Abstract
Generalized subcutaneous edema is an uncommon manifestation of inflammatory myopathy. We report a 48-year-old female patient who presented with severe generalized edema, an erythematous skin rash, dysphagia and proximal muscle weakness. She was diagnosed with dermatomyositis from the clinical signs, increased muscle enzymes, electromyographic findings and a muscle biopsy. Magnetic resonance imaging revealed increased signal intensity in the muscular and subcutaneous layers. The conditions causing generalized edema were excluded. It was concluded that the generalized edema was secondary to dermatomyositis. Aggressive treatments with high-dose glucocorticoids and immunosuppressive agents were used to control the severe subcutaneous edema.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periorbital edema is a common manifestation of inflammatory myopathy. However, generalized subcutaneous edema is an unusual presenting feature [1]. The clinical course of generalized edema varies and early recognition is essential for disease remission [1–11]. Because of the few reported cases, there are no guidelines for the management of this condition. We reported a female patient with acute edematous dermatomyositis (DM). Generalized edema was detected by magnetic resonance imaging (MRI) and treated successfully with high-dose steroid and immunosuppressive agents.
Case report
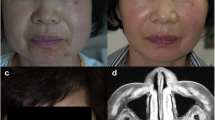
A 48-year-old woman was admitted to our hospital with erythematous skin eruptions, body swelling and progressive proximal muscle weakness with duration of 1 month. Gottron’s papules in the hand dorsum, a periorbital heliotrope rash, a “V” sign on her neck and a “Shawl” sign over her upper back were observed. A physical examination revealed erythematous skin lesions with generalized non-pitting edema (Fig. 1a). A neurological examination showed decreased muscle power in her shoulder and pelvic girdles.
Generalized edema in a 48-year-old woman with acute dermatomyositis. a Gross appearance upon admission. Severe generalized edema with Gottron’s papules in her hands and heliotrope rashes in both eyelids. b The resolution of the edema after treatment with high-dose steroid and immunosuppressive agents
The laboratory test revealed a white blood cell count of 16,200/mm3, a hemoglobin level of 14.6 g/dL, a platelet count of 131,000/mm3, an erythrocyte sedimentation rate of 26 mm/h and a C-reactive protein level of 4.2 mg/dL. The muscle enzymes were elevated (normal levels in parentheses): creatine kinase 10,056 IU/L (0–170), myoglobin 19,064 ng/ml (10–92), aldolase 40.3 U/L (0–8), aspartate transaminase 601 U/L (10–37), alanine transaminase 147 U/L (10–37). The immunofluorescent test for the antinuclear antibody and antineutrophil cytoplasmic antibody was negative. The serologic tests for rheumatoid factor, anti-Jo 1 and viral hepatitis were also negative. The chest radiography, electrocardiography and pulmonary function tests were unremarkable. The electromyographic findings were consistent with the inflammatory myopathy. Musculoskeletal ultrasonography revealed extensive subcutaneous edema (Fig. 2a). MRI of the upper and lower extremities showed increased signal intensity in the muscle layer and extensive fluid collection in the adjacent subcutaneous layer, which are compatible with subcutaneous and muscular edema (Fig. 2b, c). The Doppler examination and MR angiography were negative for deep vein thrombosis (Fig. 2d). A muscle biopsy was performed from the vastus lateralis of left thigh. Histological examination revealed that inflammatory cell infiltrates to perimysial area and perifascicular atrophy. Immunohistochemical stain for CD3, CD8 and CD20 was positive. These findings were more compatible with DM.
