Abstract
To investigate the relationship between ionized calcium and disease activity, parameters of bone metabolism and bone mineral density (BMD) at the lumbar spine (BMD-LS) and the femoral neck (BMD-FN) measured by dual X-ray absorptiometry in rheumatoid arthritis (RA). In 146 patients with RA, the following parameters were investigated: serum levels of ionized calcium, total calcium, vitamin D metabolites 25-hydroxyvitamin D3 (25D3) and 1,25-dihydroxyvitamin D3 (1,25D3), intact parathyroid hormone (iPTH), interleukin-6, osteocalcin, erythrocyte sedimentation rate (ESR) and c-reactive protein (CRP); renal excretion of pyridinolin (PYD)- and desoxypyridinolin (DPD)-crosslinks. A total of 30.1% of the patients were hypercalcemic (ionized calcium >1.30 mmol/l). In comparison with normocalcemic patients, those with hypercalcemia had significantly higher ESR (P<0.01) and CRP values (P<0.05) and significantly lower serum levels of both iPTH (P<0.01) and 1,25D3 (P<0.05) and a significantly lower BMD-LS (P<0.05). The results indicate that a substantial part of RA patients is hypercalcemic. Hypercalcemia is associated with high disease activity and may contribute to suppression of PTH secretion and vitamin D hormone synthesis. High levels of ionized calcium may be a reflection of disease-activity-related systemic bone loss, and could be a predictor of BMD at the lumbar spine in RA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An important mechanism leading to bone loss in rheumatoid arthritis (RA) is increased bone resorption [1–6]. It is well known that increased bone resorption in patients with malignant disease is often associated with hypercalcemia [7]. Production of cytokines and hormones with bone-resorbing properties such as interleukin-6 (IL-6), receptor activator of NFkappaB-ligand (RANKL) and parathormone-related peptide (PTHrP) by malignant cells or the induction of these mediators in bone marrow stromal cells are important mechanisms involved in osteolysis and hypercalcemia in malignant disease [8–13]. Interestingly, the same mediators involved in tumor osteolysis are expressed in activated synovial fibroblasts in RA. The expression of IL-6 [14, 15], PTHrP [16–18] and RANKL [19, 20] has been demonstrated in activated synovial fibroblasts at the pannus invasion front in RA and the pannus infiltrates the adjacent cartilage and bone like a semimalignant tumor [21].
Despite the expression of cytokines stimulating osteoclastogenesis and bone resorption in the rheumatoid synovium, hypercalcemia has not been previously described in RA. However, with respect to the total serum calcium levels in RA, it must be considered that high disease activity in RA is potentially associated with a decrease in hepatic albumin synthesis, resulting in a subsequent decrease in total serum calcium levels because up to 40% of total calcium is bound to albumin [22, 23]. Therefore, the measurement of ionized (“free”) calcium would be a better parameter than total calcium to assess calcium metabolism in RA.
The aim of our study was to investigate serum levels of ionized calcium in RA and the relationship of these with bone mineral density (BMD), disease activity and serum levels of calcium-regulating hormones.
Materials and methods
Patients
We investigated 146 patients with RA (age 18–84 years, mean 58.0±14.5 years) with a mean disease duration of 8.7±9.3 years (0.1–40 years). Eighty-seven patients were postmenopausal women, 28 premenopausal women and 31 men. All patients fulfilled at least four of the 1987 revised ACR criteria for RA [24].
Seventy-four patients (age 20–79 years; mean 58.6±12.4 years) with a mean disease duration of 10.3±8.7 years (0.5–34 years) were receiving glucocorticoid treatment (5–15 mg prednisolone/day), whereas 72 patients (age 18–84 years; mean 59.5±15.5 years) with a mean disease duration of 8.9±9.6 years (0.2–33 years) did not.
Patients gave their written informed consent before participating in the study. The Ethical Committee of the University approved the study design.
Laboratory tests and analytical techniques
The following parameters were investigated in the sera of the patients: erythrocyte sedimentation rate (ESR), c-reactive protein (CRP), interleukin-6 (IL-6), ionized calcium, total calcium, albumin, the vitamin D metabolites 25-hydroxyvitamin D3 (25D3) and 1,25-dihydroxyvitamin D3 (1,25D3), intact parathyroid hormone (iPTH) and osteocalcin (OC). Fasting venous blood samples were drawn between 7 and 9 a.m. For determination of vitamin D metabolites, iPTH and IL-6, serum aliquots were frozen and stored at −70°C until analyzed. Technical details concerning the measuring of calcium-regulating hormones and IL-6 are listed in Table 1.
