Abstract
Observe pulse electromagnetic fields (PEMFs) effects on ovariectomized (OVX) rats, to study the mechanisms of PEMFs therapy for postmenopausal osteoarthritis. Forty-eight female rats were exposed to PEMFs (PEMFs group), administrated E2 and placebo PEMFs (E group), or were treated with placebo PEMFs (OVX and Sham groups). The treatment duration was 30 days after which serum E2 levels, chondrocyte morphology, chondrocyte apoptosis and matrix metalloproteinases-13 expression in knee joint was analyzed. We observed differential chondrocyte formation in each group, and serum E2 content in the PEMFs and E group were significantly higher than the OVX group. The apoptosis index of chondrocytes and the positive index of MMP13 expression in the PEMFs group and E group were significantly lower than the OVX group. PEMFs has a systemic effect on estrogen metabolism in ovariectomized rats, then inhibit chondrocyte apoptosis and downregulate MMP13 expression of knee joint cartilage. It may be the mechanisms by which PEMFs therapy works for on postmenopausal osteoarthritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most scholars agree that osteoarthritis (OA) is intimately related to estrogen receptor and estrogen (E2) levels [1, 2]. Specifically, some investigators [3, 4] have demonstrated that an ovariectomized (OVX) rat could be used as an experimental animal model of postmanupausal OA. At present, there are no specific effective treatments for OA.
Pulse electromagnetic fields (PEMFs) therapy was developed as a treatment for orthopedic diseases and is a safe, effective physiotherapy for OA [5]. It had been shown that the development of OA was intimately related to chondrocyte apoptosis, inducing cartilage defects [6, 7] and increasing matrix metalloproteinase (MMP) expression, resulting in extracellular matrix (ECM) degradation [8, 9]. However, there have been no studies that analyze the effects of PEMFs on serum E2 levels, chondrocyte apoptosis, and the expression of MMP-13 in the OVX rat model. Therefore, we observed the effects of PEMFs on chondrocyte morphology, apoptosis of medial condyle of femur and tibial plateau chondrocytes, and the expression of MMP-13 of OVX rats in order to determine the therapeutic mechanism of PEMFs for postmenopausal OA.
Materials and methods
Experimental model
Three month old, non-pregnant female SPF Wistar rats (purchased from the experimental animal center of West China Hospital, Sichuan University, certificate number: 0003236) that weighed from 173 to 237 g (190 ± 20 g average) were randomly divided into the following four groups according to random digits tables: PEMFs + OVX group (PEMFs), E2 + OVX group (E), OVX group (OVX), and Sham group (Sham). All rats were subjected to bilateral OVX except the Sham group, and each group included 12 rats.
Reagents and instruments
The following reagents and instruments were used for this study: E2 (premarin or conjugated E2, Favor-clan Hecto- Palace Pharmaceutical Factory, Soochow; Bao Dai Lu No. 4, Soochow, JiangSu, China); Terminal deoxynucleotidyl Transferase Biotin-dUTP Nick End Labeling (TUNEL) kit (Roche, USA); immunohistochemical kit for MMP13 detection (NeoMarkers For Lab Vision Corporation; Astmooor Runcorn, Cheshire WA7 1PR, UK); LEICA RM2125 microtome (Jin Zang Lu No. 258, Pudong Export Processing Zone, Shanghai, China); LEICA DMLS light microscope (Jin Zang Lu No.258, Pudong Export Processing Zone, Shanghai, China); NIKON ECLIPSE E600 fluorescence microscope (Hu Guang Yan Dong Lu No1, Zhan Jiang, Guangdong, China); Union2000 electromagnetic field therapeutic instrument (Academy Institute of Medical Sciences Biomedical Engineering of China; Scientific Research East Lu No. 7, Nakai region, Tianjin, China).