Radiological findings of the patient with acute edematous dermatomyositis. a Ultrasonography of the right hand shows extensive edematous changes in the subcutaneous fat and muscle layer. b Fat-suppressed T2-weighted magnetic resonance image (MRI) of both lower extremities reveals high signal intensity in the vastus lateralis, vastus intermedius, vastus medialis, rectus femoris, semitendinosus muscles and the subcutaneous fat layer (left panel coronal view of both thighs, right panel axial view of left thigh). c Fat-suppressed T2-weighted MRI of both forearms shows marked edematous thickening involving the subcutaneous fat layer (left panel sagittal view of right forearm, right panel axial view of left forearm). d Phase-contrast MR angiography reveals patent superficial and deep veins without luminal filling defect in the right forearm
The patient was treated with high-dose methylprednisolone (2 mg/kg per day i.v.) and methotrexate (25 mg/week i.m.), which resulted in rapid improvement in her muscle weakness and edema within 2 weeks along with markedly decreased muscle enzymes. Methylprednisolone was changed to 1 mg/day of oral prednisolone, which was later decreased to 0.5 mg/day. After 4 weeks, the patient relapsed. She was presented with more aggravated generalized edema, dysphagia and progressive elevation of her muscle enzyme levels. Human intravenous immunoglobulin (IVIg) was started at a dose of 400 mg/day for 5 days. Over the next 2 weeks, the dysphagia and muscle weakness were improved dramatically, but generalized edema was persistent despite the IVIg infusion. Therefore, a renal function test, thyroid function test and duplex Doppler ultrasonography were performed to rule out other causes of the generalized edema. However, those examinations were unremarkable. Search for an underlying malignancy and hypercoagulable states (including prothrombin time, partial thromboplastin time, bleeding time, thrombin time, anti-thrombin III, homocystein, protein C, protein S, factor VIII assay, factor XII assay, factor V Leiden, lupus anticoagulant, anticardiolipin antibodies, and anti-β2-glycoprotein I antibody) was negative. As the clinical picture was highly suggestive of edematous dermatomyositis refractory to IVIg, pulse methylprednisolone (1.0 g/day) was administered intravenously for 3 days, followed by an increase in the oral prednisolone dose to 2 mg/kg per day. After 2 months, the generalized edema gradually decreased with a concomitant increase in muscular strength. The patient was discharged with significant improvement in edema (Fig. 1b). Six months after the high-dose prednisolone therapy, the prednisolone dose was tapered to 5 mg/day. She has been in good general condition without a relapse over the follow-up period.
Discussion
This case had DM associated with generalized subcutaneous edema. Non-pitting edema developed concomitantly with DM, involving the face, trunk, upper and lower extremities. Other conditions causing the edema were excluded (e.g., congestive heart failure, renal failure, liver cirrhosis, hypothyroidism and deep vein thrombosis).
An association between inflammatory myopathy and generalized edema is extremely rare: 11 cases have been reported so far. Six cases were related to DM [2, 6, 7, 9, 11] and five cases were secondary to polymyositis (PM) [1, 4, 10]. The mechanisms underlying inflammatory myopathy with subcutaneous edema are unclear. It has been suggested that increased capillary permeability can cause edema, as a result of perivascular inflammation and endothelial damage [2, 5, 8, 11, 12]. Glucocorticoid can decrease the severity of edema through its potent anti-inflammatory and immunosuppressive effects [3]. Steroid therapy is required to control subcutaneous edema in most reported cases [1, 2, 6, 9–11]. Only two patients were spontaneously recovered without specific treatment [2, 4]. Six patients with active diseases complained of dysphagia. Three of these patients died from respiratory failure despite receiving aggressive treatment [10, 11]. Human IVIg is used as an alternative to azathioprine or methotrexate in inflammatory myopathy. One patient with generalized edema showed a favorable response after being administered IVIg [2], but the other case was refractory to the drug [11]. In our case, the generalized edema was not well controlled by IVIg, but responded to intravenous pulse methylprednisolone followed by high-dose oral prednisolone. A recent study reported striking clinical and biochemical response after treatment with rituximab in refractory PM and DM [13]. Although there was no report on the use of rituximab for DM associated with generalized edema, it can be used as another option for the refractory edema.
