Abstract
The aim of this study is to evaluate the effect of submaximal aerobic exercise program on postural balance in postmenopausal women with osteoporosis. Twenty-five postmenopausal women without osteoporosis and 28 postmenopausal women with osteoporosis enrolled in this study. Balance ability of all subjects was measured by timed up and go test (TUG), four square step test (FSS), Berg balance scale (BBS) and Kinesthetic ability trainer 3000. After completion of initial measurements of balance, postmenopausal women with osteoporosis attended the submaximal aerobic exercise program on treadmill. At the end of the exercise program, balance tests were repeated. Balance tests of postmenopausal women without osteoporosis were repeated approximately 4-weeks after the initial measurement. There was statistically significant improvement in all balance scores in the postmenopausal women with osteoporosis after exercise training whereas there were no statistically significant differences in the scores of postmenopausal women without osteoporosis who did not exercise. This study showed that a 4-week submaximal aerobic exercise program provided significant improvements in static and dynamic balances in postmenopausal osteoporotic women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is an important health problem in aging population, showing itself as fractures even after minor trauma. These fractures can affect any bone in the body; wrist, femur neck and vertebra are the most frequently influenced sites [1].
Falls are recognized as the most important risk factor that increases the tendency to osteoporotic fractures that have a high rate of morbidity and mortality [1]. The causes of falls are multi-factorial. Among most commonly reported risk factors are gait and balance disorders [2]. One-fourth of the falls result in serious injuries, even falls without complications May also lead to decrease in self-confidence and quality of life [1, 3].
Frequency of falls in middle–late age groups is higher in women than in men [4]. Increased tendency to fall in elderly persons is related to decreased postural stability and is believed to be a result of impaired general health status [1]. Decreased postural stability is also observed in postmenopausal period. Fall incidence is three times higher in postmenopausal women than in men within the same age group. Estrogen withdrawal in menopause is suggested to affect postural stability via reducing the speed of information processing of the brain [5].
Regular weight bearing exercises have great benefits on bone mineral density. Walking, which is an easy and safe form of weight bearing exercise that does not require any special equipment, also improves muscle strength, balance, coordination, proprioception and reaction time; and eventually improving postural balance; exercise might contribute to reduce incidence of falls [6].
Aim of this study is to investigate the effects of 4-week aerobic exercise program on postural balance in postmenopausal women with osteoporosis.
Methods
Subjects
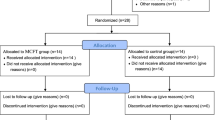
Subjects were recruited from volunteered patients who were admitted to physical medicine and rehabilitation outpatient clinic in Gazi University Hospital. This study was performed according to the Helsinki Declaration. Subjects with musculoskeletal disorders such as arthritis, amputations; neurologic disorders such as peripheric neuropathy; visual and vestibular disorders were not included. Fifty-three postmenopausal women participated in the study and all subjects were classified into two groups according to their bone mineral density. Group 1 consisted of postmenopausal women with osteoporosis (n = 28), group 2 consisted of postmenopausal women without osteoporosis (n = 25). Demographic information, systemic diseases, medications used and risk factors for falling were recorded. Musculoskeletal and neurologic examinations of each subject were performed. Mini mental state examination (MMSE) test and hospital anxiety and depression test were used for the evaluation of cognitive function and mood status, respectively.
Procedure
Balance ability of all subjects was measured by static and dynamic functional balance tests. Timed up and go test (TUG), four square step test (FSS) and Berg balance scale (BBS) were used to assess dynamic and functional balance.
In TUG, subjects were seated on a back-supported chair. Then they were asked to stand up from chair, walk (through a 3 m path specified on the floor) 3 m away from the chair (which is marked on the floor), turn, walk back to chair and sit down. Time taken to complete the test was measured in seconds [7].
For FSS, four squares were formed by four canes placed flat on the floor. The subject was asked to stand in one of the squares (number 1) facing the adjacent square (number 2). The subsequent squares were numbered as 3 and 4. The subject was then asked to step into the squares in a given order (2-3-4-1-4-3-2-1) as quickly as possible and without touching the canes. In each square, contact of both feet was required. In order to familiarize with the test, one practice trial was allowed after explaining and showing the test to the subject. If the subject failed to complete the sequence in the correct way, failed to protect her balance and had contact with any of the canes on the floor, the test procedure was repeated. Time taken to complete the given sequence was recorded in seconds. Timing began when the first foot made contact with the floor of the second square and ended when the last foot had contact with the floor of the first square [8].
