Abstract
Background: Myofascial pain syndrome (MPS) is one of the most common causes of chronic musculoskeletal pain. Several methods have been recommended for the inactivation of trigger points (TrP). Objectives: This prospective, single-blind study was proposed to compare TrP injection with botulinum toxin type A (BTX-A) to dry needling and lidocaine injection in MPS. Methods: Eighty-seven trigger points (cervical and/or periscapular regions) in 23 female and six male patients with MPS were treated and randomly assigned to three groups: lidocaine injection (n=10, 32 TrP), dry needling (n=10, 33 TrP), and BTX-A injection (n=9, 22 TrP). Outcome measures: Clinical assessment including cervical range of motion, TrP pain pressure threshold (PPT), pain scores (PS), and visual analog scales for pain, fatigue, and work disability were evaluated at entry and the end of the 4th week. Additionally, depression and anxiety were evaluated with the Hamilton depression and anxiety rating scales, and quality of life was assessed using the Nottingham health profile (NHP). The subjects were also asked to describe side effects. Injection procedure: One milliliter of 0.5% lidocaine was administered to each TrP in the lidocaine injection group, 10–20 IU of BTX-A to each TrP in the BTX-A group, and dry needling to each TrP in the last group, followed by stretching of the muscle groups involved. The patients were instructed to continue their home exercise programs. Results: Pain pressure thresholds and PS significantly improved in all three groups. In the lidocaine group, PPT values were significantly higher than in the dry needle group, and PS were significantly lower than in both the BTX-A and dry needle groups. In all, visual analog scores significantly decreased in the lidocaine injection and BTX-A groups and did not significantly change in the dry needle group. Disturbance during the injection procedure was lowest in the lidocaine injection group. Quality of life scores assessed by NHP significantly improved in the lidocaine and BTX-A groups but not in the dry needle group. Depression and anxiety scores significantly improved only in the BTX-A-injected group. Conclusions: Injection is more practical and rapid, since it causes less disturbance than dry needling and is more cost effective than BTX-A injection, and seems the treatment of choice in MPS. On the other hand, BTX-A could be selectively used in MPS patients resistant to conventional treatments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myofascial pain syndrome (MPS) is a regional muscular pain syndrome characterized by the presence of hypersensitive points called “trigger points” (TrP) in one or more muscles and/or connective tissue. In addition to the TrP, this regionally painful clinical problem presents with muscular spasm, stretching of muscular fibers, band-type tissue stiffness, stiffening and limitation of articular motion, loss of strength, and autonomic dysfunction. The pain can be felt locally at the TrP sites or at distant areas through reflection. Myofascial pain syndrome is the dominating cause of muscular disability at shoulder girdle, neck, and lumbar regions [1].
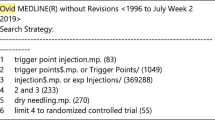
Several methods have been recommended for the inactivation of TrP. The treatments most commonly utilized for this purpose are dry needling of the TrP, injection treatments with local anesthetics or saline, sprays, and stretching. According to the results of several studies on many patients, injection continues to be the most effective choice for treatment [2, 3, 4, 5, 6, 7, 8]. Preventing the development of new TrP necessitates controlling all the factors that influence the initiation and continuation of chronic pain, as well as carrying out exercise programs [1, 9]. Although the superiority of local injection or dry needling for the inactivation of TrP is controversial, both have shown similar therapeutic efficacy [5, 9, 10, 11]. Botulinum toxin (BTX) injections have been shown to be safe and efficacious for the treatment of several neurologic and non-neurologic diseases. Controversial results are being reported concerning their use for the treatment of MPS [2, 12, 13, 14, 15, 16]. This prospective, single-blind study compares TrP injection with botulinum toxin type A (BTX-A) with dry needling and lidocaine injection in MPS.
Materials and method
Patients
Twenty-nine patients (23 female, six male) admitted to the Department of Physical Medicine and Rehabilitation of our institution with at least one TrP located on cervical, back, or shoulder muscles (upper, lower, and middle trapezius, levator scapula, teres minor, supraspinatus, infraspinatus), with disease of at least 6-month duration and not receiving any treatment during the previous 8 weeks, were recruited in this study. For comparison with the contralateral side of the body, special attention was paid to patients with myofascial pain on only one side. The patients were randomized into three groups: lidocaine injection (LIG) (n=10, 32 TrP), dry needling (DNG) (n=10, 33 TrP), and BTX-A injection (BTIG) (n=9, 22 TrP).
