Abstract
Ankylosing spondylitis (AS) is characterized by ankylosis of axial joints but osteoporosis is also a well-reported feature. T cells have been implicated as a source of receptor activator of NFκB ligand (RANKL) in inflammatory bone diseases. Hence, we assessed whether T cells in patients with AS act as a source of RANKL too. Therefore, we investigated the expression of RANKL on T cells from 21 patients with AS by flow cytometry. Bone mineral density (BMD) was evaluated by quantitative computer tomography (QCT) and dual X-ray absorptiometry (DXA) and correlated with serum levels of osteoprotegerin (OPG) and RANKL. BMD was decreased in 45% of all patients when measured with DXA (48% with QCT) and correlated negatively with OPG. Expression of intracellular RANKL was increased on CD4+ (84 vs. 70%) and CD8+ (85.2 vs. 65.3%, P < 0.05) T cells in patients with AS, whereas expression of membrane-bound RANKL was significantly lower (CD4+: 2.2 vs. 8.5% and CD8+: 0.7 vs. 3.2%, P < 0.01). Our results indicate that surface and intracellular RANKL production is differentially regulated on T cells of patients with AS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ankylosing spondylitis (AS) is a chronic, disabling rheumatic disease, which initially mainly involves the sacroiliac joints and in later stages affects the vertebral column. Alongside the inflammation, new bone formation leads to ossifications and progressive ankylosis, but bone loss leading to osteopenia/osteoporosis is also a well-reported feature of AS [1].
Since the identification of the factors involved in the control of osteoclasts, significant progress in the understanding of bone remodeling has been made. These factors include the tumor necrosis factor α (TNF-α) family member RANKL [2] and its soluble decoy receptor OPG [3]. Upon binding of RANKL to its cognate receptor RANK on osteoclast precursors osteoclast differentiation is induced [4]. However, this process is counteracted by OPG, which can interact with RANKL and thereby prevents the activation of the RANK signaling cascade. RANKL is mainly produced by osteoblasts but also activated T cells have also been found to be a fundamental source of soluble RANKL in diseased conditions [5]. Kong et al. [6] further underlined the relationship between bone and immune system by demonstrating that activated T cells regulate bone loss in pathological conditions, such as rheumatoid arthritis [7]. Further intense research demonstrated, that both activated T cells and synovial fibroblast-like cells in the joints of patients with rheumatoid arthritis (RA) express membrane-bound (mb)RANKL and soluble RANKL, thereby promoting focal bone erosions and periarticular bone loss [8]. In addition, a recently published study showed that the expression of RANKL by T cells has an important impact on the bone resorption process in chronic periodontal disease as well [9].
In this study, we aimed at investigating the surface and intracellular expression of RANKL on activated T cells of patients with AS. Moreover, we assessed bone mineral density (BMD) of those patients by DXA and QCT. BMD values of patients were further correlated with serum levels of OPG and RANKL.
Patients and methods
Patients
Twenty-one patients with diagnosed AS (mean age 51 ± 3; range 25–68 years) were enrolled in this study. Patients with a history of other bone diseases or cancer, and those who where taking drugs that are capable of affecting BMD (like bis-phosphonates or TNF α blockers but with the exception of calcium and vitamin D supplements) were excluded from the study. The same exclusion criteria were applied to 15 sex- and age- matched healthy controls (mean age 49 ± 4; range 25–69 years). All the patients provided informed and written consent to participate. The study protocol was approved by the ethical committee of the St. Vincent Hospital. Routine laboratory measures were carried out in the laboratory of the clinic according to standard procedures. Additionally, aliquots of serum samples were stored at −70°C until they were analyzed by ELISA. Clinical indices of disease activity (BASDAI) [10] and function (BASFI) [11] were evaluated by disease-specific questionnaires. Global pain of the patients was determined with a visual analog scale (VAS). Disease duration was defined as the period from appearance of symptoms until the time of inclusion into this study.
