Abstract
The authors prospectively investigated 155 pregnant women, without a history of rheumatic disease who visited the Department of Obstetrics and Gynecology for routine antenatal care, to evaluate the prevalences and clinical features of arthralgia and arthritis in healthy pregnant women. Mean of the 155 subjects’ ages was 31.8 ± 3.8 (years, ±SD). Arthralgia was found in 26 (16.7%) and arthritis in 15 (9.6%) pregnant women. Arthralgia or arthritis developed in the third trimester (28–40 weeks of gestation), except in one case (16 weeks of gestation). Most commonly involved joints were the proximal interphalangeal (n = 19, 12.2%). Rheumatoid factor and antinuclear antibody were negative in patients with arthritis. Ten women (6.8%) had persistent arthralgia for over 6 weeks, post-delivery. Four of them were followed up at Rheumatology Clinic and were diagnosed as having spondyloarthropathy (1), or unspecified arthralgia (3). In conclusion, arthralgia is common during pregnancy and most frequent in proximal interphalangeal joints.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is known that, virtually every woman experiences some degree of musculoskeletal discomfort during pregnancy and that ca. 25% have at least temporary disabling symptoms [1] Lower back, pelvic girdle, symphysis pubis, hip pain, and carpal tunnel syndrome, and thrombophlebitis are common musculoskeletal symptoms during pregnancy [2, 3]. Physiologic changes during pregnancy, such as, soft tissue swelling and joint laxity, are thought to be predisposed to joint problems [2], and maternal hormonal changes during pregnancy, that is, elevated levels of estrogen, progesterone, relaxin, cortisol, and others, may be related to these articular changes and symptoms. Investigations have revealed that almost a third of all pregnant women have complaints related to lower back and/or pelvic girdle pain [4, 5]. However, the prevalences of arthralgia and arthritis have not been reported in healthy pregnant women, although patients with rheumatic disease may experience altered disease activity during pregnancy [4–6].
The aim of the present study was to investigate the prevalences and clinical features of arthralgia and arthritis in healthy pregnant women.
Materials and methods
This prospective study was conducted to investigate the prevalences and clinical features of arthralgia and arthritis in healthy pregnant women. We enrolled 155 healthy pregnant women, who consecutively visited the Department of Obstetrics and Gynecology, Seoul National University Hospital for routine antenatal care from January 2004 to May 2004, and were followed up until 6 weeks after delivery. This study was approved by the Institutional Review Board at Seoul National University Hospital after reviewing ethical issues, and written informed consents were obtained from all 155 participants. We excluded patients with lower back pain, pelvic girdle pain, symphysis pubis pain, hip pain, carpal tunnel syndrome, thrombophlebitis, previous rheumatic disease or other conditions, such as, trauma or infection. The definition of arthralgia was subjective pain in a joint, and that of arthritis was at least one of the following signs; joint pain on motion, joint swelling, joint tenderness or erythema on a joint. Complete blood cell count, erythrocyte sedimentation rate, serum C-reactive protein, chemistry, rheumatoid factor (RF), and antinuclear antibody (ANA) were checked in the arthritis group, and joint sonography was performed in six arthritis patients. The questionnaire administered at enrollment was composed of demographic data (height, weight, gestational age at enrollment, multiparity), presence of morning stiffness, sites of arthralgia, a previous rheumatic disease history, and the presence of other comorbid disease. Patients were examined at initial visit and followed every 4 weeks during second trimester, every 2 weeks during third trimester, at the time of delivery, and at 6 weeks after delivery. Persistent arthralgia was defined as pain persisting for over 6 weeks after delivery. Women with persistent arthralgia (n = 4) were followed at the Rheumatology Clinic for 11–96 weeks after delivery.
Statistical analysis
The Mann–Whitney U test was used to compare clinical variables in different groups at baseline. The Chi-square test was used to compare clinical group variables after delivery. SPSS version 10.0 was used throughout, and P values of <0.05 were considered statistically significant.
Results
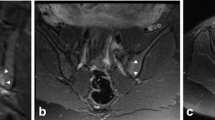
One hundred and fifty-five healthy pregnant women were enrolled. Mean age of these study subjects was 31.8 ± 3.8 (years, ±SD). Arthralgia was found in 26 (16.7%) and arthritis in 15 (9.6%). Arthralgia and arthritis developed in the third trimester (28–40 weeks of gestation) except in one case (16 weeks of gestation) (Table 1). Arthralgia worsened in the morning and after a nap in these patients. Four patients with arthralgia (4/26, 15.3%) had morning stiffness, lasting for more than 1 h. The joints involved were; proximal interphalangeal (PIP, n = 19, 12.2%), knee (n = 9, 5.8%), wrist (n = 7, 4.5%), ankle (n = 7, 4.5%), metacarpophalangeal (n = 4, 2.5%), and distal interphalangeal joint (n = 1, 0.6%) (Fig. 1). Rheumatoid factor and antinuclear antibody were negative in patients with arthritis (n = 11). Three patients were found to have synovitis by joint sonography (Fig. 2).