BBS was used to assess functional balance. The test consists of 14 items that are frequently performed in activities of daily living. The subjects were asked to perform the items in an order of increasing difficulty of the tasks. Tasks consisted of more stable positions like standing and sitting without support, sitting from standing and standing from sitting and picking up an object from the floor. The most difficult items were single leg stance and tandem stance that required maintenance of balance on reduced base of support. Scores in BBS were scaled from 0, failure to perform task, to 4, ability to perform task independently and safely [9].
Kinesthetic ability trainer 3000 (KAT 3000, Kinesthetic Ability Trainer 3000) (Med-Fit Systems Inc., Fallbrook, CA, USA) was used for quantitative assessment of static balance. In static balance test, subjects were asked to stand on the balance platform. Optimum position was obtained using the x and y-axis drawn perpendicular to each other on the platform. Subjects were instructed to put their feet on the center of the platform with the second toe coming over the line parallel to y-axis and the highest point of the long arch crossing the x-axis. The platform is freely movable so that the subject can maintain her balance by tilting it back and forth and from side to side without moving her feet, but instead changing her center of gravity by trunk movements. For the static balance test, subject was asked to maintain her equilibrium as motionless as possible on the platform for 30 s. During the procedure, for assistance, the subject kept red ‘X’ sign that represented center of the platform on the center of the computer screen, as visual feedback. For familiarization, practice on the platform for 1 min was allowed. Subject was asked to hold her arms across her chest during the tests. Three subsequent tests were performed and the best balance score obtained was recorded for analyses.
Exercise training
After completion of initial measurements of balance, postmenopausal women with osteoporosis attended the submaximal aerobic exercise program on treadmill, lasting for 30 min, twice a week for 4 weeks. Maximal exercise tolerance test (Bruce protocol) was performed on the preceding day of the exercise program. Maximum heart rate is calculated by the formula (220 − age). the submaximal aerobic exercise training was prescribed as 60–85 of maximum heart rate. On the day after the end of the exercise program, exercise tolerance test and balance tests were repeated. Balance tests were performed before the exercise tolerance test to avoid the negative effects of fatigue on postural balance.
Postmenopausal women without osteoporosis did not attend the exercise classes. Balance tests of postmenopausal women without osteoporosis were repeated approximately 4 weeks after the initial measurement to determine whether there were any practice effects of the testing procedures.
Statistics
Statistical analyses were performed using SPSS 10.0 for Windows Package Program. Balance scores of two groups were recorded as mean and standard deviation. Mann Whitney-U test was used for comparison of balance scores among groups. Chi-square test was used for comparing the nominal variables among groups. Pearson correlation test was used to assess the relationships between balance scores and age. Wilcoxon test was used to compare the balance scores measured before and after exercise program. Statistical significance was established at the “P < 0.05” level.
Results
Mean age of 53 women was 55 (43–73) years. Mean, minimum and maximum values of age, height, weight and body mass indices of two groups are shown in Table 1.
Frequencies of other risk factors that might affect balance were not significantly different among the two groups; fall history within the previous year (17.9 and 20.0%, P > 0.05, χ² = 0.04), use of antidepressants (7.1 and 12.0%, P > 0.05, χ² = 0.4) and antihypertensives (25.0 and 36.0%, P > 0.05, χ² = 0.8).
Scores of anxiety, depression and MMSE were similar among the groups (anxiety scores were 7.5 ± 2.3, 7.0 ± 2.9; depression scores were 6.1 ± 2.6, 7.0 ± 2.4; MMSE scores were 28.6 ± 2.4, 28.2 ± 1.2 for groups 1 and 2, respectively, P > 0.05).
Table 2 shows the balance scores obtained from balance test on KAT and other functional balance tests (TUG, FSS, and BBS). There was no statistically significant difference in balance scores among the groups (P > 0.05).
There was a significant correlation between age and all balance scores (P < 0.001 and r = −0.63 with BBS; P < 0.05 and r = 0.35 with KAT; P < 0.05 and r = 0.42 with TUG; P < 0.05 and r = 0.33 with FSS).
Twenty-six postmenopausal women in the study group completed the exercise program lasting for 4 weeks. One subject failed to complete the program because of musculoskeletal injury and the other never attended without providing any excuse. Table 3 demonstrates the initial and final balance scores in the postmenopausal women. Duration of exercise tolerance test was significantly increased after exercise program (6.9 ± 1.8 vs. 9.1 ± 1.7 min, P < 0.001). There was statistically significant improvement in all balance scores in the study group after the completion of the 4-week aerobic exercise program, whereas no statistically significant differences were noted in the control group.