Bone mineral densitometry
Bone density was measured using DXA (GE healthcare Lunar iDXA ME +200066) and QCT (QCTPRO™, Mindways Software Inc., on Philips MX 8000) at the lumbar spine (L1–L4) and the total hip. According to the World Health Organization (WHO) [12], osteopenia was defined as a T score <−1 and osteoporosis as a T score <−2.5 measured by DXA. Values measured at the lumbar spine by QCT (mg/cm3) below the method-respective threshold of 100 mg/cm3 hydroxylapatite are considered to be osteopenic and osteoporotic as values below the method-respective threshold of <80 mg/cm3 hydroxylapatite.
ELISA
The serum concentrations of free soluble RANKL and osteoprotegerin were analyzed by a commercially available ELISA kits from Biomedica, Vienna, Austria according to the manufacturer’s protocol.
Flow cytometry
We performed flow cytometric analysis of T cell cytokine production essentially as previously described [13]. Freshly peripheral blood mononuclear cells (PBMC) were isolated by density centrifugation from heparinized blood samples and were stimulated for cytokine production with 10 ng/ml phorbol myristate acetate (PMA), 1.25 μg/ml ionomycin for 4 h at 37°C in a 5% CO2 atmosphere and in the presence of 10 μg/ml brefeldin A (BFA) (all three are from Sigma Chemical Co, USA). Cells were fixed with 2% formaldehyde, permeabilized by 0.1% saponin (Sigma Chemical Co.) and stained for intracellular cytokines using (PE) anti-human RANKL (from eBioscience, San Diego, California, USA) in combination with staining for T cell surface markers, using PeCy-7 conjugated anti-CD4 and APC conjugated anti-CD8 (both from Becton Dickinson, San Jose, CA, USA). For staining membrane-bound (mb) RANKL, the cells were neither fixed nor permeabilized, because we observed that nonpermeabilized but fixed cells used for surface staining showed a false high expression of mbRANKL, similar to the results of the intracellular staining which suggests that formaldehyde makes the cells permeable (data not shown). Stained cells were analyzed using the FACS Calibur (Becton Dickinson) and the Cell Quest Pro software.
Statistical analysis
All statistical analyses were performed by SPSS 14.0 software for Windows. All results are presented as means and standard error of the mean (SEM). Differences between the two groups were tested using the Mann–Whitney U test. Correlation analysis was performed using the Spearman test. In all cases, the minimal requirement for establishing statistical significance was <0.05.
Results
Patient characteristics
The clinical data are given in Table 1. On average the patients with AS had a moderate disease activity with a mean disease duration of 25.4 years. Mean levels of PTH and 25(OH) vitamin D3 were within the normal range. Patients with AS showed mean serum OPG levels of 3.3 ± 0.4 pmol/l (normal range from 1.2 to 6.6 pmol/l) and soluble RANKL 0.1 ± 0.0 pmol/l (normal range from 0.0 to 2.7 pmol/l) which were both within the normal range.
Frequency of osteopenia and osteoporosis and the relationship with circulatory OPG and RANKL
Figure 1 shows the prevalence of osteopenia or osteoporosis in patients with AS. Abnormal BMD was detected with DXA at the total hip in 45% of all cases; there was a significant correlation between T scores of the total hip and the lumbar spine (LS, Spearman correlation coefficient r = 0.54; P = 0.01). Measurements of the LS by QCT showed that 48% of all cases were osteopenic or osteoporotic, especially within the male population. Measurements of the total hip by QCT and DXA showed a significant correlation (r = 0.87; P = 0.001) but in contrast values of the QCT and DXA measurements of the LS did not (r = 0.195; P = 0.42).
Comparison of the relative frequencies of osteopenia or osteoporosis measured at different sites and with two different methods (DXA and QCT) in patients with AS. *Significantly different from QCT LS in men (P ≤ 0.05). TH total hip, LS lumbar spine, DXA dual-energy X-ray absorptiometry, QCT quantitative computed tomography
Serum OPG levels were negatively correlated with lumbar spine BMD values, measured by QCT (r = −0.571; P = 0.025) and—although statistically not significant—they also tended to be negatively correlated with all other BMD measurements. Furthermore, serum levels of OPG were positively related with the age of the AS patients (r = 0.513; P = 0.025). Additionally, there was a significant negative relationship between spinal BMD measured by QCT and age (r = −0.630; P = 0.003).