We did not include patients with cardiovascular or respiratory disease, allergies, with injections to TrP within the last 2 months, having undergone cervical or shoulder surgery within the last year, diagnosed with fibromyalgia syndrome, cervical radiculopathy, myelopathy with severe disc or skeletal lesions, or did not cooperate well. Furthermore, patients using aminoglycosides or other medications preventing neuromuscular transmission, with motor neuron diseases or diseases affecting neuromuscular junctions, or who had possible pregnancy were also not included.
Measurements
The diagnosis of active myofascial TrP was based upon criteria described by Travell and Simons: tender spots in one or more palpable taut bands, a typical pattern of referred pain, palpable or visible local twitch responses on snapping palpation at the most sensitive spot in the taut band, and restricted range of motion (ROM) in lateral bending of the cervical spine to the opposite side [8, 9, 17]. The measurements were obtained before treatment (BT) and 1 month after treatment for the evaluation of therapeutic efficacy and side effects. Cervical ROM was measured with goniometry, as was ROM in the opposite direction of the muscle containing TrP [11, 18].
Pressure pain threshold (PPT) measurements were performed with an algometry device by placing the plastic tip on the TrP. Pressure was increased by 1 kg/s, and the pressure value at which the patient felt the first discomfort was recorded in kg. The same region was assessed twice at 1-min intervals [19, 20, 21, 22, 23]. To compare PPT values on affected sides with those on the healthy sides, measurements were obtained from points exactly symmetrical to the TrP.
Pain score (PS) measurements were obtained by placing the thumb to the skin covering the muscle containing the TrP in a perpendicular fashion and exerting pressure until there was whitening of the nail bed and then evaluating the pain intensity. Scoring was from 0 to 3 (0 no pain, 1 mild pain, 2 significant pain, and 3 severe pain resulting in jumping sign).
Subjective complaints of pain, fatigue, and work disability were measured using a visual analog scale (VAS) between 0 and 10. For measurement of the pain-related disability score, Nottingham Health Profile (NHP) assessments were done before and after treatment. For the evaluation of pain-related anxiety and depression, a psychiatrist who was not informed about the grouping of the patients helped them to fill out the Hamilton Anxiety and Depression Inventory.
Dry needling and local anesthetic injection
Lidocaine injection and dry needling of TrP was performed by the modification of techniques recommended by Travell and Simons [8, 9, 11, 17]. The patients were asked to lie down in prone position. Injections were done with 25-gauge needles 1.25 in long. The stretched band, that was localized between the thumb and the index finger, was entered rapidly, having the tip of the needle perpendicular to the skin. The needle was inserted into the muscle until the exact TrP was reached. After injecting 1 ml of 0.5% lidocaine solution, the needle was moved backward and forward, and the same point was needled eight to ten times. Then the tip was withdrawn to the subcutaneous tissue, the injector was mildly inclined, and the sides and upper and lower parts of the first injection site were needled. Thus we tried to inactivate satellite TrPs that might cause pain [11, 14, 17, 18, 24, 25]. The same procedures were applied with empty syringes to the patients in the dry needling group.
Botulinum toxin injection
In this group, each TrP was injected with a single dose of BTX-A of 10–20 IU (10 IU in 1 ml). The needle penetration was same as with dry needling and local anesthetic injection. Afterwards, 1–2 ml of BTX solution was injected and the needle was retrieved. For establishing hemostasis in all the groups following injection, compression was applied for 2 min to the injection sites. Then the muscles were lengthened with passive stretching. After the injection procedures, the patients were questioned on discomfort during the injection. Following the treatment, all patients were given home exercise programs. The postural habits at home and work were investigated and, if deficient, the patients were informed on prevention.
Data analysis
Definitive statistical techniques were applied to the anthropometric and demographic information in all groups. For measurements with ordinal variables, the chi-squared test was used. For intragroup comparisons, Wilcoxon’s signed rank test was used, and for comparisons between groups, one-way analysis of variance was applied and evaluated by post hoc test. For multiple comparisons, the 0.05 significance limit divided among three comparisons was 0.016. For other comparisons, significance was accepted at 0.05.