OA model and specimen preparation
Bilateral OVX was performed through a sagittal medial laparotomy under general anesthesia with an intraperitoneal injection of 5% chloraldurat as previously described [3]. In the Sham group, the surrounding fatty tissue of bilateral ovaries was excised. Antibiotic prophylaxis with cefonicid (100 mg/kg) was administered before and for 5 days following surgery. Each group was housed in cages at room temperature (20–26°C), moisture of 60–70%, and under a 12/12 h light/dark cycle with free access to water and rodent food. Each rat was intramuscularly injected with penicillin (400,000 units) to prevent infection once every day for 4 days. The experimental procedures were in compliance with the “Animal Protection Law of the People’s Republic of China (2001)”.
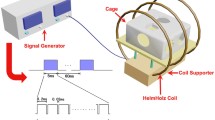
Twelve weeks following the surgery, the PEMFs group rats (whole body) was exposed to pulsed electromagnetic fields with the following specifications: field frequency of 8 Hz; intensity of magnetism of 3.8 mT; 40 min per day for 30 days; and free running. Twelve weeks following surgery, the E group was administered premarin (0.0625 mg/kg per day; intragastric administration 1–2 ml/100 g). Drugs were diluted into suspension with stroke-physiological saline solution. As the same, the E group, OVX group and Sham group rats (whole body) were exposed to placebo PEMFs (identical instrument as PEMFs group but not on switch).
Detection serum E2 levels
After 30 days of intervention, serum from all experimental animals were collected, supernatants were extracted (2 ml), and stored at −20°C. E2 levels were detected using an electrochemiluminescence immunoassay (ECLIA) following the manufacturer’s instructions (Roche, USA).
Tissue preparation and light microscopy
After 30 days, all rats were killed by cervical dislocation. The articular capsule of the knee joint was excised and the medial condyle of femur and tibial plateau cartilage was separated and rinsed with physiological saline. The tissue was further processed for analysis using neutral buffer formalin fixation (40 g/L), disodium ethylenediamine tetraacetic acid decalcification (100 g/L), renoveatur decalcifying fluid on alternate days for 2 weeks, successive ethyl alcohol dehydration, dimethyl benzene transparence, and paraffin imbedding. Several microtome sections (5 μm) were collected from each tissue for morphological observation, apoptosis examination, and MMP13 detection in chondrocytes. The cartilaginous tissue was stained with Hematoxylin and Eosin (H&E) and mounted with neutral balsam to observe chondrocyte morphology by light microscopy.
Chondrocyte apoptosis by TUNEL assay
Chondrocyte apoptosis was measured using the TUNEL assay following manufacturer’s instructions. Briefly, the sections were fixed in dimethyl benzene for 10 min, washed with PBS (three times, 5 min each), incubated in 3% hydrogen peroxide, and washed with PBS (three times, 5 min each). After blotting superfluous fluid on the glass slide with filter paper, the sections were boiled in 0.01 mol/L citrate (pH 6.0) for 10 min then washed with PBS (three times, 5 min each). The tissue sections were incubated in primary antibody (50 μL per section) in a 37°C hygro-cabinet for 1 h after which the sections were washed with PBS (three times, 5 min each). Next, the sections were incubated in secondary antibody (biotinylated goat anti-mouse IgG; 50 μL per section) for 30 min in a 37°C hygro-cabinet, washed with PBS (three times, 5 min each). After incubation with alkaliphosphatase red (A-P red), the sections were washed with distilled water (three times, 2 min each) and counterstained with hematoxylin for 2 min, washed with distilled water (three times, 5 min each)and mounted with gummi. Light microscopy was used to observe positive stained cells which were prunosus in cellular nucleus, karyopycnosis, calculated the apoptosis index (AI), the positive stained cells rate of 300 chondrocytes. Each slide was evaluated by two blinded observers.