Furthermore, the excretion of pyridinoline (PYD)- and desoxypyridinoline (DPD)-crosslinks, as well as the calcium/creatinine (u-Ca/crea)-ratio in the morning urine and the daily urinary calcium excretion, were measured.
Pyridinoline and DPD were determined in urine by a reversed-phase HPLC method, described previously by us [25], and expressed as the PYD/creatinine-ratio (PYD/crea) and the DPD/creatinine ratio (DPD/crea), respectively.
Ionized calcium was measured by an ion-selective electrode system (Ionometer EH-F, Fresenius, Schweinfurt, Germany). The normal value of ionized calcium was 1.1–1.3 mmol/l.
Bone mineral density was determined by dual X-ray absorptiometry (DXA, Hologic, Waltham, MA, QDR 4500A) at the lumbar spine (L1–4; BMD-LS) and the femoral neck (BMD-FN).
Statistical analysis
The data were analyzed statistically using the SPSS for Windows Statistical Program. For correlation analysis, we used the Spearman correlation coefficient. To compare the parameters of the various patient groups, first the non-parametric Kruskal–Wallis test was used. If significant differences were detected, the Mann–Whitney U-test was used to compare particular groups. A P<0.05 was considered significant.
Results
Serum levels of ionized calcium in RA
A total of 102 patients (69.9%) had normal serum levels of ionized calcium, whereas 44 patients (30.1%) were hypercalcemic (ionized calcium >1.30 mmol/l). Serum levels of ionized calcium were not different between postmenopausal women (1.28±0.07 mmol/l), premenopausal women (1.27±0.06 mmol/l) and men (1.29±0.05 mmol/l).
Furthermore, no significant differences were observed in the level of ionized calcium between patients with (1.28±0.06 mmol/l) and without glucocorticoid therapy (1.27±0.07 mmol/l). Ionized calcium was not related with age, disease duration and cumulative glucocorticoid dose.
Correlation of ionized calcium with parameters of disease activity and bone metabolism
In the whole group, ionized calcium was significantly positively correlated with ESR and CRP (P<0.01), with total calcium and calcium corrected for albumin (P<0.01) and with the calcium/creatinine ratio in the morning urine (P<0.05; Table 2).
In contrast, ionized calcium was negatively related with the serum levels of both 1,25D3 (P<0.01) and iPTH (P<0.05).
Furthermore, ionized calcium showed a positive correlation with osteocalcin (P<0.05), but was not significantly related with PYD or DPD.
1,25-Dihydroxyvitamin D3 was significantly negatively correlated with both parameters of disease activity ESR, CRP (P<0.001) and IL-6 (P<0.01), and negatively correlated with PYD (P<0.01). 1,25D3 showed positive correlations with iPTH (P<0.01) and u-Ca/crea (P<0.05).
Osteocalcin (P<0.05) and the markers of bone resorption PYD (P<0.001) and DPD (P<0.001) were positively correlated with ESR and CRP.
Serum levels of IL-6 were significantly positively correlated with the markers of bone resorption PYD (P<0.001) and DPD (P<0.01) and showed a negative correlation with iPTH (P<0.05) and total serum calcium (P<0.05).
Serum albumin showed a highly significant negative correlation with ESR, CRP (P<0.001), IL-6 (P<0.01) and with the markers of bone resorption PYD (P<0.001) and DPD (P<0.01) and a positive correlation with 1,25D3 (P<0.001).
Serum levels of ionized calcium, total calcium, albumin and IL-6 according to different CRP levels
Serum levels of total calcium, ionized calcium, albumin and IL-6 in patients with different disease activity according to the CRP level are shown in Fig. 1. Serum levels of total calcium were not influenced by disease activity. In contrast, serum levels of ionized calcium were significantly higher in patients with high disease activity (CRP >60 mg/l; P<0.01) and in patients with CRP 20–60 mg/l (P<0.05) in comparison to those with CRP <20 mg/l. Patients with CRP >60 mg/l had significantly lower albumin levels than patients with lower disease activity (P<0.001). The IL-6 serum levels were significantly higher in patients with CRP >60 mg/l (P<0.001) and in those with CRP 20–60 mg/l (P<0.001) in comparison with patients with low disease activity (CRP <20 mg/l). Furthermore, patients with CRP 20–60 mg/l showed significantly lower IL-6 levels compared with patients with CRP >60 mg/l (P<0.01).