Generalized edema has been detected by computed tomography (CT) in previous reported cases [2]. Recently, MRI has been used in inflammatory myopathy for assessing the disease activity, guiding therapeutic decisions and in selecting the appropriate site for a biopsy [14–16]. MRI is not only more sensitive to muscle abnormalities but also can detect clinically unrecognized edema in the skin, subcutaneous tissue and fascia, which is common in the early stages of inflammatory myopathy [9, 15]. In this case, the edema was detected early by MRI and ultrasonography.
This case shows that generalized subcutaneous edema can be a manifestation of DM. Therefore an accurate diagnosis is essential to exclude other etiologies causing edema. Muscle MRI can be used as an additional diagnostic tool to detect subcutaneous edema and monitor its response to therapy. High-dose glucocorticoid is required to treat inflammatory myopathy, particularly in cases presenting with severe generalized edema.
References
Andonopoulos AP, Gogos CA, Tzanakakis G (1993) Subcutaneous edema: an “unrecognized” feature of acute polymyositis. Rheumatol Int 13:159–161
Gorelik O, Almoznino-Sarafian D, Alon I, Rapoport MJ, Goltsman G, Herbert M, Modai D, Cohen N (2001) Acute inflammatory myopathy with severe subcutaneous edema, a new variant? Report of two cases and review of the literature. Rheumatol Int 20:163–166
Karabiber H, Aslan M, Alkan A, Yakinci C (2004) A rare complication of generalized edema in juvenile dermatomyositis: a report of one case. Brain Dev 26:269–272
Lyon-Caen O, Bouche P, Chaunu MP, Duyckaerts C, Vitoux JF (1985) Acute polymyositis with spontaneously regressive subcutaneous edema. Apropos of a case. Rev Neurol (Paris) 141:749–752
Mitchell JP, Dennis GJ, Rider LG (2001) Juvenile dermatomyositis presenting with anasarca: a possible indicator of severe disease activity. J Pediatr 138:942–945
Mroue KH, Sharara NH, Rbeiz JG, Arayssi TK (2003) A case of edematous dermatomyositis. J Rheumatol 30:2722–2723
Nitsche A, San Agustin PG, Amado V, Prina AP, Corsaro G (1988) Trunk and abdominal wall edema in dermatomyositis. Medicina (B Aires) 48:331–332
Sevigny GM, Mathes BM (1999) Periorbital edema as the presenting sign of juvenile dermatomyositis. Pediatr Dermatol 16:43–45
Smyth AE, Bell AL, Crone M (2000) Acute oedematous dermatomyositis. Ann Rheum Dis 59:575
Venables GS, Bates D, Cartlidge NE, Hudgson P (1982) Acute polymyositis with subcutaneous oedema. J Neurol Sci 55:161–164
Werner de Castro GR, Appenzeller S, Bertolo MB, Costallat LT (2006) Acute dermatomyositis with subcutaneous generalized edema. Clin Rheumatol 25:898–900
Dalakas MC, Hohlfeld R (2003) Polymyositis and dermatomyositis. Lancet 362:971–982
Noss EH, Hausner-Sypek DL, Weinblatt ME (2006) Rituximab as therapy for refractory polymyositis and dermatomyositis. J Rheumatol 33:1021–1026
Hernandez RJ, Sullivan DB, Chenevert TL, Keim DR (1993) MR imaging in children with dermatomyositis: musculoskeletal findings and correlation with clinical and laboratory findings. AJR Am J Roentgenol 161:359–366
Reimers CD, Finkenstaedt M (1997) Muscle imaging in inflammatory myopathies. Curr Opin Rheumatol 9:475–485
Park JH, Olsen NJ (2001) Utility of magnetic resonance imaging in the evaluation of patients with inflammatory myopathies. Curr Rheumatol Rep 3:334–345
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, KH., Lim, SR., Kim, YJ. et al. Acute dermatomyositis associated with generalized subcutaneous edema. Rheumatol Int 28, 797–800 (2008). https://doi.org/10.1007/s00296-008-0520-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-008-0520-0