MMP13 expression in chondrocytes
Tissue preparation for immunohistochemistry was performed as in the TUNEL analysis. The primary monoclonal antibody for MMP13 (diluted 1:150; 40 μL per section) was incubated in a 4°C hygro-cabinet overnight after which the sections were washed with PBS (three times, 5 min each). The secondary antibody (biotinylated goat anti-mouse IgG; 40 μL per section) was incubated in a 37°C hygro- cabinet for 40 min after which the sections were washed with PBS (three times, 5 min each). HRP-labeled strepto anti-biotin antibodies (diluted 1:100) were incubated with the sections in a 37°C hygro- cabinet for 30 min after which the sections were washed with PBS (three times, 5 min each). Tissue sections were incubated with DAB for 10 min, counterstained with H&E, dehydrated with ethyl alcohol, mounted with DPX. Light microscopy was used to observe positive stained cells which were buffy or dark in cytoplasm, karyopycnosis, calculated the positive index (PI), the positive stained cells rate of 300 chondrocytes. Each slide was evaluated by two blinded observers.
Statistical analysis
Measurement data serum E2 level, AI, and PI are expressed as the mean ± SD. Multitude group comparisons were analyzed by oneway-ANOVA method. Statistics were performed by analysis of variance using the SPSS version 12.0 statistical software (Chicago, IL, USA). Differences between groups were considered significant when P ≤ 0.05.
Results
Comparison of chondrocyte morphology
In the PEMFs and E groups, thinning of the articular cartilage, slight surface asperity, and partial chondrocyte abolition (Figs. 1, 2) were seen. In the OVX group, course articular cartilage surfaces, fibrous degeneration, and fissuring were detected (Fig. 3). The chondrocyte morphology was nearly normal in the Sham group (Fig. 4).
Post-intervention serum E2 levels for all groups
The serum E2 levels in the PEMFs and E groups were statistically higher than in the OVX group (P = 0.002 and P = 0.002, respectively). The serum E2 level in the PEMFs group was not statistically higher than in the E group (P = 0.977). The serum E2 levels of the PEMFs, E, and OVX groups were statistically lower than Sham group (P = 0.002, P = 0.002, and P = 0.000, respectively), demonstrating that PEMFs increase E2 levels in OVX rats (Table 1).
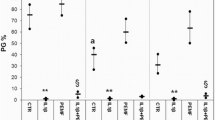
Post-intervention AI of chondrocytes
The nucleus of apoptotic chondrocytes appears buffy. The AI of chondrocytes in the PEMFs group and E group were statistically lower than the OVX group (P = 0.000 < 0.01, P = 0.000 < 0.01). The AI of chondrocytes in the PEMFs group was not statistically lower than the E group (P = 0.160). The AI of chondrocytes in the PEMFs, E, and OVX groups were statistically higher than the Sham group (P = 0.000 < 0.01; P = 0.000 < 0.01; P = 0.000 < 0.01), illustrating that PEMFs and E2 inhibit chondrocyte apoptosis (Table 2; Figs. 5, 6, 7, 8).
Post-intervention PI of MMP13
The nuclei of MMP13-positive chondrocytes appear buffy, and the PI of MMP13 in the PEMF and E groups was statistically lower than in the OVX group (P = 0.000 < 0.01 and P = 0.000 < 0.01, respectively). The PI of MMP13 in the PEMFs group was not statistically lower than in the E group (P = 0.051). The PI of MMP13 in the PEMFs, E, and OVX groups were significantly higher than the Sham group (P = 0.000 < 0.01, P = 0.000 < 0.01, P = 0.000 < 0.01), demonstrating that PEMFs and E2 reduce the expression of MMP13 (Table 3; Figs. 9, 10, 11, 12).
Discussion
The morbitity of OA in the postmenopausal women is higher than in males of similar ages. Women that have low serum E2 levels were more likely to suffer from OA, suggesting that E2 plays an important role in OA. At present, there are no effective treatments for OA. PEMFs have been shown to be safe, effective physiotherapy for OA [5]. Thus, it is important to investigate the mechanisms by which PEMFs affect OA.