Serum levels of IL-6, ionized calcium (Ca2+), total calcium and albumin according to CRP in 146 patients with RA. Serum levels of IL-6 are significantly increasing with an increase in CRP. Patients with CRP >60 mg/l and CRP 20–60 mg/l showed significantly higher levels of ionized calcium in comparison to those with lower disease activity, whereas the serum levels of total calcium are not different between the patient groups according to CRP. Serum albumin levels in patients with CRP >60 mg/l are significantly lower than in patients with lower disease activity. ***P<0.001; **P<0.01; *P<0.05 vs patients with CRP <20 mg/l; +++P<0.001; ++P<0.01 vs patients with CRP 20–60 mg/l
Influence of glucocorticoid therapy on BMD, parameters of disease activity and bone metabolism
Patients receiving glucocorticoid treatment at the time of the investigation had a significantly longer disease duration (10.3±8.9 vs 6.9±9.5 years; P<0.001), a significantly lower ESR (41±28 vs 54±28 mm/h; P<0.01) and a significantly lower renal excretion of both PYD (90.0±65.0 vs 114.4±62.1 nmol/mmol creatinine; P<0.01) and DPD (14.6±10.0 vs 19.9±10.0 nmol/mmol creatinine; P<0.001) and a significantly higher u-Ca/crea-ratio (0.46±0.26 vs 0.36 vs 0.23; P<0.05) compared with patients not receiving glucocorticoid therapy. Despite a lower BMD-LS (0.81±0.24 vs 0.84±0.15 g/cm2) and BMD-FN (0.71±0.15 vs 0.74±0.15 g/cm2) in patients with glucocorticoid therapy, the differences to those without glucocorticoid treatment were not significant. Serum levels of 25D3, 1,25D3, iPTH, IL-6, osteocalcin, albumin, total calcium and ionized calcium did not differ between patients with and without glucocorticoid therapy.
Differences between hypercalcemic and normocalcemic patients with RA
Hypercalcemic patients showed a significantly lower BMD-LS (P<0.05) and significantly higher values of ESR (P<0.01) and CRP (P<0.05) than normocalcemic patients. Furthermore, hypercalcemic patients were characterized by significantly lower serum levels of both 1,25D3 (P<0.05) and iPTH (P<0.01) in comparison with normocalcemic patients (Fig. 2).
Serum levels of ESR, CRP, 1,25D3, iPTH and BMD-LS in normo- (n=102) and hypercalcemic (n=44) patients with RA (n=146). Hypercalcemic patients had a significantly higher ESR and a significantly higher CRP level than normocalcemic patients and significantly lower levels of both 1,25D3 and iPTH. Furthermore, BMD-LS was significantly lower in hypercalcemic patients in comparison to those with normal values of ionized calcium. **P<0.01; *P<0.05
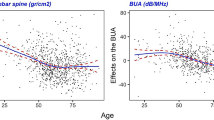
Correlation between BMD at the lumbar spine and femoral neck and parameters of disease activity, bone metabolism, age and disease duration
BMD-LS showed a significant negative correlation with the age of patients (P<0.001) and with serum-ionized calcium, PYD-excretion and ESR (P<0.05).
In contrast, BMD-FN showed no correlation with ionized calcium, but was significantly negatively related to the PYD/DPD-ratio in the morning urine (P<0.001). Furthermore, BMD-FN was negatively correlated with both age (P<0.001) and disease duration (P<0.01) and with the cumulative glucocorticoid dose (P<0.05).
Both BMD-LS and BMD-FN showed no significant correlations with serum levels of IL-6, calcium-regulating hormones or osteocalcin.