Results
The age, duration of pain, number and localizations of TrP on the affected body half, and average body mass indices grouped according to treatment type are presented in Table 1. There was no significant difference between the groups concerning these features. Of the 87 TrP included in treatment, 27 were localized on the trapezius muscle (nine LIG, ten DNG, eight BTIG).
Lidocaine injection
Comparison of the results before and at the end of the 1st month after lidocaine injection are presented in Table 2. In the LIG, subjective pain, fatigue, and work disability measured by VAS showed significant decreases (P<0.05). When compared with preinjection values, PPT showed significant increases (P<0.001) in the 1st postinjection month. Pain pressure threshold and PS values of the body points symmetrical to the TrP did not show any significant change in the 1st postinjection month (P>0.05). The NHP showed significant reduction in the 1st postinjection month, whereas the Hamilton depression and anxiety scales did not show any significant change (P>0.05). Cervical ROM values in the LIG showed significant changes in the 1st postinjection month (P<0.05).
Dry needling
The comparison of results before and 1 month after dry needling is presented in Table 3. When compared with pretreatment values, PPT showed a significant increase (P<0.05) and PS a significant decrease (P<0.05). At the end of the 1st month after treatment, PPT values of the body points symmetrical with the TrP showed a significant increase, whereas PS values showed a significant decrease. Subjective pain, fatigue, and work disability on VAS, NHP, and Hamilton depression and anxiety scores did not show any significant change (P>0.05). There was a significant increase in cervical ROM values 1 month after treatment (P<0.05).
Botulinum toxin injection
Comparison of the results obtained before and at the end of the 1st month after BTX-A injection are presented in Table 4. The PPT showed a significant increase (P<0.05) and PS a significant decrease (P<0.05). After 1 month, PPT values of the points symmetrical with the TrP showed significant improvement (P<0.05), while PS values did not demonstrate any significant change (P>0.05). Subjective pain, fatigue, and work disability measured by VAS showed significant reductions (P<0.05). After the treatment, NHP and Hamilton depression and anxiety scores showed significant decreases (P<0.05). Cervical ROM had a significant increase end of the 1st month after treatment (P<0.05).
Comparison of treatment results of the lidocaine injection, dry needling, and botulinum toxin groups
The P values obtained after comparing pre- and post-treatment values of the LIG, DNG, and BTIG within the groups and between group pairs are presented in Table 5.
For PPT values at TrP, there was no significant pretreatment difference between the groups (P>0.05) but a significant difference post treatment (P<0.05). A significant difference in TrP PPT values at the end of the 1st month after treatment was observed between LIG and DNG (P<0.016) but not between LIG and BTIG or between DNG and BTIG (P>0.016). The PPT values at the symmetrical points pretreatment and 1 month after treatment did not demonstrate a significant difference between groups (P>0.05). When pretreatment PS values of TrP were compared, there was a significant difference (P<0.05) between LIG and BTIG (P<0.016). When PS values of TrP were compared after 1-month treatment, there was a significant difference between LIG and DNG as well as between LIG and BTIG in favor of lidocaine injection (P<0.016).
At the end of the 1st month after treatment, comparison of subjective pain, fatigue, and work disability by VAS showed a significant difference (P<0.05). When pain VAS after treatment was compared among the three groups, there was more improvement seen in favor of LIG and BTIG. For VAS fatigue scores 1 month post treatment, LIG showed better values than DNG (P<0.016).
The side effects exerted by the three treatments were: coldness and burning sensation at the treatment site in 30% (three patients) and paresthesia in 30% (three) of LIG patients, fatigue in 55.6% (five), muscle pain in 33.3% (three), and headache in 10% (one) of the BTIG. However, these side effects did not last more than a few days. Discomfort at the time of injection was felt by 80% (eight) DNG patients and 20% (two) in the LIG. In the BTIG, there was no discomfort at the time of injection.
Discussion
Myofascial pain syndrome involves regional muscular pain characterized by localized muscular sensitivity. It might be responsible for the unidentified causes of pain observed at different locations in patients. Prevention of the erroneous diagnoses and inappropriate therapeutic approaches that are frequently done in MPS patients will reduce the problems of work loss and inappropriate treatment costs [26, 27, 28].
