Abstract
The objective of this study was to investigate the expression of IL-23 and IL-17 and the influence of IL-23 on IL-17 production in ankylosing spondylitis (AS) patients. IL-23 and IL-17 levels in the serum and supernatants of cultured peripheral blood mononuclear cells (PBMCs) were determined by ELISA. IL-23p19 mRNA expression in PBMCs were analyzed using RT-PCR. The patients with AS at active stage showed elevated levels of IL-23 and IL-17 in the serum and supernatants of cultured PBMCs. A higher expression of IL-23p19 mRNA in PBMCs of AS patients was also observed. A significantly enhanced production of IL-17 in the supernatants of cultured PBMCs was found in the presence of recombinant IL-23 and this effect was more significant in patients with AS. The results suggest that IL-23 and IL-17 may play critical roles in the pathogenesis of AS and IL-23-stimulated production of IL-17 by PBMCs may be responsible for the development of AS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
IL-23 is a heterodimeric protein that is a member of the IL-12 family of cytokines. It is composed of a unique p19 and a common p40 subunit that is shared with IL-12 [1]. IL-23 is produced by activated monocytes, activated antigen-presenting cells including DCs and macrophages, T cells, B cells and endothelial cells [1–4]. IL-23 plays a central role in the expansion and survival of IL-17-producing Th17 cells which are responsible for many inflammatory autoimmune diseases once attributed to Th1 cells [5, 6]. Recent studies have found that IL-23 was increased in patients with psoriasis and Behcet’s disease [2, 7]. The expression of IL-17 was upregulated in certain autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus, systemic sclerosis, psoriasis and inflammatory bowel disease [8–14]. IL-23 and IL-17 have been shown to play critical roles in the development and maintenance of autoimmune inflammation [5, 6, 15–20]. The mechanisms by which IL-23 induces autoimmunity are not completely understood. Accumulating evidences indicate that IL-17 may be one of the important effectors involved in these mechanisms.
Ankylosing spondylitis (AS) is an autoimmune disease characterized by inflammatory back pain, asymmetrical peripheral oligoarthritis (predominantly of the lower limbs), enthesitis, and specific organ involvement such as anterior uveitis, psoriasis and chronic inflammatory bowel disease. The cause of AS is unknown now. The two central features that deserve explanation are inflammation and new bone formation, especially in the spine [21]. Although previous studies suggested that IL-23 and IL-17 may play critical roles in certain autoimmune diseases, it is not clear whether they are involved in AS yet. Our study was therefore designed to examine the expression of IL-23 and IL-17 and the effect of IL-23 on the production of IL-17 by peripheral blood mononuclear cells (PBMCs) from AS patients. In this study, our results showed that IL-23 and IL-17 levels in the serum and supernatants of PBMCs were significantly higher in AS patients compared with normal controls. IL-23p19 mRNA expression in PBMCs was markedly up-regulated in AS patients. Recombinant (r) IL-23 could promote higher IL-17 production of PBMCs in AS patients than in normal controls. Taken together, our findings suggest that IL-23 and IL-17 may play critical roles in the development of AS.
Materials and methods
Patients
This study was approved by the ethics committee of the third affiliated hospital of Sun Yat-Sen University. Informed consent was obtained from all patients and control subjects. Fifty-seven patients with AS disease (52 men and 5 women) with an average age of 29.7 years and 38 healthy individuals (30 men and 8 women) with an average age of 27.7 years were included in the study. All AS patients were diagnosed according to the New York modified criteria [22]. Eighteen patients were diagnosed for the first time and all the patients’ BASDAI were no <4 when taken blood samples.
Cell isolation and culture
The PBMCs were prepared from heparinized venous blood by Ficoll–Hypaque density-gradient centrifugation. Cells were grown in RPMI1640 medium (Gibco, USA) supplemented with 10% fetal bovine serum (FBS, Gibco, USA) at an initial density of 2 × 106 cells/ml. To study the production of IL-23, isolated PBMCs were divided into two aliquots: one was stimulated with or without Staphylococcus aureus Cowan Ι (SAC, Sigma, USA) (0.02%) for 4 h and analyzed for IL-23p19 subunit using RT-PCR, and the other was stimulated for 48 h and subsequently used for IL-23 analysis by ELISA. For determination of IL-17 production, isolated PBMCs were cultured in the presence or absence of rIL-23 (50 ng/ml) (R & D Systems, USA) for 72 h.