Expression of intracellular and surface RANKL in T cells
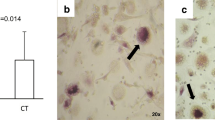
Cytokine expression was determined by three color flow cytometry. Permeabilized, fixed and stimulated T lymphocytes from peripheral blood of patients with AS showed a significantly higher expression of intracellular RANKL within the CD8+ T cell population compared to the healthy controls (85.2 vs. 65.3%, P < 0.05). Similar results were detected within the CD4+ T cell population, but they did not reach statistical significance (84 vs. 70%; Fig. 2). In contrast, the expression of surface RANKL on activated peripheral blood T cells from patients with AS was significantly lower in both cell subsets compared to healthy controls (CD4+ 2.23 vs. 8.5% and CD8+ 0.7 vs. 3.2%; P < 0.01; Fig 3). Statistically significant differences were detected between the two cell populations in each group, indicating that CD4+ T cells have a higher capacity to express surface RANKL.
Intracellular expression of RANKL in activated peripheral blood T lymphocytes in AS and healthy controls (CO) as determined by flow cytometry. a Representative dot plot diagrams showing the negative control (left column), RANKL-positive cells on CD4+ T cells (middle column) and RANKL-positive cells on CD8+ T cells (right column); b Black bars indicate the intracellular RANKL expression in patients with AS, and white bars show the expression in healthy controls. Each bar represents the mean percentage of RANKL-positive T cells ± SEM per group. *Significantly different from RANKL expression in CD8+ cells of CO (P < 0.05)
Cell surface expression of RANKL in activated peripheral blood T cells in patients with AS and healthy controls (CO) analyzed by flow cytometry. a Representative dot plot diagrams showing RANKL-positive cells on CD4+ T cells (left column) and RANKL-positive cells on CD8+ T cells (right column); b Black bars indicate the surface RANKL expression in patients with AS, and white bars show the expression in healthy controls. Each bar represents the mean percentage of RANKL-positive T cells ± SEM per group. **Significantly different from membrane bound RANKL expression of CO (P < 0.01). For definitions, see Fig. 2 legend
Discussion
Besides formation of new bone in form of osteophytes and syndesmophytes, bone loss is a well-documented and common complication in AS as well [14, 15]. To prove whether our patients are an appropriate group for studying bone loss, we determined bone density with two different methods, namely DXA and QCT. Compared with a previous study from Kudlacek et al. [16] that used a normal adult Austrian population to establish an appropriate normative database it is clearly evident that our patient cohort with a percentage of 45% had a much higher frequency of osteopenic values in the total hip compared to the healthy controls with about 12%. Furthermore, only about 15.5% of the collective in this study had z-scores <1, whereas about 85% of the AS-patients in our study showed z-scores <1. Both studies used Lunar systems for the BMD measurements and hence allow to compare these results.
BMD values of the lumbar spine were higher measured by DXA and lower using QCT, indicating that QCT is the more sensitive method for detecting low bone density at the lumbar spine in patient with AS, especially in the presence of syndesmophytes, as already reported in previous research [17, 18]. We observed this phenomenon mainly in men which may be due to the different gender specific clinical manifestations in AS. Moreover, levels of PTH and 25(OH) vitamin D3 were assessed to exclude that bone loss in these patients was a result of other bone disorders, such as secondary hyperparathyroidism.
In our correlation study between BMD and circulating levels of OPG and RANKL in patients with AS we found that serum OPG levels were significantly negatively correlated with lumbar spine BMD values, determined by QCT, and also showed a non-significant negative relationship using DXA measurements. Additionally, serum levels of OPG showed a significant positive correlation with age. These observations may be explained by the compensatory reaction of OPG to encounter age-related bone loss, a phenomenon that was also seen in previous studies [19–21]. Moreover, circulating levels of RANKL were not different in the AS and the control group, which is in contrast to the report from Kim et al. who found significantly elevated levels of RANKL in the serum of AS patients [22]. This discrepancy may be explained by the small sample size of our study.