Discussion
We found that low bone mineral density did not modify the balance and a 4-week submaximal aerobic exercise program significantly improved the static and dynamic balances in postmenopausal women with osteoporosis.
Incidence of falls increases with advancing age. Most of the elderly persons who fall, experience complications like fractures, soft tissue injuries, limited mobility and fear of falling, all of which affect independence and quality of life [1]. Prevention programs for falls require identifying the risk factors of falls. Falls are related to numerous risk factors and fall risk is directly proportional to the number of the risk factors present.
Postural imbalance is a major risk factor for falls. Nguyen et al. [10] found that bone mineral density, postural sway and quadriceps strength were the important indicators of falls. Lord et al. [11] showed that eyes closed postural sway, reaction time, lower limb proprioception and strength of ankle dorsiflexors were significantly different between multiple fallers and nonfallers. Wolfson et al. [13] reported that the decline in balance ability in the elderly was most probably related to loss of strength in lower extremity and decline in sensorimotor functions. Our study also confirmed that advanced age is an important factor for impairment of balance. Women are more prone to falls than men. Although there is no gender difference for falls in advanced age, the incidence of falls is higher in middle–late aged women when compared to men of the same age [4]. Crilly et al. [4] reported that fall incidence starts increasing during menopause and this increase may be related to the effects of hormonal changes on postural stability. Another study also showed that the fall risk increased during perimenopausal period [14]. Nitz et al. [15] investigated the mediolateral balance changes in women aged between 40 and 80 years and found that there was a significant decline in mediolateral balance ability in ages of 40–60 years, which correspond to menopausal period. Estrogen withdrawal after menopause leads to slowing of speed of information processing in brain. This change is especially important for postural stability which depends on identifying sensory input and initiating appropriate physical response [5]. It is believed that hormon replacement therapy (HRT) might modify the changes observed in muscle mass and strength during the perimenopausal period [16, 17]. Naessen et al. [18] showed that postmenopausal women who were taking estrogen pills for long periods had better postural balance than women who were not. This effect of estrogen on postural balance is most probably related to the effects on neuronal transmission in central nervous system. Besides central effects, long-term estrogen replacement therapy protects elements of connective tissue and muscle strength, upgrades quality of life and emotional state of women and these effects are believed to ameliorate postural balance function indirectly [19]. Therefore, in this study we assessed women in postmenopausal period in whom the fall risk tends to increase.
It is a well-known fact that inactivity is a disrupting factor for postural control. Many studies reported that physical activities and sports improved postural performance [20, 21]. Aging and sedentary life cause diminution of muscle mass (sarkopenia) and strength. Sports and being physically active might prevent or delay these changes. Increased physical activity is related to better muscle strength, reaction time, balance and coordination and all these help to prevent falls and fall-related fractures [22]. Perrin et al. [21] found that physically active elderly persons had better postural control than inactive peers. Since it was shown that balance ability was not different in individuals who started sportive activities later in life and in individuals who never gave up sports, it is essential to prescribe physical activity to elderly persons who were previously sedentary [21]. Physically active individuals regulate somatosensory inputs more efficiently and this leads to better balance control. Proprioception and sensory inputs originating from plantar surface of the foot are important systems for maintenance of balance. Physical activity provides more effective postural adaptation via increasing susceptibility to these stimuli [21].
A variety of exercise programs are developed to improve balance and prevent fall risk in elderly persons with osteoporosis. Exercise can decrease the risk of fracture in osteoporotic individuals by protecting bone mineral density and more importantly by decreasing the fall risk via improvement in postural stability [23]. Studies also showed that exercise might ameliorate the risk factors for balance impairment and falls, although type, intensity, frequency and duration of exercise are not uniform in these studies. Heinonen et al. [24] reported that plyometric exercise programs (jumping, step, etc.) for 18 months increased bone mineral density of lower extremity and axial skeleton that was bearing weight and also improved the muscle strength and dynamic balance in premenopausal women. High-velocity movements in plyometric exercises are believed to increase the speed of body movements and reflex time and hence improve balance, coordination, reaction time, motor skills and muscle strength.
