosis in AS is reported between 18.7% and 62% [24, 28]. Studies have shown that axial osteoporosis prevalence was high even in mild progression and early stages of AS, and it was stated to be responsible from the vertebral fractures in 4–18% of the cases [2, 25, 29, 30]. In this study, osteoporosis was found in 32% of the patients with AS. In the thoracic region of 16% of the patients and in the lumbar region of 3% of the patients, fracture was found in at least one vertebra.
The etiology of bone mineral loss in AS has not been completely clarified and in various studies, it was suggested that different mechanisms such as immobilization caused by pain and spinal restriction, inflammatory cytokines, genetic factors, glucocorticoids used for treatment, and NSAIDs have played a role [3, 4, 31]. It is thought that pain and restriction in the early stage and spinal ankylosing in the late stage cause immobility and thus creates a tendency to osteoporosis [32]. In previous studies, Meirelles et al. reported that in patients with AS, BMD values in the femur regions except the femur neck and in anterior–posterior lumbar regions were significantly lower, when compared with the control group [33]. Franck et al. found that the lumbar BMD values were similar to the control group in both male and female patients with AS, but the BMD values of total hip and femur neck were significantly lower, when compared with the control group [34]. Although negative effects of widely used NSAIDs have not been demonstrated on the bone metabolism in humans, few animal studies have reported that they may cause bone loss [32, 35, 36]. It is a well-known fact that systemic glucocorticoid therapy decreases BMD; however, its use in AS is limited. In this study, although all patients with AS and the control group had been physically active for the last 12 months and had not been receiving glucocorticoid therapy, the BMD values of the lateral lumbar region and femur, measured by the DEXA method were significantly lower in the patient group, when compared with the control group. No significant difference was detected in terms of anterior–posterior lumbar BMD values.
In previous studies, it was found that the decrease in the lumbar and femur neck BMD values detected in early stage of AS became more prominent in cases with slow progression; however, it patients at the late stage, although BMD of the femur neck decreased, the vertebral BMD increased [26, 30, 37]. Studies have reported that there is a relation between the duration of disease and anterior–posterior lumbar BMD values and BMD increases as the duration of disease increases [24, 26, 30, 33, 38]. Today, DEXA is the most preferred densitometry measurement method. In anterior–posterior measurements, besides the vertebral corpus, posterior elements and discs are also involved in the measured area; therefore, both cortical and trabecular bones are evaluated together [39]. Syndesmophytes, ligament calcifications, and fusion of the facet joints, which are characteristics of AS, increase the error rate in measurements and, particularly in late stage disease, lead to false high BMD values. In this study, it is considered that the positive correlation found between the duration of disease and anterior–posterior lumbar BMD measurement is due to this error. The fact that there is no relation between lateral lumbar BMD measurement and the duration of disease supports this consideration.
Thus, as it was stated before, with the lumbar lateral BMD measurements being superior in detecting the bone loss in the early stage [40, 41], the present authors believe that diagnosis of osteoporosis in either early or late stage AS patients would be more precise, without the need for proximal femur BMD values [32, 33, 42] and treatment could be started.
In recent studies, it was shown that vitamin D is effective not only on calcium, phosphorus, and bone metabolism, but also on the immune system [15, 43]. Amento et al. reported that vitamin D, being an endogenous immunomodulator leading to the suppression of active T cells and cell proliferation, may slow down the inflammatory process [12]. In their study investigating the relation between disease activity in AS and vitamin D, Lange et al. found that high disease activity and disorders in vitamin D metabolism are related with increased bone resorption [5]. In another study, in osteoporotic patients with AS, levels of ESR and CRP were significantly high while vitamin D level was low [4]. It was stated that with the lack of vitamin D, which is an endogenous immunomodulator, proliferation of the T cells and activation cannot be prevented and that the severity of inflammatory process may increase [4]. In this study, vitamin D levels in patients with AS were significantly lower, when compared with the control group. However, no significant relation was found between vitamin D and PTH levels and indicators of disease activity. This finding suggests that in addition to the link between vitamin D and disease activity, vitamin D may also play a role in the etiopathogenesis of this disease.
In their studies, Lange et al. [4] reported that in AS patients with osteoporosis, vitamin D level was significantly lower than AS patients without osteoporosis, whereas ESR and CRP levels were high. In this study, when AS patients with and without osteoporosis were compared, no significant difference was found in terms of vitamin D levels. In patients with osteoporosis, disease activity indicators ESR and CRP were significantly high, while total and ionized calcium levels were significantly low. Moreover, a negative correlation was detected between lateral lumbar BMD values and disease activity indicators ESR, CRP, and BASDAI. In the group with osteoporosis, BASMI scores were also significantly higher. These findings reveal that high disease activity plays a role in the etiology of osteoporosis developed in AS rather than vitamin D deficiency and that immobilization caused by movement restriction contributes to that process.