ELISA for IL-23 and IL-17
The concentrations of IL-23 in the serum and supernatants were assayed using a human IL-23 ELISA kit (Bender MedSystems, Austria). The concentrations of IL-17 in the serum and the collected supernatants were measured using a human IL-17 ELISA kit (R & D Systems, USA).
RNA preparation and RT-PCR
Total RNA was extracted from PBMCs using Trizol Reagent (Invitrogen). After precipitation with isopropanol and washing with 75% ethanol, the RNA pellets were dissolved in diethylpyrocarbonate-treated water. mRNA from 1 μg of total cellular RNA was reversed and transcribed using the RevertAid™ First Strand cDNA Synthesis Kit (Fermentas) in 20 μl final volume reactions containing oligo dT18, 5× reaction buffer, Ribobock™ Ribonuclease, dNTP and M-Mulv. PCR amplificaton of cDNA aliquots was performed by adding 1.25 mM of each dNTP, 1.25 U Taq DNA polymerase (Takara) and 20 μM of sense and antisense primers. The reaction was done in 25 μl of PCR buffer (15 mM MgCl2, 500 mM KCl, 100 mM Tris–HCl, pH 8.3). The sense and antisense primers used in this experiment were: IL-23p19: sense 5′-TGT GGA GAT GGC TGT GAC-3′, antisense 5′-TTG AAG CGG AGA AGG AGA-3′, β-actin: sense 5′-GGA CTT CGA GCA AGA GAT GG-3′, antisense 5′-TGT GTT GGC GTA CAG GTC TTT G-3′. The expected product lengths were 275 bp for p19 and 229 bp for β-actin. Reactions were processed in a DNA thermal cycler as follows: 94°C for 5 min followed by 30 cycles of: 30 s of denaturation at 94°C, 45 s of annealing at 55°C for IL-23p19 and at 58°C for β-actin, followed by 45 s of elongation at 72°C. Finally, the PCR products were fully extended by incubation at 72°C for 5 min. PCR products were run on a 1.8% agarose gel and stained with ethidium bromide. The level of mRNA expression was presented as a ratio of IL23p19 PCR product over β-actin product.
Statistical analysis
Data were expressed as mean ± SD. Statistical analysis was performed using Student t test. A level of P < 0.05 was considered to be statistically significant.
Results
Levels of IL-23 in the serum and supernatants of cultured PBMCs of AS patients and normal control subjects
Serum IL-23 levels were significantly higher in AS patients (n = 39) than those in normal control subjects (n = 20; P < 0.001; Fig. 1a). The expression of IL-23 in the supernatants of PBMCs being cultured 48 h in AS patients (n = 8) were significantly higher than that in normal control subjects (n = 8; P = 0.002) as well. IL-23 production was significantly increased in the presence of SAC stimulation, with a higher upregulation in AS patients than in normal control subjects (P < 0.001; Fig. 1b).
IL-23 levels in the serum and supernatants of cultured PBMCs. a IL-23 levels in the serum of AS patients (n = 39) and normal control subjects (n = 20) measured by ELISA. b IL-23 levels in the supernatants of cultured PBMCs from AS patients (n = 8) and normal control subjects (n = 8) determined by ELISA. Separated PBMCs were cultured with or without SAC (0.02%) for 48 h. Data are represented as mean ± SD. *P < 0.001 compared with normal control subjects. # P < 0.01 compared with normal control subjects
Expression of IL-23p19 mRNA in PBMCs of AS patients and normal control subjects
We investigated IL-23p19 mRNA expression of PBMCs in AS patients and normal control subjects. The expression of IL-23p19 mRNA was normalized by respective β-actin mRNA. The average intensity ratio of IL-23p19 PCR product/β-actin product (0.466 ± 0.152) in AS patients (n = 8) was significantly higher than that in normal control subjects (0.226 ± 0.048; n = 8; P = 0.003; Fig. 2a). Moreover, IL-23p19 mRNA was also markedly higher in AS patients (0.972 ± 0.116) than that in normal control subjects (0.480 ± 0.269; P < 0.001) after stimulation with SAC (Fig. 2b). Data were represented as mean ± SD.