This is the first study to show that peripheral blood T cells respond to an in vitro stimulation with ionomycin and PMA with a higher intracellular production of RANKL in patients with AS compared to the healthy controls. This high extent of intracellular RANKL expression was observed in both T cell populations, but the increase of RANKL in patients with AS was significant only for the CD8+ T cell subpopulation. Our observation may be explained by the strong association between the MHC-class I molecule HLA-B27 and AS [23]. The arthritogenic peptide hypothesis proposes that AS is a consequence of the antigen presentation function of HLA-B27 to CD8+ T cells, resulting in an immune mediated pathogenesis. Also, a previous study has demonstrated a strong antigen specific T cell cytokine response with a significant reduction after infliximab treatment only in CD8+ T cells from patients with AS [24]. Although the intimate interactions between bone and immune cells show an important role for CD8+ cytotoxic T cells and CD4+ T helper cells in AS and rheumatoid arthritis, detailed analysis investigating the role of CD8+ or CD4+ T cells in the pathogenesis of these immune-mediated disease are scarce [25].
Somewhat unexpectedly, we found that the cell surface expression of RANKL on activated peripheral blood T cells was significantly lower in the group of patients with AS compared to the healthy controls (Fig. 3). This result is contrary to a recent observation in patients with rheumatoid arthritis (RA), in which higher levels of surface RANKL were detected in patients with RA compared to healthy controls [26]. However, one has to consider that the bone-related pathologies of RA and AS are quite different. Therefore, a lower expression of surface RANKL on T cells in AS may contribute to its less severe bone-destructive disease pattern.
Further, we could show that intracellular RANKL is more abundantly expressed in activated T cells than the membrane-bound form. The production of soluble RANKL is regulated at various levels, including transcriptional, translational and post-translational mechanisms. Especially, the post-translational regulation of RANKL shedding by members of a disintegrin and metalloproteinase domain (ADAM) family or by matrix metallo-proteinases (MMPs), like MMP-3, MMP-7 or MMP-14, seems to be important as e.g. MMP-14-deficient mice display increased osteoclastogenesis in vivo [27, 28]. However, little is known about the complex regulation of soluble RANKL production, which may serve as an important clinical predictor for bone loss. Further studies are needed that focus on the biological and pathological importance of RANKL shedding as well as on the contribution of surface and soluble RANKL in osteoclast differentiation, which has not been determined unambiguously yet [29, 30].
Although a relevant positive control group as a purely bone resorptive disease such as rheumatoid arthritis is lacking in this study, our results presented here underline the involvement of immune cells in the pathogenesis of AS and indicate that activated CD4+ and CD8+ T cells contribute to the production of RANKL in the inflammatory bone-resorptive disease AS.
References
Toussirot E, Wendling D (2000) Bone mass in ankylosing spondylitis. Clin Exp Rheumatol 21:16–20
Wong BR, Rho J, Arron J, Robinson E, Orlinick J, Chao M, Kalachikov S, Cayani E, Bartlett FS 3rd, Frankel WN, Lee SY, Choi Y (1997) TRANCE is a novel ligand of the tumor necrosis factor receptor family that activates c-Jun N-terminal kinase in T-cells. J Biol Chem 272:25190–25194