Shaw and Snow [25] found that weight bearing resistive exercises lasting for 9 months significantly increased muscle strength of lower extremity and lateral stability in postmenopausal women aged 50–75 years. Lord et al. [26] also showed that a 12 month-exercise program consisting of strengthening, balance and coordination exercises improved quadriceps muscle strength and postural sway in elderly women.
The effects of aerobic exercise on balance and prevention of falls are intensely investigated in postmenopausal elderly women. Shigematsu et al. [27] reported that a 3 month-aerobic exercise program of dancing improved balance and mobility in elderly women. We supported these reports and showed that even a short duration submaximal aerobic exercise (4 weeks, twice a week) program significantly improved static and dynamic balances in postmenopausal women.
The duration of the exercise training programs aiming at decreasing the propensity for falling in the elderly women seems to be at least 3 months or longer. Carter et al. [23] showed that an exercise program lasting for 20 weeks, aiming to develop posture, gait, balance, coordination, hip and trunk stabilization in osteoporotic women improved the strength of knee extension, which is an independent factor of dynamic balance and falls. However, in another study by the same authors 10-weeks exercise program did not significantly modify the strength of knee extension, and the static and dynamic balances in osteoporotic women and it was stressed that the length of the exercise program might be insufficient to change the fall-risk profile in women with osteoporosis [28]. On the other hand, Mills [29] showed that 8 week-duration low intensity aerobic exercise improved the balance by 22% in the elderly. Incongruous results obtained from different studies might possibly arise from the differences of the type, duration, intensity and frequency of the exercises. Our study showed that the relatively short duration aerobic exercise (4 weeks, twice a week) program significantly improved balance scores in postmenopausal women when compared with the control group. Nevertheless, this improvement in balance function does not warrant prevention of falls. The effects of exercise on falls and fractures should be investigated prospectively to make an accurate conclusion. Length of our study is very short to make an interpretation about effects of exercise on falls, so studies with longer periods are needed. On the other hand, persistence of improvements in balance ability can be maintained by exercise regularity. Exercise should be a part of life in postmenopausal women to prevent falls and fall related fractures.
Most of the studies on balance and falls analyze elderly persons at high risk [3, 11, 12, 20, 22, 26, 27, 29]. However, not only physically dependent subjects, but also independent individuals need to be protected from falls and maintain their functional abilities. Independent individuals will also experience decline in physical capabilities and functions as their age advances, so the target population of rehabilitation should also be individuals at younger age group. We also studied women who were younger (mean age: 56 years) and functionally more capable (mean Berg balance score: 53.8) compared to other studies. As significant improvement in balance and functions is observed after exercise in younger and functionally independent women, exercise should be an important part of management strategies aiming to improve balance and prevent falls and hence, fractures in this age group.
In conclusion, this study shows that the balance abilities of postmenopausal women with osteoporosis were not different from that of postmenopausal women without osteoporosis, in other words osteoporosis did not modify balance. Balance proved to be correlated with age considering all the subjects in two groups. A 4 week-submaximal aerobic exercise training program provided significant improvements in static and dynamic balances in our postmenopausal osteoporotic women.
References
Lord SR, Sambrook PN, Gilbert C, Kelly PJ, Nguyen T, Webster IW, Eisman JA (1994) Postural stability, falls and fractures in the elderly: results from Dubbo osteoporosis epidemiology study. Med J Aust 160:684–691
Shumway-Cook A, Baldwin M, Polissar NL, Gruber W (1997) Predicting the probability for falls in community-dwelling older adults. Phys Ther 77:812–819
Blake AJ, Morgan K, Bendalll MJ (1998) Falls by elderly people at home: prevelance and associated factors. Age Ageing 17:365–372
Crilly RG, Richardson LD, Roth JH, Vandervoort AA, Hayes KC, Mackenzie RA (1987) Postural stability and colles’ fracture. Age Ageing 16:133–138