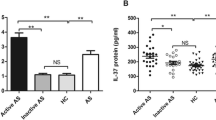
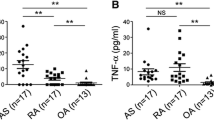
Concentrations of IL-17 in the serum and supernatants of cultured PBMCs of AS patients and normal control subjects and effect of IL-23 on the production of IL-17
IL-17 levels in serum were significantly higher in AS patients (n = 39) than those in normal control subjects (n = 20; P < 0.001; Fig. 3a). Although very low levels of IL-17 were detected in the supernatants of PBMCs being cultured 72 h, a significantly higher expression was noted in AS patients (n = 10) than that in normal control subjects (n = 10; P < 0.001; Fig. 3b).
IL-17 levels in the serum and supernatants of cultured PBMCs. a IL-17 levels in the serum of AS patients (n = 39) and normal control subjects (n = 20) measured by ELISA. b IL-17 production by cultured PBMCs from AS patients (n = 10) and normal control subjects (n = 10). Cells were cultured in the presence or absence of rIL-23 for 72 h. *P < 0.001 compared with normal control subjects; # P < 0.01 compared with medium. Data are represented as mean ± SD. *P < 0.001 compared with normal control subjects, # P < 0.01 compared with medium
To examine the influence of rIL-23 on the production of IL-17, PBMCs separated from five healthy individuals were cultured in the presence of rIL-23 (0, 1, 10, 50, 100 ng/ml) for 72 h. The results showed that the production of IL-17 was augmented significantly at dose of 50 ng/ml of rIL-23 (P = 0.028; Fig. 4) and this concentration was therefore used for subsequent experiments. The similarly stimulatory effect of IL-23 on IL-17 production was also seen in stimulated PBMCs of AS patients (P = 0.005). This effect was more pronounced in AS patients than in normal control subjects (P < 0.001; Fig. 3b).
Recombinant IL-23 induces IL-17 production by PBMCs from normal control subjects (n = 5). PBMCs were cultured in the presence or absence of rIL-23 (0, 1, 10, 50, 100 ng/ml) for 72 h. The concentrations of IL-17 in the supernatants of cultured PBMCs were measured by ELISA. Data are expressed as mean ± SD. *P < 0.05 compared with 0 ng/ml
Discussion
In the present study, we found elevated levels of IL-23 and IL-17 in the serum and supernatants of cultured PBMCs of AS patients. Moreover, an increased expression of IL-23p19 mRNA was also found in PBMCs of AS patients. Furthermore, we observed that IL-23 could promote IL-17 production by PBMCs of AS patients and normal control subjects. IL-23 stimulated a considerably higher production of IL-17 by PBMCs of AS patients than of normal control subjects. These results suggest that IL-23 and IL-17 may be involved in the pathogenesis of AS and IL-23 may play a unique role possibly through promoting the secretion of IL-17.
To study whether IL-23 is involved in the development of AS patients, we first assayed its levels in the serum of AS patients and normal control subjects. We found that serum IL-23 levels were markedly increased in AS patients. Because IL-23 is primarily produced by activated antigen-presenting cells that are present in PBMCs, we further assayed the production of IL-23 by PBMCs [23]. It has been reported that IL-23 is composed of a unique p19 and a common p40 subunit shared with IL-12 [1]. Therefore, we only examined the IL-23p19 mRNA expression in PBMCs by RT-PCR. The results showed an increased expression of IL-23p19 mRNA in PBMCs of AS patients than that of normal control subjects. We also observed a similar result for the IL-23 level in the supernatants of unstimulated cultured PBMCs. As previous study has shown that SAC was a potent stimulator for IL-23 secretion [23], we further tested the production of IL-23 by PBMCs stimulated by SAC. The results showed that both IL-23 levels in the supernatants of cultured PBMCs and IL-23p19 mRNA in PBMCs were markedly increased in AS patients and normal control subjects following stimulation with SAC. Moreover, the SAC-induced upregulation of IL-23 and IL-23p19 mRNA was significantly increased in AS patients. Our studies revealed a strong association between elevated levels of IL-23 and AS. These results suggest that IL-23 may be actively involved in the pathogenesis of AS.