Decreasing E2 levels may result in OA and may be related to the estrogen receptor (ER) and gene polymorphisms of ER. Some scholars have verified that both ER-α and ER-β are expressed in articular cartilage, and the expression of ER-α and ER-β proceeds the development of OA. Oshima et al. [10] revealed expression of ER-α and ER-β in the articular cartilage and subchondral bone layers of adult rats of both sexes. High expression of both receptors was also seen in immature rats; in contrast, the expression of ER-α and ER-β decreased in an OVX aged, female rat model, suggesting that there are direct effects of E2 and ER expression on articular surface metabolism. Guofeng et al. [11] used dextran-coated charcoal to quantitively detect ER expression in cartilage cells during the development of OA induced by bilateral OVX in guinea pigs, suggesting that bilateral OVX led to severe OA through reduction in serum E2 levels and downregulation of ER expression in cartilage. Valdes et al. [12] observed that MMP12 gene phenotype was related to image changes in OA of the knee; the progressive traits and OA osteophyte grade were also associated with ER-α. Many investigators have linked ER-α gene polymorphisms with radiographic OA [13–16]. Kang et al. [17] reported that pain susceptibility was associated with ER polymorphisms in temporomandibular joints in female OA patients. Finally, Kinney et al. [18] suggested that human articular chondrocytes exhibit sexual dimorphism in their responses to 17β-estradiol.
Estrogen may affect OA formation through MMP expression. Type II collagen is the primary collagen found in articular cartilage, and Claassen et al. [19] reported that 17β-estradiol promoted type II collagen synthesis as well as other protein such as insulin in articular chondrocytes. Collagen type II degradation products (CTX II) are the characteristic metabolic product of type II collagen in vivo. Because most type II collagen protein is distributed to cartilage, the contents of CTX II in blood and urine may be a special marker of cartilage metabolism. Oestergaard et al. [20] distributed 46 Sprague–Dawley rats into the following treatment groups: OVX, OVX plus early E2 therapy, OVX plus delayed E2 therapy, and sham operation and showed that E2 therapy evoked significant decreases in serum CTX II levels independent of the time. However, delayed initiation resulted in diminished efficacy in terms of preventing cartilage lesions. CTX II fragments were present in articular cartilage, colocalizing with early lesions at the cartilage surface. MMPs are the chief agent responsible for the destruction of collagen and articular cartilage proteins. Lee et al. [21] reported that 17β-estradiol inhibited the expression of MMP1 and MMP13 in chondrocytes. Lu et al. [22] reported that E2 deficiency would result in increased expression of MMP-13, which proceeds OA. After 3 months, we found the E2 content was significantly lower in OVX animals as compared to the Sham group (P < 0.01, Table 1) and MMP 13 expression was significantly higher in OVX animals as compared to the Sham group (Table 3, Figs. 9, 10, 11, 12), resulting in increased catabolism of type II collagen accompanied by loss of cartilage matrix (Figs. 1, 2, 3, 4).
The effects of E2 on articular cartilage are dose–responsive; most investigators presumed that low dose E2 reduces inflammatory factor-induced cartilage degradation while high dose E2 promotes cartilage cataplasia. Richette et al. [23] verified the effect of 17β-estradiol on interleukin-1β (IL-1β)-induced proteoglycan degradation, showing that low concentrations (0.1 nM) of E2 counteracts the IL-1β-induced decrease in sulphated PG, while high concentrations (10 nM) of E2 enhances the IL-1β effects. Song et al. [24] reported an increase in expression of MMP-1 mRNA, MMP-3 mRNA, and IL-1β in OA synovial tissue from OVX rabbits. E2 supplementation decreased MMP and IL-1β expression, which was further enhanced by progestin. Low dose E2 could decrease the ratio of MMP-1/TIMP-1 and MMP3/TIMP1, which could further decreased by progestin; high dose E2 could slightly increase the ratio, but remained lower than the untreated control group. The investigators suggested that certain doses of E2 and the appropriate E2 and progestin ratio are crucial for normal articular cartilage, and E2 deficiency or excess damages articular cartilage. Rong et al. [25] found that E2 modulates collagen expression and MMP mRNA expression in articular cartilage chondrocytes; E2 concentrations lower than the physiological level (10−12 mol/L) can delay the degradation of articular cartilage. For degenerative chondrocytes, concentrations lower than the physiological level was appropriate for the maintenance of the collagen epitope of articular cartilage.