Small joints of the hands were involved in 12.9% (20/155) of the study subjects (Table 2). When their pattern of involvement was analyzed, most had PIP involvement only or PIP and MCP involvement.
One hundred and forty-seven participants (94.8%) were followed up until 6 weeks after delivery (23 in the arthralgia group, 124 in the non-arthralgia group). Eight women were lost to follow-up after delivery, three in the arthralgia group and five in the non-arthralgia group (two follow-up loss after delivery, one at 38 weeks, one had congenital cytomegalovirus infection leading to pregnancy termination at 22 weeks and one had spontaneous abortion at 11 weeks of gestational age). One hundred and thirty women (83.8%) delivered at Seoul National University Hospital, and 17 (10.9%) who delivered at private hospitals were contacted by telephone. The female to male newborn baby ratio was approximately 1 (78 vs. 75) and was not different between the arthralgia and non-arthralgia groups. The number of twin deliveries was 14 (5 vs. 9 in these two groups, respectively, P = 0.096), 24 babies were large for gestational age (3 vs. 21, respectively, P = 0.312), and 9 had a congenital anomaly (3 vs. 6, respectively, P = 0.229) (Table 3). Ten women (10/147, 6.8%) had arthralgia that persisted for more than 6 weeks after delivery, and four of these were followed up after the postpartum period at a Rheumatology Clinic. They were diagnosed as having; spondyloarthropathy (n = 1), and unspecified arthralgia (n = 3). Subgroup analysis on the arthralgia group dichotomized according to the persistence of arthralgia, showed no difference in delivery outcome.
Discussion
Pregnancy induces several changes in the musculoskeletal system. Progressive lordosis is most commonly caused by the enlarging uterus. Hypermobility of the sacroiliac and pubic joint are common. Lower back pain, hip pain, carpal tunnel syndrome, and thrombophlebitis also tend to develop during pregnancy. In patients with systemic rheumatic disease, disease activity may be altered during pregnancy. An increase in the disease activity of systemic lupus erythematous during pregnancy would be expected due to increased levels of estrogen, prolactin, and helper T cell cytokines [6]. In rheumatoid arthritis patients, disease activity may be decreased during pregnancy. The risk of new onset rheumatoid arthritis is reported to be reduced during pregnancy, but is increased after delivery due to hormonal factors [7, 8].
In the present study, we investigated arthralgia and arthritis in healthy pregnant women without a history of rheumatic disease. Rheumatologists (HJC, JCL) screened all healthy pregnant women using questionnaires and examined women who complained of arthralgia. The frequencies of arthralgia and arthritis were 16.7% (26/155) and 9.6% (15/155) among our study subjects. Arthralgia usually developed in the third trimester and the proximal hand interphalangeal joint was the most commonly involved. In most cases, arthralgia and arthritis improved spontaneously.
Iijima [9] reported on the prediction of the postpartum onset of rheumatoid arthritis in Japanese women. A total of 2,547 healthy pregnant women were examined prospectively, and 410 subjects were followed up for 1 year after delivery. Two of nine women, positive for rheumatoid factor at enrollment developed rheumatoid arthritis at 1 and 3 months postpartum, respectively. Transient arthralgia was found within 12 months postpartum, more frequently in women with rheumatoid factor than those without it (33.3 vs. 8.1%). They reported that the postpartum onset of rheumatoid arthritis was observed in at least 2 of 2,547 healthy subjects (0.08%), and it could be predicted by positive rheumatoid factor test.
In our study, rheumatoid factor and antinuclear antibody were both negative in patients with arthritis (n = 11). Moreover, 10 women (6.8%) had persistent arthralgia over 6 weeks after delivery. Of these patients, one had spondyloarthropathy, and three unspecified arthralgia. Concerning hand arthralgia, nearly half of the cases (9/20, 45%) had persistent symptoms or signs at 6 weeks post-delivery. The prevalence of arthralgia in women found in the present study was similar to that found in a Japanese study [9]. However, in our cohort, there was no newly developed rheumatoid arthritis during pregnancy.