Simonet WS, Lacey DL, Dunstan CR, Kelley M, Chang MS, Lüthy R, Nguyen HQ, Wooden S, Bennett L, Boone T, Shimamoto G, DeRose M, Elliott R, Colombero A, Tan HL, Trail G, Sullivan J, Davy E, Bucay N, Renshaw-Gegg L, Hughes TM, Hill D, Pattison W, Campbell P, Sander S, Van G, Tarpley J, Derby P, Lee R, Boyle WJ (1997) Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell 89:309–319
Lacey DL, Timms E, Tan HL, Kelley MJ, Dunstan CR, Burgess T, Elliott R, Colombero A, Elliott G, Scully S, Hsu H, Sullivan J, Hawkins N, Davy E, Capparelli C, Eli A, Qian YX, Kaufman S, Sarosi I, Shalhoub V, Senaldi G, Guo J, Delaney J, Boyle WJ (1998) Osteoprotegerin (OPG) ligand is a cytokine that regulates osteoclast differentiation and activation. Cell 93:165–176
Kong YY, Yoshida H, Sarosi I, Tan HL, Timms E, Capparelli C, Morony S, Oliveira-dos-Santos AJ, Van G, Itie A, Khoo W, Wakeham A, Dunstan CR, Lacey DL, Mak TW, Boyle WJ, Penninger JM (1999) OPGL is a key regulator of osteoclastogenesis, lymphocyte development and lymph-node organogenesis. Nature 397:315–323
Kong YY, Feige U, Sarosi I, Bolon B, Tafuri A, Morony S, Capparelli C, Li J, Elliott R, McCabe S, Wong T, Campagnuolo G, Moran E, Bogoch ER, Van G, Nguyen LT, Ohashi PS, Lacey DL, Fish E, Boyle WJ, Penninger JM (1999) Activated T-cells regulate bone loss and joint destruction in adjuvant arthritis through osteoprotegerin ligand. Nature 402:304–309
Kotake S, Udagawa N, Hakoda M, Mogi M, Yano K, Tsuda E, Takahashi K, Furuya T, Ishiyama S, Kim KJ, Saito S, Nishikawa T, Takahashi N, Togari A, Tomatsu T, Suda T, Kamatani N (2001) Activated human T cells directly induce osteoclastogenesis from human monocytes: possible role of T cells in bone destruction in rheumatoid arthritis patients. Arthritis Rheum 44:1003–1012
Schett G (2006) Rheumatoid arthritis: inflammation and bone loss. Wien Med Wochenschr 156:34–41
Kawai T, Matsuyama T, Hosokawa Y, Makihira S, Seki M, Karimbux NY, Goncalves RB, Valverde P, Dibart S, Li YP, Miranda LA, Ernst CW, Izumi Y, Taubman MA (2006) B and T lymphocytes are the primary sources of RANKL in the bone resorptive lesion of periodontal disease. Am J Pathol 169:987–997
Garrett S, Jenkinson T, Kennedy LG, Withelock H, Gaisford P, Calin A (1994) A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol 21:2286–2291
Calin A, Garrett S, Whitelock H, Kennedy LG, O’Hea J, Mallorie P, Jenkinson T (1994) A new approach to defining functional ability in ankylosing spondylitis: the development of the Bath Ankylosing Spondylitis Functional Index. J Rheumatol 21:2281–2285
World Health Organization. Assessment of fracture risk, its application to screening for postmenopausal osteoporosis (1994) Report of a WHO Study Group. WHO Technical Report Series No. 843. WHO, Geneva, pp 1–129
Pietschmann P, Gollob E, Brosch S, Hahn P, Kudlacek S, Willheim M, Woloszczuk W, Peterlik M, Tragl KH (2003) The effect of age and gender on cytokine production by human peripheral blood mononuclear cells and markers of bone metabolism. Exp Gerontol 38:1119–1127
Karberg K, Zochling J, Sieper J, Felsenberg D, Braun J (2005) Bone loss is detected more frequently in patients with ankylosing spondylitis with syndesmophytes. J Rheumatol 32:1290–1298
Capaci K, Hepguler S, Argin M, Tas I (2003) Bone mineral density in mild and advanced ankylosing spondylitis. Yonsei Med J 44:379–384
Kudlacek S, Schneider B, Peterlik M, Leb G, Klaushofer K, Weber K, Woloszczuk W, Willvonseder R, Austrian Study Group on Normative Values of Bone Metabolism (2003) Normative data of bone mineral density in an unselected adult Austrian population. Eur J Clin Invest 33:332–339