Influence of gender and menopausal state on BMD
Postmenopausal women had a significantly lower BMD-LS (0.77±0.22 g/cm2) in comparison with premenopausal women (0.91±0.14 g/cm2; P<0.001) and with men (0.88±0.15 g/cm2; P<0.05) and a significantly lower BMD-FN (0.69±0.16 g/cm2) in comparison with premenopausal women (0.76±0.13 g/cm2; P<0.01) and with men (0.79±0.12 g/cm2; P<0.01).
Discussion
RA is associated with increased bone resorption and the mediators of this process are in part identical with those in malignant disease. Because increased bone resorption in malignant disease is often associated with hypercalcemia, the aim of our study was to measure ionized calcium in RA patients and to investigate the relationship of ionized calcium with BMD, parameters of bone metabolism and disease activity.
One study on bone metabolism in children with chronic rheumatic diseases found no relationship between disease activity and serum levels of ionized calcium [26]. However, this study population consisted of heterogeneous rheumatic diseases including juvenile chronic arthritis, systemic lupus erythematosus and juvenile dermatomyositis, making an interpretation difficult.
The relation between ionized calcium on one hand and other parameters of bone metabolism and BMD in patients with RA on the other was hitherto not investigated.
According to the measured serum levels of ionized calcium, approximately 30% of the investigated RA patients were hypercalcemic. Hypercalcemia was associated with a higher disease activity, lower serum levels of both 1,25D3 and iPTH and a lower BMD-LS. The latter finding was surprising, because calcium deficiency is a risk factor for osteoporosis.
Potential causes and consequences of hypercalcemia in RA patients should be discussed.
The serum calcium level is determined by bone resorption, intestinal calcium absorption and renal calcium reabsorption/excretion [27]. Potentially, the rise of serum-ionized calcium in patients with high disease activity could be explained by an increase in one or more of these processes.
Intestinal calcium absorption is mainly influenced by the 1,25D3 level and action [28, 29]. Low 1,25D3 serum levels were shown to be associated with decreased intestinal calcium absorption [28, 30]. In our patients, 1,25D3 serum levels showed a negative relationship to disease activity, as clearly proved by the negative correlation between 1,25D3 level on one hand and CRP, ESR and IL-6 on the other. This finding is in accordance with the results of a recent study [29]. Because of the positive correlation between ionized calcium and disease activity, the negative relation between 1,25D3 and disease activity and the positive relationship between 1,25D3 and intestinal calcium absorption shown in other studies, an increase of intestinal calcium absorption with increasing disease activity as a cause for the rise of ionized calcium can be excluded.
Renal calcium reabsorption is increased by PTH [27]. Serum levels of ionized calcium showed a positive correlation with the Ca/crea-ratio in the morning urine and the daily urinary calcium excretion was slightly but not significantly higher in hypercalcemic patients than in normocalcemic (data not shown). Therefore, and because iPTH levels in our patients correlated negatively with both disease activity (ESR and IL-6) and ionized calcium, an increase in renal calcium reabsorption as a cause of increasing ionized calcium in patients with high disease activity is unlikely.
A rise in bone resorption with increasing disease activity in our RA patients is clearly proved by the significant positive correlation between PYD/crea and DPD/crea on one hand and ESR, CRP and IL-6 on the other. Principally, the increase in bone resorption in patients with high disease activity could be the main cause of high serum levels of ionized calcium and hypercalcemia in these patients, respectively.
On the other hand, the total serum calcium levels in our patients were not related to disease activity and showed a tendency to fall in patients with high CRP-levels. This discrepancy of the relation between disease activity on one hand and total serum calcium and ionized serum calcium on the other could be explained by the decrease of serum albumin in patients with high disease activity, clearly proved by the highly significant negative correlation of serum albumin with ESR, CRP and IL-6. Because of the albumin binding of a part of the serum calcium, the total serum calcium level is strongly dependent on the serum albumin level and a decrease of serum albumin lowers total serum calcium levels [27]. In contrast, the serum level of ionized calcium is not dependent on serum albumin and ionized calcium in hypocalcemia, which is caused by albumin deficiency, usually remains normal. Therefore, an increased bone resorption leading to an influx of calcium into the blood from the extravessel space in RA patients with high disease activity could induce hypercalcemia measured by high levels of ionized calcium, whereas the serum levels of total calcium are in the low normal or normal range. Proinflammatory cytokines are involved in both the increase in bone resorption and the suppression of hepatic albumin synthesis in RA patients with high disease activity. Thus, the effects of IL-6 are crucial for the inhibition of hepatic albumin synthesis [23, 31]. On the other hand, the activation of the IL-6-system probably plays a central role in bone loss in RA [5, 6, 32–35].