Chagin et al. [26] discovered endogenous estradiol-induced proliferation and apoptosis of a human chondrocyte-like cell line, HCS-2/8 cells. The aromatase inhibitor, letrozole, and the pure ER antagonist, ICI 182,780, inhibited the differentiation of chondrocytes, and admoveatur caspase-3 or pan-caspase inhibitors completely blocked ICI 182,780-induced apoptosis.
The results of our investigation showed that chondrocytes of the femoral head underwent pathological changes in OVX rats. After intervention with premarin, the chondrocyte lesions were significantly reduced as compared to the OVX group (Figs. 1, 2, 3, 4). Thus, we support the view that low level E2 is associated with the development of OA. In addition, apoptosis of chondrocytes was significantly higher in the E group than the Sham group (P < 0.01) but was significantly lower than in OVX group (P < 0.01, Table 2; Figs. 5, 6, 7, 8). We presume that E2 inhibits chondrocyte apoptosis, delaying the development of OA. Whether the effects of premarin on articular cartilage presents a dose–responsive relationship needs to be furthered studied.
The therapeutic effects of PEMFs on osteoarthritis [27–30] have been documented; PEMFs can relief pain, the primary clinical symptom of OA, in a relatively short time and improve joint disfunction. Wolsko et al. [31] reported that the mechanism by which PEMFs relieves or eliminates pain is mediated by a Ca2+ ion channel. At the same time, Del Seppia et al. [32] determined that one potential mechanism of PEMFs was associated with increased serumβ2-endorphin. Furthermore, oxygen free radicals as a etiological factor for impaired articular cartilage that proceeds of OA has been determined; Beecher et al. [33] found that impairing an antioxidant agent, superoxide dismutase (SOD) induced chondrocytes apoptosis. In addition, Kurz et al. [34] found SOD diminished pressure-induced chondrocyte apoptosis. De Nicola et al. [35] reported that an electromagnetic field augmented reactive oxygen species, depleted glutathione, and decreased chondrocyte apoptosis.
In this experimental study, exposure of OVX rats to PEMFs for 30 days increased serum E2 levels compared to the control group (P < 0.01, Table 1), decreased chondrocyte apoptosis induced by low E2 (Table 2, Figs. 5, 6, 7, 8), exhibiting the same effect as the control group that received E2 intervention. This demonstrates that PEMFs enhanced serum E2 levels in OVX rats, improved chondrocyte cataplasia induced by decreased E2, repressed the apoptosis of chondrocytes, and possess the E2-like effects.
Metal ions are necessary for enzymatic activity; magnetic fields are thus able to influence the catalytic activity of enzymes that use metal ions as a cofactor. Consequently, PEMFs can regulate the enzymatic activity of MMPs, which degrade extracellular matrix. In fact, MMP13 demolishes extracellular matrix, so to a certain extent, reduced expression of MMP13 in articular chondrocytes would prevent and cure OA. Ciombor et al. [36] exposed 12 month old Hartley guinea pigs, which spontaneously develop arthritis that bears morphological, biochemical, and immunohistochemical similarities to human OA, to PEMFs for 1 h/day for 6 months. PEMFs treatment preserved the morphology of articular cartilage, retarded the development of OA lesions, suppressed MMP13 and MMP3 expression, upregulated gene expression of TGF-β, and downregulated MMP and IL-1 activity. Furthermore, PEMFs favorably affected cartilage homeostasis mediated by the stimulation of TGF-β. In the study, we determined that exposure of OVX rats to PEMFs for 30 days could decrease the expression of MMP13 in chondrocytes compared to the OVX group (P < 0.01, Table 3, Figs. 9, 10, 11, 12), in a similar manner as the E group, demonstrating that PEMFs protect articular cartilage by influencing MMP13 expression.