As a result, in this study, it was found that the incidence of osteoporosis increases in AS and this might be related with increased inflammatory activity and that vitamin D levels in patients with AS is lower, when compared with the control group. Performing BMD measurements regularly on all patients with AS in the early stage and later is important in order to prevent disability and vertebral fractures that may result in vital complications. Due to its immunomodulatory effects, vitamin D appears to be a hormone that has the potential of playing an important role in the etiopathogenesis of AS and in the control of inflammatory activity. The present authors believe that, in addition to the disease activity indicators, monitoring vitamin D levels would also be useful in order to determine the patients under osteoporosis risk.
References
Van Der Linden S, Van Der Hejide D, Braun J (2005) Ankylosing spondylitis. In: Harris ED, Budd RC, Frestein GS et al (eds) Kelley’s textbook of rheumatology. Elsevier Saunders, Philadelphia, PA, pp 1125–1141
Will R, Palmer R, Bhalla AK et al (1989) Osteoporosis in early ankylosing spondylitis: a primary pathological event? Lancet 2(8678–8679):1483–1485
Gratacos J, Collado A, Pons F et al (1999) Significant loss of bone mass in patients with early, active ankylosing spondylitis: a followup study. Arthritis Rheum 42(11):2319–2324
Lange U, Teichmann J, Strunk J et al (2005) Association of 1.25 vitamin D3 deficiency, disease activity and low bone mass in ankylosing spondylitis. Osteoporos Int 16(12):1999–2004
Lange U, Jung O, Teichmann J et al (2001) Relationship between disease activity and serum levels of vitamin D metabolites and parathyroid hormone in ankylosing spondylitis. Osteoporos Int 12(12):1031–1035
Manolagas SC (1995) Role of cytokines in bone resorption. Bone 17(2 Suppl):63S–67S
Pacifici R (1995) Cytokines and osteoclast activity. Calcif Tissue Int 56(Suppl 1):S27–S28
Nguyen L, Dewhirst FE, Hauschka PV et al (1991) Interleukin-1 beta stimulates bone resorption and inhibits bone formation in vivo. Lymphokine Cytokine Res 10(1–2):15–21
Fujita T, Matsui T, Nakao Y et al (1990) Cytokines and osteoporosis. Ann N Y Acad Sci 587:371–375
Baier R, Grauer A, Lazaretti-Castro M et al (1994) Differential effects of 1, 25-dihydroxyvitamin D3 on cell proliferation and calcitonin gene expression. Endocrinology 135(5):2006–2011
Muller K, Bendtzen K (1996) 1,25-Dihydroxyvitamin D3 as a natural regulator of human immune functions. J Investig Dermatol Symp Proc 1(1):68–71
Amento EP (1987) Vitamin D and the immune system. Steroids 49(1–3):55–72
Bouillon R, Okamura WH, Norman AW (1995) Structure-function relationships in the vitamin D endocrine system. Endocr Rev 16(2):200–257
Cantorna MT, Mahon BD (2005) D-hormone and the immune system. J Rheumatol Suppl 76:11–20
Deluca HF, Cantorna MT (2001) Vitamin D: its role and uses in immunology. Faseb J 15(14):2579–2585
van der Linden S, Valkenburg HA, Cats A (1984) Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum 27(4):361–368
Garrett S, Jenkinson T, Kennedy LG et al (1994) A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol 21(12):2286–2291
Calin A, Garrett S, Whitelock H et al (1994) A new approach to defining functional ability in ankylosing spondylitis: the development of the Bath Ankylosing Spondylitis Functional Index. J Rheumatol 21(12):2281–2285
Yanik B, Gursel YK, Kutlay S et al (2005) Adaptation of the Bath Ankylosing Spondylitis Functional Index to the Turkish population, its reliability and validity: functional assessment in AS. Clin Rheumatol 24(1):41–47
Ay S, Kutlay Ş, Kurtaiş Y (2004) Ankilozan Spondilitli Hastalarda Bath Ankilozan Spondilit Hastalık Aktivite İndeksinin (BASHAİ) Türkçe Versiyonunun Geçerlilik Ve Güvenirlik Çalışması. Romatizma (Acta Rheumatol Turcica) 19(3):139–146
Jenkinson TR, Mallorie PA, Whitelock HC et al (1994) Defining spinal mobility in ankylosing spondylitis (AS). The Bath AS Metrology Index. J Rheumatol 21(9):1694–1698