Lee YS, Schlotzhauer T, Ott SM, van Vollenhoven RF, Hunter J, Shapiro J, Marcus R, McGuire JL (1997) Skeletal status of men with early and late ankylosing spondylitis. Am J Med 103:233–241
Reid DM, Nicoll JK, Kennedy NS, Smith MA, Tothill P, Nuki G (1986) Bone mass in ankylosing spondylitis. J Rheumatol 13:932–935
Khosla S, Arrighi HM, Melton LJ 3rd, Atkinson EJ, O’Fallon WM, Dunstan C, Riggs BL (2002) Correlates of osteoprotegerin levels in women and men. Osteoporos Int 13:394–399
Pulsatelli L, Dolzani P, Silvestri T, Caraceni P, Facchini A, Ravaglia G, Salvarani C, Melicòni R, Mariani E (2004) Soluble receptor activator of nuclear factor-κB ligand (sRANKL)/osteoprotegerin balance in ageing and age-associated diseases. Biogerontol 5:119–127
Kudlacek S, Schneider B, Woloszezuk W, Pietschmann P, Willvonseder R (2003) Serum levels of osteoprotegerin increase with age in a healthy adult population. Bone 32:681–686
Kim HR, Kim HY, Lee SH (2006) Elevated serum levels of soluble receptor activator of nuclear factors-KappaB ligand (sRANKL) and reduced bone mineral density in patients with ankylosing spondylitits (AS). J Rheumatol 45:1197–2000
Boyle LH, Goodall JC, Opat SS, Gaston JS (2001) The recognition of HLA-B27 by human CD4(+) T-lymphocytes. J Immunol 167:2619–2624
Zou J, Rudwaleit M, Brandt J, Thiel A, Braun J, Sieper J (2003) Down-regulation of the nonspecific and antigen-specific T cell cytokine response in ankylosing spondylitis during treatment with infliximab. Arthritis Rheum 48:780–790
Udagawa N, Kotake S, Kamatani N, Takahashi N, Suda T (2002) The molecular mechanism of osteoclastogenesis in rheumatoid arthritis. Arthritis Res 4:281–289
Miranda-Carús ME, Benito-Miguel M, Balsa A, Cobo-Ibáñez T, Pérez de Ayala C, Pascual-Salcedo D, Martín-Mola E (2006) Peripheral blood T lymphocytes from patients with early rheumatoid arthritis express RANKL and interleukin-15 on the cell surface and promote osteoclastogenesis in autologous monocytes. Arthritis Rheum 54(4):1151–1164
Schlondorff J, Lum L, Blobel CP (2001) Biochemical and pharmacological criteria define two shedding activities for TRANCE/OPGL that are distinct from the tumor necrosis factor alpha convertase. J Biol Chem 276:14665–14674
Hikita A, Yana I, Wakeyama H, Nakamura M, Kadono Y, Oshima Y, Nakamura K, Seiki M, Tanaka S (2006) Negative regulation of osteoclastogenesis by ectodomain shedding of receptor activator of NF-κB ligand. J Biol Chem 48:36846–36855
Lum L, Wong BR, Josien R, Becherer JD, Erdjument-Bromage H, Schlöndorff J, Tempst P, Choi Y, Blobel CP (1999) Evidence for a role of a tumor necrosis factor-alpha (TNF-alpha)-converting enzyme-like protease in shedding of TRANCE, a TNF family member involved in osteoclastogenesis and dendritic cell survival. J Biol Chem 7:13613–13618
Nakashima T, Kobayashi Y, Yamasaki S, Kawakami A, Eguchi K, Sasaki H, Sakai H (2000) Protein expression and functional difference of membrane-bound and soluble receptor activator of NF-kappaB ligand: modulation of the expression by osteotropic factors and cytokines. Biochem Biophys Res Commun 275:768–775
Acknowledgments
The authors are very grateful to all enrolled patients with ankylosing spondylitis, especially to Maria Nimführ, the president of the support group “Morbus Bechterew” in Vienna, for their dedication and participation in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stupphann, D., Rauner, M., Krenbek, D. et al. Intracellular and surface RANKL are differentially regulated in patients with ankylosing spondylitis. Rheumatol Int 28, 987–993 (2008). https://doi.org/10.1007/s00296-008-0567-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-008-0567-y