A multidisciplinary approach is recommended in chronic MPS, as the pain has a complex nature [29]. The mainstream of treatment is to break down the vicious cycle of pain through the elimination of TrPs. There are different approaches for the treatment of MPS [1, 8, 9, 26, 30].
In our study, we aimed to investigate the differences between efficacies of local injection of lidocaine and dry needling, that are commonly used in practice, and low-dose injections of BTX by comparing the results after 1 month of treatment with pretreatment values.
Some studies indicate that the efficacy of injections to the TrP was related to reflex mechanisms rather than pharmacologic effects of the solutions [5, 31, 32, 33]. To determine whether the effect obtained by TrP injection was related to the pharmaceutic agent, we used dry needling as a control. This study differs from many others in that it utilizes a comprehensive control group for measuring results [2, 5, 12, 16, 34].
In our study, injection of local anesthetics, treatment with dry needling, and the injection of BTX had therapeutic efficacies of different degrees in the TrPs of all patients. This effect was observed objectively as increased cervical ROM and PPT in the muscles containing TrPs and subjectively as significantly increased VAS (Table 2, Table 3, Table 4). The cervical ROM values of all three groups showed significant increase with treatment. After treatment, variables such as pain, fatigue, and work disability as measured by VAS showed a significant decrease in the LIG and BTIG (P<0.05) but not the DNG (P>0.05).
In order to have controls for PPT and VAS values obtained from TrP, we chose patients with unilateral MPS in our study. Before and after the treatment, PPT and VAS measurements were obtained from points on the contralateral sides which were symmetrical with the TrP. Thus, in the muscles with TrP, sensitivity was objectively and subjectively higher than in the unaffected muscles. With treatment, PPT measurements of the symmetric points of the DNG and BTIG showed significant increase, while symmetric point VAS values of the DNG showed a significant decrease. This positive effect obtained by treatment at the symmetrical points of the contralateral sides might be related to the decrease in sensitivity of the TrP and a general reduction in pain through diminishment of aggravating factors such as postural problems by stretching and strengthening exercises.
It has frequently been mentioned that patients suffering from myofascial pain for long periods might develop anxiety and depression [3, 28, 35, 36, 37, 38]. In our study, Hamilton depression and anxiety scores showed significant improvements in the BTIG (P<0.05), whereas there was no such improvement in the LIG or DNG (P>0.05). The lack of a significant decrease after treatment might be due to the fact that the scores were relatively low and in accordance with mild-to-moderate anxiety and depression before treatment. In intergroup comparison after the treatment, there was no difference between groups concerning improvement in Hamilton depression and anxiety scores (P>0.05). In intragroup comparison, there was significant improvement in NHP scores in the LIG and BTIG but not in the DNG (P>0.05).
Concerning the therapeutic effect on TrP, all the variables measured by VAS and disability scores showed no significant difference between lidocaine and BTX injection. However, when compared with dry needling, lidocaine injection was more effective than BTX.
Wheeler et al. reported side effects (increased pain and muscle spasm, mild loss of strength and heaviness in the ipsilateral arm, headache, irritability, increased cervical pain, and weakness of the eye and face) observed in 12 patients (27.3%) following the first injection. They reported that side effects were seen in only two (8.3%) patients after the second injection and in none after the third injection. Moreover, these side effects were reported to have resolved within 1–2 weeks [14]. In another study, none of the patients injected with BTX was reported to have a persisting side effect [2]. In our study, we observed fatigue, muscle pain, and short-term headache as side effects in the BTIG. The most commonly observed side effect was fatigue (55.6%), followed by muscle pain (33.3%). However, none of these side effects lasted more than a few days.
In previous studies, dry needling of TrP was reported to be as effective as local anesthetics in the inactivation of TrP. However, the injection of TrP with local anesthetics was more comforting than dry needling [5, 22]. Hong et al. reported that dry needling or injection of TrP with 0.5% lidocaine decreased the myofascial pain effectively, increased the threshold of pain in TrP, and increased ROM of the treated muscles; during dry needling, there was a significant sensation of pain which could last up to 1 week [5].