The assumption that the rise of ionized calcium related to increasing disease activity is caused by increased bone turnover and resorption is underlined by the positive correlation between ionized calcium and osteocalcin, as a marker of bone turnover.
Another potential explanation for elevated levels of ionized calcium in patients with high disease activity is a decrease of albumin-bound calcium due to inflammation-associated acidosis [36, 37]. However, a low pH in patients with RA was only detected in the synovial fluid and not in the serum [37]. Therefore, despite serum pH was not measured in our patients an increase of ionized calcium due to acidosis is not likely.
Furthermore, the question is if hypercalcemia influences the secretion of calcium-regulating hormones in patients with high disease activity? Indeed, the decrease of the serum levels of 1,25D3 and iPTH in patients with high disease activity could be in part the consequence of hypercalcemia in these patients. Ionized calcium is one of the negative regulators of PTH secretion, by interaction with the calcium-sensing receptor of the parathyroid gland [38]. A suppression of PTH secretion due to hypercalcemia and a subsequent decrease in the activity of the renal 1-alpha-hydroxylase in patients with high disease activity is in accordance with the finding of higher disease activity and lower iPTH and 1,25D3 levels in hypercalcemic patients and with the positive correlation between iPTH and 1,25D3. In addition, the effects of proinflammatory cytokines could contribute to low levels of 1,25D3 and PTH in patients with high disease activity. It has been shown that nuclear factor kappa B that is induced by TNF-alpha downregulates the promoter of the 1-alpha-hydroxylase [39]. Moreover, the proinflammatory bone-resorbing cytokines IL-1β and IL-6 were shown to inhibit PTH-secretion in vitro [40, 41]. In the case of IL-1β, this inhibition of PTH-secretion was induced by an increase of mRNA of the calcium-sensing receptor [40].
Ionized calcium showed a significant negative correlation with BMD-LS. The finding of lower BMD-LS in hypercalcemic patients in comparison to normocalcemic may reflect an increased systemic bone resorption in patients with high disease activity. This hypothesis is in accordance with various data from RA patients and animal models of this disease that have shown an increase of osteoclastogenesis and of secretion of proinflammatory cytokines with bone-resorbing properties in the bone marrow, suggesting a disease-activity-related systemic bone loss [6, 42–46]. It has been also shown that functional bone resorptive activity of RA-osteoclasts formed from circulating precursors is higher than those of normal controls [47].
Interestingly, an increase in ionized calcium has been shown to induce the secretion of IL-6 in mononuclear blood cells in vitro and in vivo [48]. Because IL-6 is a cytokine with bone-resorbing properties, the stimulation of its secretion by ionized calcium may induce a circulus vitiosus, leading to further bone resorption in chronic inflammatory processes such as RA.
In summary, the results of our study show that a substantial part of RA patients are hypercalcemic and this hypercalcemia may contribute to the suppression of PTH secretion and 1-alpha-hydroxylation of 25D3. Therefore, ionized calcium should be measured to assess calcium metabolism in RA. The increase in ionized calcium in RA patients with high disease activity may reflect systemic effects of proinflammatory cytokines with bone-resorbing properties involved in systemic bone loss. Thus, the results of this study agree with other investigations showing the importance of high disease activity and high bone turnover for systemic bone loss in RA [1, 49–51]. Longitudinal studies would be beneficial to evaluate the importance of ionized calcium as a marker of bone loss in RA.