The morbidity of OA is related to endocrine secretions, such as E2 levels, as well as inflammatory factors. The human body is hypersensitive to electromagnetic field; organs accept PEMFs stimulation, which thereby affects the hypothalamic-hypophysis-adrenal systems as well as the immune system [37, 38]. Reyes-Guerrero et al. [39] presumed that extremely low-frequency electromagnetic fields retain social recognition memory in female rats similar 17β-estradiol. In this study, we found that OVX rats that were treated with PEMFs for 30 days could increase the level of E2 (P < 0.01) to similar levels as the E group (Table 1, Fig. 1). In addition, PEMFs protected the chondrocytes of the femoral head, reducing chondrocyte apoptosis, repressed the expression of MMPs in OVX rats compared to the OVX control group (P < 0.01), in a similar manner to the E group (Tables 2, 3; Figs. 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12).
In conclusion, low E2 levels result in the apoptosis of chondrocytes and the expression of MMP13; PEMFs can significantly enhance the level of serum E2 in OVX rats and inhibit the apoptosis of chondrocytes, downregulate the expression of MMP13 as well as administration estrogen in OVX rats. Therefore, on the basis of the predecessors’ investigations, our methods and results, we consider PEMFs has a systemic effect on estrogen metabolism in OVX rats. PEMFs can prevent and cure the knee osteoarthritis resulting from estrogen decrease. Because the knee OA is a common OA in clinic as well as hip and lumbar vertebra OA, we selected the cartilage in knee joint to study. Meanwhile, we presumed that PEMFs can impact on others articular cartilage and we will further study to verify the viewpoint. We suggest that the effects of PEMFs on chondrocytes and extracellular matrix is by the pathway of systemic effect on estrogen metabolism in ovariectomized rats.
Whether different intensities and frequencies of PEMFs will have different effects on E2 levels, chondrocyte apoptosis, and MMP13 expression needs to be further investigated.
References
Kalichman L, Kobyliansky E (2007) Age, body composition, and reproductive indices as predictors of radiographic hand osteoarthritis in Chuvashian women. Scand J Rheumatol 36:53–57. doi:10.1080/03009740600902460
Cooley HM, Stankovich J, Jones G (2003) The association between hormonal and reproductive factors and hand osteoarthritis. Maturitas 45:257–265. doi:10.1016/S0378-5122(03)00151-8
Hoegh-Andersen P, Tanko LB, Andersen TL et al (2004) Ovariectomized rats as a model of postmenopausal osteoarthritis: validation and application. Arthritis Res Ther 6:R169–R180. doi:10.1186/ar1152
Dai G, Wang S, Li J et al (2006) The validity of osteoarthritis model induced by bilateral ovariectomy in guinea pig. J Huazhong Univ Sci Technolog Med Sci 26:716–719. doi:10.1007/s11596-006-0624-2
Sharma L (2002) Nonpharmacologic management of osteoarthritis. Curr Opin Rheumatol 14:603–607. doi:10.1097/00002281-200209000-00022
John T, Muller RD, Oberholzer A et al (2007) Interleukin-10 modulates pro-apoptotic effects of TNF-ain human articular chondrocytes in vitro. Cytokine 40:226–234. doi:10.1016/j.cyto.2007.10.002
Kim HA, Blanco FJ (2007) Cell death and apoptosis in ostearthritic cartilage. Curr Drug Targets 8:333–345. doi:10.2174/138945007779940025
Morquette B, Shi Q, Lavigne P et al (2006) Production of lipid peroxidation products in osteoarthritic tissues—new evidence linking 4-hydroxynonenal to cartilage degradation. Arthritis Rheum 54:271–281. doi:10.1002/art.21559