Shepherd JE (2001) Effects of estrogen on cognition, mood, and degenerative brain diseases. J Am Pharm Assoc 41:221–228
Kannus P (1999) Preventing osteoporosis, falls and fractures among elderly people. BMJ 318:205–206
Shumway-Cook A, Brauer S, Woolacott M (2000) Predicting the probability for falls in community-dwelling older adults using the timed up and go test. Phys Ther 80:896–903
Dite W, Temple VA (2002) A clinical test of stepping and change of direction to identify multiple falling older adults. Arch Phys Med Rehabil 83:1566–1571
Berg KO, Maki BE, Williams JI, Holliday PJ, Wood-Dauphinee SL (1992) Clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil 73:1073–1080
Nguyen T, Sambrook P, Kelly P, Jones G, Lord S, Freund J, Eisman J (1993) Prediction of osteoporotic fractures by postural instability and bone density. BMJ 307(6912):1111–1115
Lord SR, Clark RD, Webster IW (1991) Physiological factors associated with falls in an elderly population. JAGS 39:1194–1200
Wolfson L, Whipple R, Derby CA, Amerman P, Murphy T, Tobin JN, Nashner L (1992) A dynamic posturography study of balance in healthy elderly. Neurology 42:2069–2075
Winner S, Morgan C, Evans J (1989) Perimenopausal risk of falling and incidence of distal forearm fracture. BMJ 298:1486–1488
Nitz JC, Choy NL, Isles RC (2003) Medial-lateral postural stability in community-dwelling women over 40 years of age. Clin Rehabil 17:765–767
Brooke-Wawel K, Prelevic GM, Bakridan C, Ginsburg J (2001) Effects of physical activity and menopausal hormone replacement therapy on postural stability in postmenopausal women: a cross-sectional study. Maturitas 37(3):167–172
Preisinger E, Alacamlioglu Y, Saradeth T, Resch KL, Holzer G, Metka M (1995) Forearm bone density and grip strength in women after menopause, with and without estrogen replacement therapy. Maturitas 21:57–63
Naessen T, Lindmark B, Larsen HC (1997) Better postural balance in elderly women receiving estrogens. Am J Obstet Gynecol 177(2):412–416
Philips SK, Rook KM, Siddle NC, Bruce SA, Woledge RC (1992) Muscle weakness in women occurs at an earlier age than in men, but strength is preserved by hormone replacement therapy. Clin Sci 84:95–98
Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM (1997) Randomised controlled trial of a general practice program of home based exercise to prevent falls in elderly women. BMJ 315:1065–1069
Perrin PP, Gauchard GC, Perrot C, Jeandel C (1999) Effects of physical and sporting activities on balance control in elderly people. Br J Sports Med 33:121–126
Myers AH, Yong Y, Langlois JA (1996) Prevention of falls in the elderly. Bone 18:87–102
Carter ND, Khan KM, McKay HA, Petit MA, Waterman C, Heinonen A, Janssen PA, Donaldson MG, Mallinson A, Riddell L, Kruse K, Prior JC, Flicker L (2002) Community-based exercise program reduces risk factors for falls in 65-to 75-year-old women with osteoporosis: randomised controlled trial. CMAJ 167:997–1004
Heinonen A, Kannus P, Sievänen H, Oja P, Pasanen M, Rinne M, Uusi-Rasi K, Vuori I (1996) Randomised controlled trial of effect of high-impact exercise on selected risk factors for osteoporotic fractures. Lancet 348:1343–1347
Shaw JM, Snow CM (1998) Weighted vest exercise improves indices of fall risk in older women. J Gerontol 53:M53–M58
Lord SR, Ward JA, Williams P, Zivanovic E (1996) The effects of a community exercise program on fracture risk factors in older women. Osteoporosis Int 6(5):361–367
Shigematsu R, Chang M, Yabushita N, Sakai T, Nakagaichi M, Nho H, Tanaka K (2002) Dance-based aerobic exercise may improve indices of falling risk in older women. Age Ageing 31(4):261–266
Carter ND, Khan KM, Petit MA, Heinonen A, Waterman C, Donaldson MG, Janssen PA, Mallinson A, Riddell L, Kruse K, Prior JC, Flicker L, McKay HA (2001) Results of a 10 week community based strength and balance training program to reduce fall risk factors: a randomised controlled trial in 65–75 year old women with osteoporosis. Br J Sports Med 35:348–351
Mills EM (1994) The effect of low intensity aerobic exercise on muscle strength, flexibility and balance among sedentary elderly persons. Nurs Res 43(4):207–211
Swanenburg J, de Bruin ED, Stauffacher M, Mulder T, Uebelhart D (2007) Effects of exercise and nutrition on postural balance and risk of falling in elderly people with decreased bone mineral density: randomized controlled trial pilot study. Clin Rehabil 21:523–534
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gunendi, Z., Ozyemisci-Taskiran, O. & Demirsoy, N. The effect of 4-week aerobic exercise program on postural balance in postmenopausal women with osteoporosis. Rheumatol Int 28, 1217–1222 (2008). https://doi.org/10.1007/s00296-008-0651-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-008-0651-3