To our knowledge, this is the first descriptive report about arthralgia and arthritis in the small joints of the hands resembling rheumatoid arthritis during pregnancy. While discomfort of small hand joints is relatively common during pregnancy, we were unable to find a report in the medical literature describing hand arthritis.
The mechanism of arthralgia in hand joints is unclear. Several possible hypotheses and explanations could be considered. First, pregnancy is associated with physiological changes, such as, soft tissue edema and joint laxity [1, 2, 10, 11], which may cause pain in pelvic and/or large limb joints and in small hand joints. Arthralgia in our cases usually developed during the third trimester, which is characterized by an increased plasma volume and a decreased serum osmotic pressure, which results in excess body fluid collection. Second, disturbances in hormonal balance may result in fluid retention during pregnancy, and this increased fluid may induce joint fluid collection and subsequently cause pain and stiffness [1, 10]. Changes in the levels of circulating cytokines, which has been reported to occur during and after pregnancy in patients with rheumatic disease [12], may contribute to arthralgia in healthy pregnant women. Third, metabolic balance derangement that occur during certain diseases may cause joint inflammation. These diseases include diabetes mellitus, hepatic diseases, hemochromatosis, and others [13–15].
It should be noted that our results may not represent the characteristics of community-based healthy pregnant women, because our hospital is a tertiary center.
In conclusion, the frequencies of arthralgia and arthritis were 16.7, and 9.6%, respectively, in our healthy pregnant female cohort. The proximal interphalangeal hand joint was most commonly involved. In most cases, arthralgia and arthritis subsided spontaneously. Spondyloarthropathy developed in one subject (0.6%). Further study is required to identify those factors that predict arthritis during pregnancy and to elucidate its pathophysiology.
References
Ritchie JR (2003) Orthopedic considerations during pregnancy. Clin Obstet Gynecol 46(2):456–466
Borg-Stein J, Dugan SA, Gruber J (2005) Musculoskeletal aspects of pregnancy. Am J Phys Med Rehabil 84(3):180–192
Lowery CL (1995) Sudden joint and extremity pain in pregnancy. Obstet Gynecol Clin North Am 22(1):173–190
Albert H, Godskesen M, Westergaard J (2001) Prognosis in four syndromes of pregnancy-related pelvic pain. Acta Obstet Gynecol Scand 80(6):505–510
Albert H, Godskesen M, Westergaard J (2000) Evaluation of clinical tests used in classification procedures in pregnancy-related pelvic joint pain. Eur Spine J 9(2):161–166
Petri M (1997) Hopkins lupus pregnancy center: 1987 to 1996. Rheum Dis Clin North Am 23:1–14
Silman AJ, Kay A, Brennan P (1992) Timing of pregnancy in relation to the onset of rheumatoid arthritis. Arthritis Rheum 35:152–155
Barrett JH, Brennan P, Fiddler M, Silman AJ (1999) Does rheumatoid arthritis remit during pregnancy and relapse postpartum? Results from a nationwide study in the United Kingdom performed prospectively from late pregnancy. Arthritis Rheum 42(6):1219–1227
Iijima T, Tada H, Hidaka Y, Yagoro A, Mitsuda N, Kanzaki T, Murata Y, Amino N (1998) Prediction of postpartum onset of rheumatoid arthritis. Ann Rheum Dis 57(8):460–463
Ekman-Ordeberg G, Salgeback S, Ordeberg G (1987) Carpal tunnel syndrome in pregnancy. A prospective study. Acta Obstet Gynecol Scand 66(3):233–235
Schauberger CW, Rooney BL, Goldsmith L, Shenton D, Silva PD, Schaper A (1996) Peripheral joint laxity increases in pregnancy but does not correlate with serum relaxin levels. Am J Obstet Gynecol 174:667–671
Ostensen M, Forger F, Nelson JL, Schuhmacher A, Hebisch G, Villiger PM (2005) Pregnancy in patients with rheumatic disease: anti-inflammatory cytokines increase in pregnancy and decrease post partum. Ann Rheum Dis 64:839–844
Ruddy S, Harris ED, Sledge CB (eds) (2001) Kelley’s textbook of rheumatology. W·B Saunders Company, Philadelphia
Chi ZC, Ma SZ (2003) Rheumatologic manifestations of hepatic diseases. Hepatobiliary Pancreat Dis Int 2:32–37
Schumann K (2001) Safety aspects of iron in food. Ann Nutr Metab 45:91–101
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Choi, H.J., Lee, J.C., Lee, Y.J. et al. Prevalence and clinical features of arthralgia/arthritis in healthy pregnant women. Rheumatol Int 28, 1111–1115 (2008). https://doi.org/10.1007/s00296-008-0596-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-008-0596-6