Manacu CA, Martel-Pelletier J, Roy-Beaudry M et al (2005) Endothelin-1 in osteoarthritic chondrocytes triggers nitric oxide production and upregulates collagenase production. Arthritis Res Ther 7:R324–R332. doi:10.1186/ar1489
Oshima Y, Matsuda K, Yoshida A et al (2007) Localization of estrogen receptors alpha and beta in the articular surface of the rat femur. Acta Histochem Cytochem 40:27–34. doi:10.1267/ahc.06015
Dai G, Li J, Liu X et al (2005) The relationship of the expression of estrogen receptor in cartilage cell and osteoarthritis induced by bilateral ovariectomy in guinea pig. J Huazhong Univ Sci Technolog Med Sci 25:683–686
Valdes AM, Hart DJ, Jones KA et al (2004) Association study of candidate genes for the prevalence and progression of knee osteoarthritis. Arthritis Rheum 50:2497–2507. doi:10.1002/art.20443
Bergink AP, van Meurs JB, Loughlin J et al (2003) Estrogen receptor alpha gene haplotype is associated with radiographic osteoarthritis of the knee in elderly men and women. Arthritis Rheum 48:1913–1922. doi:10.1002/art.11046
Lian K, Lui L, Zmuda JM et al (2007) Estrogen receptor alpha genotype is associated with a reduced prevalence of radiographic hip osteoarthritis in elderly Caucasian women. Osteoarthr Cartil 15:972–978. doi:10.1016/j.joca.2007.02.020
Jin SY, Hong SJ, Yang HI et al (2004) Estrogen receptor alpha gene haplo type is associated with primary knee osteoarthritis in Korean population. Arthritis Res Ther 6:R415–R421. doi:10.1186/ar1207
Fytili P, Giannatou E, Papanikolaou V et al (2005) Association of repeat polymorphisms in the estrogen receptors alpha, beta, and androgen receptor genes with knee osteoarthritis. Clin Genet 68:268–277. doi:10.1111/j.1399-0004.2005.00495.x
Kang SC, Lee DG, Choi JH et al (2007) Association between estrogen receptor polymorphism and pain susceptibility in female temporomandibular joint osteoarthritis patients. Int J Oral Maxillofac Surg 36:391–394. doi:10.1016/j.ijom.2006.12.004
Kinney RC, Schwartz Z, Week K et al (2005) Human articular chondrocytes exhibit sexual dimorphism in their responses to 17 beta-estradiol. Osteoarthr Cartil 13:330–337. doi:10.1016/j.joca.2004.12.003
Claassen H, Schluter M, Schunke M et al (2006) Influence of 17 beta-estradiol and insulin on type II collagen and protein synthesis of articular chondrocytes. Bone 39:310–317. doi:10.1016/j.bone.2006.02.067
Oestergaard S, Sondergaard BC, Hoegh-Andersen P et al (2006) Effects of ovariectomy and estrogen therapy on type II collagen degradation and structural integrity of articular cartilage in rats: implications of the time of initiation. Arthritis Rheum 54:2441–2451. doi:10.1002/art.22009
Lee YJ, Lee EB, Kwon YE et al (2003) Effect of estrogen on the expression of matrix metalloproteinase (MMP)1, MMP3, and MMP13 and tissue inhibitor of metalloproternase1 in osteoarthritis chondrocytes. Rheumatol Int 23:282–288. doi:10.1007/s00296-003-0312-5
Lu T, Achari Y, Sciore P et al (2006) Estrogen receptor alpha regulates matrix metalloproteinase-13 promoter activity primarily through the AP-1 transcriptional regulatory site. Biochim Biophys Acta 1762:719–731
Richette P, Dumontier MF, Francois M et al (2004) Dual effects of 17beta oestradiol on interleukin 1 beta induced proteoglycan degradation in chondrocytes. Ann Rheum Dis 63:191–199. doi:10.1136/ard.2003.006510
Song YJ, Wu ZH, Lin SQ et al (2003) The effect of estrogen and progestin on the expression of matrix metalloproteinases, tissue inhibitor of metalloproteinase and interleukin-1β mRNA in synovia of OA rabbit model. Zhonghua Yi Xue Za Zhi 83:498–503