IL-17 has been claimed to function as an effector cytokine primarily induced by IL-23 [16, 24, 25]. To investigate whether the upregulated IL-23 in AS patients promotes the disease via induction of IL-17, we measured its production in patients and controls. An elevated level of IL-17 in the serum was observed in AS patients than in normal control subjects. Furthermore, we assayed IL-17 production by PBMCs from AS patients and normal control subjects. The results showed a significantly increased production of IL-17 in the supernatants of PBMCs in AS patients compared with normal control subjects. Because CD4+ T cells play an essential role in the development of autoimmune diseases and have been indicated highly pathogenic on some autoimmune disease models, such as experimental autoimmune encephalomyelitis and collagen-induced arthritis, it will be more instructive to address IL-17 production by CD4+ T cells in AS patients [24–27].
As IL-23 and IL-17 were coincidently increased in AS patients and IL-17 can be induced by IL-23, we further examined whether IL-23 could enhance the production of IL-17 in AS. Our findings showed that IL-23 could induce PBMCs to secrete IL-17 in AS patients and normal control subjects. More importantly, IL-23-induced IL-17 production by PBMCs was markedly higher in AS patients than in normal control subjects. These results revealed that IL-23 could induce IL-17 production and that the PBMCs of AS patients most highly responded to the IL-23 stimulation. This study suggest that the up-regulated IL-23 in AS patients may sensitize certain effector cells in PBMCs to produce IL-17 which in turn participates in the development of AS.
In conclusion, our study revealed that the levels of IL-23 and IL-17 in serum and supernatants of PBMCs and the expression of IL-23p19 mRNA in PBMCs are all significantly increased in AS patients. Furthermore, IL-23 enhances the production of IL-17 by PBMCs of AS patients and normal control subjects. These results suggest that upregulated IL-23 and IL-17 production may be responsible for the development of AS. As many other cytokines could influence the production of IL-17, it is necessary to examine the role of other cytokines on the production of IL-17 in AS patients. It is also important to explore the mechanisms of IL-23-induced IL-17 production in AS. All in all, an in-depth understanding of the IL-23/IL-17 pathway may contribute to the study on the pathogenesis and new therapeutic target of AS.
References
Oppmann B, Lesley R, Blom B et al (2000) Novel p19 protein engages IL-12p40 to form a cytokine from a cytokine, IL-23, with biological activities similar as well as distinct from IL-12. Immunity 13:715–725. doi:10.1016/S1074-7613(00)00070-4
Lee E, Trepicchio WL, Oestreicher JL et al (2004) Increased expression of interleukin 23 p19 and p40 in lesional skin of patients with psoriasis vulgaris. J Exp Med 199:125–130. doi:10.1084/jem.20030451
Pirhonen J, Matikainen S, Julkunen I (2002) Regulation of virus-induced IL-12 and IL-23 expression in human macrophages. J Immunol 169:5673–5678
van Seventer JM, Nagai T, van Seventer GA (2002) Interferon-beta differentially regulates expression of the IL-12 family members p35, p40, p19 and EBI3 in activated human dendritic cells. J Neuroimmunol 133:60–71. doi:10.1016/S0165-5728(02)00362-4
Cua DJ, Sherlock J, Chen Y et al (2003) Inerleukin-23 rather than interleukin-12 is the critical cytokine for autoimmune inflammation of the brain. Nature 421:744–748. doi:10.1038/nature01355
Yen D, Cheung J, Scheerens H et al (2006) IL-23 is essential for T cell-mediated colitis and promotes inflammation via IL-17 and IL-6. J Clin Invest 116:1310–1316. doi:10.1172/JCI21404
Lew W, Chang JY, Jung JY et al (2008) Increased expression of interleukin-23 p19 mRNA in erythema nodosum-like lesions of Behcet’s disease. Br J Dermatol 158:505–511. doi:10.1111/j.1365-2133.2007.08403.x
Chabaud M, Durand JM, Buchs N et al (1999) Human interleukin-17: a T cell-derived proinflammatory cytokine produced by the rheumatoid synovium. Arthritis Rheum 42:963–970. doi:10.1002/1529-0131(199905)42:5<963::AID-ANR15>3.0.CO;2-E