Melton LJIII, Lane AW, Cooper C et al (1993) Prevalence and incidence of vertebral deformities. Osteoporos Int 3(3):113–119
Ozoran K, Paker N, Basgoze O et al (1989) Calcitonin and calcium combined therapy in osteoporosis: effects on vertebra trabecular bone density. J Int Med Res 17(4):395–400
El Maghraoui A, Borderie D, Cherruau B et al (1999) Osteoporosis, body composition, and bone turnover in ankylosing spondylitis. J Rheumatol 26(10):2205–2209
Ralston SH, Urquhart GD, Brzeski M et al (1990) Prevalence of vertebral compression fractures due to osteoporosis in ankylosing spondylitis. BMJ 300(6724):563–565
Mullaji AB, Upadhyay SS, Ho EK (1994) Bone mineral density in ankylosing spondylitis DEXA comparison of control subjects with mild and advanced cases. J Bone Joint Surg Br 76(4):660–665
Lange U, Kluge A, Strunk J et al (2005) Ankylosing spondylitis and bone mineral density—what is the ideal tool for measurement? Rheumatol Int 26(2):115–120
Hanson CA, Shagrin JW, Duncan H (1971) Vertebral osteoporosis in ankylosing spondylitis. Clin Orthop Relat Res 74:59–64
Cooper C, Carbone L, Michet CJ et al (1994) Fracture risk in patients with ankylosing spondylitis: a population based study. J Rheumatol 21(10):1877–1882
Donnelly S, Doyle DV, Denton A et al (1994) Bone mineral density and vertebral compression fracture rates in ankylosing spondylitis. Ann Rheum Dis 53(2):117–121
Gratacos J, Collado A, Filella X et al (1994) Serum cytokines (IL-6, TNF-alpha, IL-1 beta and IFN-gamma) in ankylosing spondylitis: a close correlation between serum IL-6 and disease activity and severity. Br J Rheumatol 33(10):927–931
El Maghraoui A (2004) Osteoporosis and ankylosing spondylitis. Joint Bone Spine 71(4):291–295
Meirelles ES, Borelli A, Camargo OP (1999) Influence of disease activity and chronicity on ankylosing spondylitis bone mass loss. Clin Rheumatol 18(5):364–368
Franck H, Meurer T, Hofbauer LC (2004) Evaluation of bone mineral density, hormones, biochemical markers of bone metabolism, and osteoprotegerin serum levels in patients with ankylosing spondylitis. J Rheumatol 31(11):2236–2241
Saino H, Matsuyama T, Takada J et al (1997) Long-term treatment of indomethacin reduces vertebral bone mass and strength in ovariectomized rats. J Bone Miner Res 12(11):1844–1850
Jiang Y, Zhao J, Genant HK et al (1998) Bone mineral density and biomechanical properties of spine and femur of ovariectomized rats treated with naproxen. Bone 22(5):509–514
Devogelaer JP, Maldague B, Malghem J, Nagant de Deuxchaisnes C (1992) Appendicular and vertebral bone mass in ankylosing spondylitis. A comparison of plain radiographs with single- and dual-photon absorptiometry and with quantitative computed tomography. Arthritis Rheum 35(9):1062–1067
Reid DM, Nicoll JJ, Kennedy NS et al (1986) Bone mass in ankylosing spondylitis. J Rheumatol 13(5):932–935
Masud T, Langley S, Wiltshire P et al (1993) Effect of spinal osteophytosis on bone mineral density measurements in vertebral osteoporosis. BMJ 307(6897):172–173
Bronson WD, Walker SE, Hillman LS et al (1998) Bone mineral density and biochemical markers of bone metabolism in ankylosing spondylitis. J Rheumatol 25(5):929–935
Gilgil E, Kacar C, Tuncer T et al (2005) The association of syndesmophytes with vertebral bone mineral density in patients with ankylosing spondylitis. J Rheumatol 32(2):292–294
Bessant R, Keat A (2002) How should clinicians manage osteoporosis in ankylosing spondylitis? J Rheumatol 29(7):1511–1519
Selby P (2008) Rickets and osteomalacia. In: Hochberg MC (ed) Rheumatology. Mosby Elsevier, Amsterdam, pp 1977–1987
Conflict of interest
There is no conflict of interest regarding financial or other relationships.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mermerci Başkan, B., Pekin Doğan, Y., Sivas, F. et al. The relation between osteoporosis and vitamin D levels and disease activity in ankylosing spondylitis. Rheumatol Int 30, 375–381 (2010). https://doi.org/10.1007/s00296-009-0975-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-009-0975-7