Wan R, Yang Q, Deng L et al (2005) Effect of estrogen on collagen epitope expression of chondrocytes. Chin J Sports Med 24:187–190. doi:10.1016/j.csm.2004.08.005
Chagin AS, Chrysis D, Takigawa M et al (2006) Locally produced estrogen promotes fetal rat metatarsal bone growth; an effect mediated through increased chondrocyte proliferation and decreased apoptosis. J Endocrinol 188:193–203. doi:10.1677/joe.1.06364
Fischer G, Pelka RB, Barovic J (2005) Adjuvant treatment of osteoarthritis of the knee with weak pulsing magnetic fields. Results of a prospective, placebo controlled trial. Z Orthop Ihre Grenzgeb 143:544–550. doi:10.1055/s-2005-836830
Sutbeyaz ST, Sezer N, Koseoglu BF (2006) The effect of pulsed electromagnetic fields in the treatment of cervical osteoarthritis: a randomized, double-blind, sham-controlled trial. Rheumatol Int 26:320–324. doi:10.1007/s00296-005-0600-3
Nicolakis P, Kollmitzer J, Crevenna R et al (2002) Pulsed magnetic field therapy for osteoarthritis of the knee—a double-blind sham-controlled trial. Wien Klin Wochenschr 114:678–684
Battisti E, Piazza E, Rigato M (2004) Efficacy and safety of a musically modulated electromagnetic field (TAMMEF) in patients affected by knee osteoarthritis. Clin Exp Rheumatol 22:568–572
Wolsko PM, Eisenberg DM, Simon LS et al (2004) Double-blind placebo-controlled trial of static magnets for the treatment of osteoarthritis of the knee: results of a pilot study. Altern Ther Health Med 10:36–43
Del Seppia C, Ghione S, Luschi P et al (2007) Pain perception and electromagnetic fields. Neurosci Biobehav Rev 31:619–642. doi:10.1016/j.neubiorev.2007.01.003
Beecher BR, Martin JA, Pedersen DR et al (2007) Antioxidants block cyclic loading induced chondrocyte death. Iowa Orthop J 27:1–8
Kurz B, Lemke A, Kehn M et al (2004) Influence of tissue maturation and antioxidants on the apoptotic response of articular cartilage after injurious compression. Arthritis Rheum 50:123–130. doi:10.1002/art.11438
De Nicola M, Cordisco S, Cerella C et al (2006) Magnetic fields protect from apoptosis via redox alteration. Ann N Y Acad Sci 1090:59–68. doi:10.1196/annals.1378.006
Ciombor DM, Aaron RK, Wang S et al (2003) Modification of osteoarthritis by pulsed electromagnetic field—a morphological study. Osteoarthr Cartil 11:455–462. doi:10.1016/S1063-4584(03)00083-9
Marino AA, Wolcott RM, Chervenak R et al (2001) Coincident nonlinear changes in the endocrine and immune systems due to low-frequency magnetic fields. Neuroimmunomodulation 9:65–77. doi:10.1159/000049009
Izmest’eva OS, Parshkov EM, Zhavoronkov LP et al (2003) Effects of electromagnetic field of thermal intensity on the hypophysis-thyroid unit of the neuroendocrine system. Radiats Biol Radioecol 43:597–600
Reyes-Guerrero G, Vazquez-Garcia M, Elias-Vinas D et al (2006) Effects of 17 b-estradiol and extremely low-frequency electromagnetic fields on social recognition memory in female rats: A possible interaction? Brain Res 1095:131–138. doi:10.1016/j.brainres.2006.04.020
Acknowledgments
The authors thank Zhen-Mei An, Ph.D. for technical assistance with the serum E2 assay. We would also like to thank Yin-Ling Deng for help with the TUNEL assay. We thank the National Natural Science Fund for the financial support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Luo, Q., Li, SS., He, C. et al. Pulse electromagnetic fields effects on serum E2 levels, chondrocyte apoptosis, and matrix metalloproteinase-13 expression in ovariectomized rats. Rheumatol Int 29, 927–935 (2009). https://doi.org/10.1007/s00296-008-0782-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-008-0782-6