References
Gough A, Sambrook P, Devlin J, Huisson A, Njeh C, Robbins S, Nguyen T, Emery P (1998) Osteoclastic activation is the principal mechanism leading to secondary osteoporosis in rheumatoid arthritis. J Rheumatol 25:1282–1289
Romas E, Gillespie MT, Martin TJ (2002) Involvement of receptor activator of NfkappaB ligand and tumor necrosis factor-alpha in bone destruction in rheumatoid arthritis. Bone 30:340–346
Shimizu S, Shiozawa S, Shiozawa K, Imura S, Fujita T (1985) Quantitative histologic studies on the pathogenesis of periarticular osteoporosis in rheumatoid arthritis. Arthritis Rheum 28:25–31
Kröger H, Arnala I, Rehnberg V, Hamalainen M, Alhava E (1994) Histomorphometry of periarticular bone in rheumatoid arthritis. Ann Chir Gynaecol 83:56–62
Tanabe M, Ochi T, Tomita T, Suzuki R, Sakata T, Shimaoka Y, Nakagawa S, Ono K (1994) Remarkable elevation of interleukin 6 and interleukin 8 levels in the bone marrow serum of patients with rheumatoid arthritis. J Rheumatol 21:830–835
Toritsuka Y, Nakamura N, Lee SB, Hashimoto J, Yasui N, Shino K, Ochi T (1997) Osteoclastogenesis in iliac bone marrow of patients with rheumatoid arthritis. J Rheumatol 24:1690–1696
Guise TA, Kozlow WM, Heras-Herzig A, Padalecki SS, Yin JJ, Chirgwin JM (2005) Molecular mechanisms of breast cancer metastases to bone. Clin Breast Cancer 5(Suppl 2):46–53
Roux S, Mariette X (2004) The high rate of bone resorption in multiple myeloma is due to RANK (receptor activator of nuclear factor-kappaB) and RANK ligand expression. Leukoc Lymphoma 45:1111–1118
Lai FP, Cole-Sinclair M, Cheng WJ, Quinn JM, Gillespie MT, Sentry JW, Schneider HG (2004) Myeloma cells can directly contribute to the pool of RANKL in bone bypassing the classic stromal and osteoblast pathway of osteoclast stimulation. Br J Haematol 126:192–201
Giuliani N, Colla S, Morandi F, Rizzoli V (2004) The RANK/RANK ligand system is involved in interleukin-6 and interleukin-11 upregulation by human myeloma cells in the bone marrow microenvironment. Haematologica 89:1118–1123
Bendre M, Gaddy D, Nicholas RW, Suva LJ (2003) Breast cancer metastasis to bone: it is not all about PTHrP. Clin Orthop Relat Res 415(Suppl):39–45
Barton BE (2005) Interleukin-6 and new strategies for the treatment of cancer, hyperproliferative diseases and paraneoplastic syndromes. Expert Opin Ther Targets 9:737–752
Abe M, Hiura K, Wilde J, Shioyasono A, Moriyama K, Hashimoto T, Kido S, Oshima T, Shibata H, Ozaki S, Inoue D, Matsumoto T (2004) Osteoclasts enhance myeloma cell growth and survival via cell–cell contact: a vicious cycle between bone destruction and myeloma expansion. Blood 104:2484–2491
Miyazawa K, Mori A, Yamamoto K, Okudaira H (1998) Constitutive transcription of the human interleukin-6 gene by rheumatoid synoviocytes: spontaneous activation of NF-kappaB and CBF1. Am J Pathol 152:793–803
Sung JY, Hong JH, Kang HS, Choi I, Lim SD, Lee JK, Seok JH, Lee JH, Hur GM (2000) Methotrexate suppresses the interleukin-6 induced generation of reactive oxygen species in the synoviocytes of rheumatoid arthritis. Immunopharmacology 47:35–44
Kohno H, Shigeno C, Kasai R, Akiyama H, Iida H, Tsuboyama T, Sato K, Konishi J, Nakamura T (1997) Synovial fluids from patients with osteoarthritis and rheumatoid arthritis contain high levels of parathyroid hormone-related peptide. J Bone Miner Res 12:847–854
Funk JL, Cordaro LA, Wie H, Benjamin JB, Yocum DE (1998) Synovium as a source of increased amino-terminal parathyroid hormone-related protein expression in rheumatoid arthritis. A possible role for locally produced parathyroid hormone-related protein in the pathogenesis of rheumatoid arthritis. J Clin Invest 101:1362–1371