Kotake S, Udagawa N, Takahashi N et al (1999) IL-17 in synovial fluids from patients with rheumatoid arthritis is a potent stimulator of osteoclastogenesis. J Clin Invest 103:1345–1352. doi:10.1172/JCI5703
Wong CK, Ho CY, Li EK et al (2000) Elevation of proinflammatory cytokine (IL-18, IL-17, IL-12) and Th2 cytokine (IL-4) concentrations in patients with systemic lupus erythematosus. Lupus 9:589–593. doi:10.1191/096120300678828703
Kurasawa K, Hirose K, Sano H et al (2000) Increased interleukin-17 production in patients with systemic sclerosis. Arthritis Rheum 43:2455–2463. doi:10.1002/1529-0131(200011)43:11<2455::AID-ANR12>3.0.CO;2-K
Teunissen MB, Koomen CW, l Malefyt R et al (1998) Interleukin-17 and interferon-gamma synergize in the enhancement of proinflammatory cytokine production by human keratinocytes. J Invest Dermatol 111:645–649. doi:10.1046/j.1523-1747.1998.00347.x
Lowes MA, Kikuchi T, Fuentes-Duculan J et al (2008) Psoriasis vulgaris lesions contain discrete populations of Th1 and Th17 T cells. J Invest Dermatol 128:1207–1211. doi:10.1038/sj.jid.5701213
Fujino S, Andoh A, Bamba S et al (2003) Increased expression of interleukin 17 in inflammatory bowel disease. Gut 52:65–70. doi:10.1136/gut.52.1.65
McKenzie BS, Kastelein R, Cua DJ (2006) Understanding the IL-23-IL-17 immune pathway. Trends Immunol 27:17–23. doi:10.1016/j.it.2005.10.003
Langrish CL, Chen Y, Blumenschein WM et al (2005) IL-23 drives a pathogenic T cell population that induces autoimmune inflammation. J Exp Med 201:233–240. doi:10.1084/jem.20041257
Murphy CA, Langrish CL, Chen Y et al (2003) Divergent pro- and antiinflammatory roles for IL-23 and IL-12 in joint autoimmune inflammation. J Exp Med 198:1951–1957. doi:10.1084/jem.20030896
Chen Y, Langrish CL, McKenzie BS et al (2006) Anti-IL-23 therapy inhibits multiple inflammatory pathways and ameliorates autoimmune encephalomyelitis. J Clin Invest 116:1317–1326. doi:10.1172/JCI25308
Nakae S, Nambu A, Sudo K, Iwakura Y (2003) Suppression of immune induction of collagen-induced arthritis in IL-17-deficient mice. J Immunol 171:6173–6177
Lubberts E, Koenders MI, Oppers-Walgreen B et al (2004) Treatment with a neutralizing anti-murine interleukin-17 antibody after the onset of collagen-induced arthritis reduces joint inflammation, cartilage destruction, and bone erosion. Arthritis Rheum 50:650–659. doi:10.1002/art.20001
Braun J, Sieper J (2007) Ankylosing spondylitis. Lancet 369:1379–1390. doi:10.1016/S0140-6736(07)60635-7
van der Linden S, Valkenburg HA, Cats A (1984) Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum 27:361–368. doi:10.1002/art.1780270401
Ma XT, Zhang XJ, Zhang B et al (2004) Expression and regulation of interleukin-23 subunits in human peripheral blood mononuclear cells and hematopoietic cell lines in response to various inducers. Cell Biol Int 28:689–697. doi:10.1016/j.cellbi.2004.07.002
Iwakura Y, Ischigame H (2006) The IL-23/IL-17 axis in inflammation. J Clin Invest 116:1218–1222. doi:10.1172/JCI28508
Dong C (2006) Diversification of T-helper-cell lineages: finding the family root of IL-17-producing cells. Nat Rev Immunol 6:329–333. doi:10.1038/nri1807
Kolls JK, Linden A (2004) Interleukin-17 family members and inflammation. Immunity 21:467–476. doi:10.1016/j.immuni.2004.08.018
Aggarwal S, Ghilardi N, Xie MH, de Sauvage FJ, Gurney AL (2003) Interleukin-23 promotes a distinct CD4 T-cell activation state characterized by the production of interleukin-17. J Biol Chem 278:1910–1914. doi:10.1074/jbc.M207577200
Acknowledgments
This work was supported by research grant 30325019 of National Science in China.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, X., Lin, Z., Wei, Q. et al. Expression of IL-23 and IL-17 and effect of IL-23 on IL-17 production in ankylosing spondylitis. Rheumatol Int 29, 1343–1347 (2009). https://doi.org/10.1007/s00296-009-0883-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-009-0883-x