Horiuchi T, Yoshida T, Koshihara Y, Sakamoto H, Kanai H, Yamamoto S, Ito H (1999) The increase of parathyroid hormone-related peptide and cytokine levels in synovial fluid of elderly rheumatoid arthritis and osteoarthritis. Endocr J 46:643–649
Hofbauer LC, Khosla S, Dunstan CR, Lacey DL, Boyle WJ, Riggs BL (2000) The roles of osteoprotegerin and osteoprotegerin ligand in the paracrine regulation of bone resorption. J Bone Miner Res 15:2–12
Gravallese EM, Manning C, Tsay A, Naito A, Pan C, Amento E, Goldring SR (2000) Synovial tissue in rheumatoid arthritis is a source of osteoclast differentiation factor. Arthritis Rheum 43:250–258
Meinecke I, Rutkauskaite E, Gay S, Pap T (2005) The role of synovial fibroblasts in mediating joint destruction in rheumatoid arthritis. Curr Pharm Des 11:563–568
Niwa Y, Iio A, Niwa G, Sakane T, Tsunematsu T, Kanoh T (1990) Serum albumin metabolism in rheumatic diseases: relationship to corticosteroids and peptic ulcer. J Clin Lab Immunol 31:11–16
Huang Y, Shinzawa H, Togashi H, Takahashi T, Kuzumaki T, Otsu K, Ishikawa K (1995) Interleukin-6 down-regulates expressions of the aldolase B and albumin genes through a pathway involving the activation of tyrosine kinase. Arch Biochem Biophys 320:203–209
Arnett FC, Edworthy SM, Bloch DA (1988) The American Rheumatism Association 1987 revised criteria for classification of rheumatoid arthritis. Arthritis Rheum 31:315–324
Müller A, Hein G, Franke S, Herrmann D, Henzgen S, Roth A, Stein G (1996) Quantitative analysis of pyridinium crosslinks of collagen in the synovial fluid of patients with rheumatoid arthritis using high-performance liquid chromatography. Rheumatol Int 16:23–28
Reed A, Haugen M, Pachmann LM, Langman CB (1990) Abnormilities in serum osteocalcin values in children with chronic rheumatic diseases. J Pediatr 116:574–580
Broadus AE, Silverberg SJ, Lemann J Jr (1993) Calcium, magnesium and phosphorus homeostasis. In: Favus MJ (ed) Primer on the metabolic bone diseases and disorders of mineral metabolism. Raven Press, New York, NY, pp 29–39
Need AG, Morris HA, Horowitz M, Scopacasa E, Nordin BE (1998) Intestinal calcium absorption in men with spinal osteoporosis. Clin Endocrinol 48:163–168
Oelzner P, Müller A, Deschner F, Hüller M, Abendroth K, Hein G, Stein G (1998) Relationship between disease activity and serum levels of vitamin D metabolites and PTH in rheumatoid arthritis. Calcif Tissue Int 62:193–198
Morris HA, Need AG, O’Loughlin PD, Horowitz M, Bridges A, Nordin BE (1990) Malabsorption of calcium in corticosteroid-induced osteoporosis. Calcif Tissue Int 46:305–308
Bauer J, Lengyel G, Thung SN, Jonas U, Gerok W, Acs G (1991) Human fetal hepatocytes respond to inflammatory mediators and excrete bile. Hepatology 13:1131–1141
Kotake S, Sato K, Kim KJ, Takahashi N, Udagawa N, Nakamura I, Yamaguchi A, Kishimoto T, Suda T, Kashiwazaki S (1996) Interleukin-6 and soluble interleukin-6 receptors in the synovial fluids from rheumatoid arthritis patients are responsible for osteoclast-like cell formation. J Bone Miner Res 11:88–95
Hayashida K, Ochi T, Fujimoto M, Owaki H, Shimaoka Y, Ono K, Matsumoto K (1992) Bone marrow changes in adjuvant-induced and collagen-induced arthritis. Interleukin-1 and interleukin-6 activity and abnormal myelopoiesis. Arthritis Rheum 35:241–245
Suzuki Y, Tanihara M, Ichikawa Y, Osanai A, Nakagawa M, Ide M, Mizushima Y (1995) Periarticular osteopenia in adjuvant induced arthritis: role of interleukin-1 in decreased osteogenic and increased resorptive potential of bone marrow cells. Ann Rheum Dis 54:484–490
Sugiyama T (2001) Involvement of interleukin-6 and prostaglandin E2 in periarticular osteoporosis of postmenopausal women with rheumatoid arthritis. J Bone Miner Metab 19:89–96
Toffaletti J, Abrams B (1989) Effects of in vivo and in vitro production of lactic acid on ionized, protein-bound, and complex-bound calcium in blood. Clin Chem 35:935–938
Farr M, Garvey K, Bold AM, Kendall MJ, Bacon PA (1985) Significance of the hydrogen ion concentration in synovial fluid in rheumatoid arthritis. Clin Exp Rheumatol 3:99–104
Chen RA, Goodman WG (2004) Role of calcium-sensing receptor in parathyroid gland physiology. Am J Physiol Renal Physiol 286:1005–1011
Ebert R, Jovanovic M, Ulmer M, Schneider D, Meissner-Weigl J, Adamski J, Jakob F (2004) Down-regulation by nuclear factor kappaB of human 25-hydroxyvitamin D3 1 alpha-hydroxylase promoter. Mol Endocrinol 18:2440–2450
Nielsen PK, Rasmussen AK, Butters R, Feldt-Rasmussen U, Bendtzen K, Diaz R, Brown EM, Olgaard K (1997) Inhibition of PTH secretion by interleukin-1 beta in bovine parathyroid glands in vitro is associated with an up-regulation of the calcium-sensing receptor mRNA. Biochem Biophys Res Commun 238:880–885
Carlstedt E, Ridefelt P, Lind L, Rastad J (1999) Interleukin-6 induced suppression of bovine parathyroid hormone secretion. Biosci Rep 19:35–42
Kotake S, Higaki M, Sato K, Himeno S, Morita H, Kim KJ, Nara N, Miyasaka N, Nishioka K, Kashiwazaki S (1992) Detection of myeloid precursors (granulocyte/macrophage colony forming units) in the bone marrow adjacent to rheumatoid arthritis joints. J Rheumatol 19:1511–1516
Fujikawa Y, Sabokbar A, Neale S, Athanasou NA (1996) Human osteoclast formation and bone resorption by monocytes and synovial macrophages in rheumatoid arthritis. Ann Rheum Dis 55:816–822
Hirohata S, Yanagida T, Itoh K, Nakamura H, Yoshino S, Tomita T, Ochi T (1996) Accelerated generation of CD14+ monocyte-lineage cells from the bone marrow of rheumatoid arthritis patients. Arthritis Rheum 39:836–843
Schulze-Koops H, Davis LS, Kavanaugh AF, Lipsky PE (1997) Elevated cytokine messenger RNA levels in the peripheral blood of patients with rheumatoid arthritis suggest different degrees of myeloid cell activation. Arthritis Rheum 40:639–647
Suzuki Y, Nishikaku F, Nakatuka M, Koga Y (1998) Osteoclast-like cells in murine collagen induced arthritis. J Rheumatol 25:1154–1160
Hirayama T, Danks L, Sabokbar A, Athanasou NA (2002) Osteoclast formation and activity in the pathogenesis of osteoporosis in rheumatoid arthritis. Rheumatology 41:1232–1239
Bornefalk E, Ljunghall S, Lindh E, Bengtson O, Johansson AG, Ljunggren O (1997) Regulation of interleukin-6 secretion from mononuclear blood cells by extracellular calcium. J Bone Miner Res 12:228–233
Reeve J, Loftus J, Hesp R, Ansell BM, Wright DJ, Woo PM (1993) Biochemical prediction of changes in spinal bone mass in juvenile chronic (or rheumatoid) arthritis treated with glucocorticoids. J Rheumatol 20:1189–1195
Cortet B, Flipo RM, Pigny P, Duquesnoy B, Boersma A, Marchandise X, Delcambre B (1998) Is bone turnover a determinant of bone mass in rheumatoid arthritis. J Rheumatol 25:2339–2344
Cortet B, Guyot MH, Solau E, Pigny P, Dumoulin F, Flipo RM, Marchandise X, Delcambre B (2000) Factors influencing bone loss in rheumatoid arthritis: a longitudinal study. Clin Exp Rheumatol 18:683–690
Acknowledgement
This work was supported by the Thuringian Ministry of Science, Research and Art (FKZ B307-01025).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oelzner, P., Lehmann, G., Eidner, T. et al. Hypercalcemia in rheumatoid arthritis: relationship with disease activity and bone metabolism. Rheumatol Int 26, 908–915 (2006). https://doi.org/10.1007/s00296-005-0095-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-005-0095-y