In our study, during and after the injection of lidocaine, the discomfort was found to be significantly low. Pain was felt by 80% of the patients during the time of injection in the DNG, whereas it was present in only 20% of the LIG. The utilization of local anesthetics in TrP injections might decrease the sensation of discomfort [32]. This can be explained by local anesthetics’ lengthening the relative refractory period of the peripheral nerves and limiting the maximum frequency of impulse conduction. The use of local anesthetics in TrP injections decreases pain in the initial period, thereby providing confidence in the physician and compliance with exercise programs.
For the treatment of disseminated pain syndromes, there is controversy in the literature concerning the potential efficacy of BTX-A [12, 13]. In our study, the effects of single-dose injection of BTX on TrP were not different than with dry needling. However, in a study by Cheshire et al. performed in 1994 on patients with MPS, saline injection was used in the control group, and single doses of BTX were reported to be more effective [12].
Currently, as the primary effect of BTX is muscular relaxation, it is advantageous to traditional treatment approaches and has a longer effect [2]. Wheeler et al. reported reduced pain in 80% of patients following the first injection of BTX and stated that a single dose was sufficient in 41%, while 32% required second doses and 27% required repetitive doses [14]. For longer duration of the effect of BTX treatment, multiple injections are required and thus the cost increases. For this reason, BTX will not be the first choice for treating MPS. In order to reduce the cost of treatment and show its efficacy in MPS, we utilized BTX in single, low-dose injections.
In another study by Wheeler et al. on the therapeutic efficacy in MPS (PPT, cervical pain, and a disability scale were used), the injection of single doses of BTX was not reported superior to normal saline injection [13]. However, in our study, BTX was found to be superior to dry needling, according to VAS values.
Our study indicates that, to increase efficacy, the injections should be complemented with a strict physical therapy program rather than repeating the injections [14, 16]. The major potential advantage of BTX in the treatment of MPS is the possibility of lasting therapeutic efficacy when combined with physical therapy. Wheeler and Goolkasian demonstrated that, when utilized together with physical therapy, BTX can be an effective treatment for patients with chronic cervical pain. However, theirs were only preliminary studies aiming at evaluating the therapeutic efficacy of BTX-A. Cheshire et al. compared the effects of BTX-A treatment with those of saline injections and reported a mild improvement with BTX-A [12]. When Wheeler et al. evaluated patients receiving BTX-A treatment alone, they arrived at the conclusion that physical therapy was a required additional element, both before and after injections, and important in lengthening the pain reduction [13]. The efficacy of stretching exercises and home programs has been proven by many studies in MPS [17, 39, 40]. In our study, a physician applied stretching to the TrP of all the patients, and all were instructed on home exercises.
In conclusion, the therapeutic efficacy on the TrP in all three groups was found to be significant, according to the results of this study. In the intergroup comparison, lidocaine injection increased PPT values more than dry needling. Botulinum toxin and lidocaine injections both had significant effects on VAS values such as pain, fatigue, and work disability, but this efficacy was more prominent with lidocaine. Although dry needling did not have any therapeutic efficacy on disability, lidocaine and BTX injections had effects of significant degree. Lidocaine injection and dry needling were not efficacious in depression and anxiety scores, whereas BTX was more effective.
According to the results of this study, we think that the decision for injection should include a local anesthetic such as lidocaine rather than dry needling because of its practical and rapid application, which results in lower sensitivity. Low-dose injections of BTX should not be the first choice, due to higher cost and discomfort, and should be left as a choice for chronic MPS patients who are resistant to conventional treatments.
References
Sola AE, Bonica JJ (1990) Myofascial pain syndromes. In: Bonica JJ (ed) The management of pain. Lea and Febiger, Philadelphia, pp 352–367
Alo KM, Yland MJ, Kramer DL, Charnov JH, Redko V (1997) Botulinum toxin in the treatment of myofascial pain. The Pain Clinic 10:107–116
Esenyel M, Çaglar N, Aldemir T (2000) Treatment of myofascial pain. Am J Phys Med Rehabil 79:48–52
Flor H, Birbaumer N (1993) Comparison of the efficacy of electromyographic biofeedback, cognitive-behavioral therapy, and conservative medical interventions in the treatment of chronic musculoskeletal pain. J Consult Clin Psychol 61:653–658
Hong CZ (1994) Lidocaine injection versus dry needling to myofascial trigger point. Importance of the local twitch response. Am J Phys Med Rehabil 73:256–263
Janzen VD, Scudds R (1997) Sphenopalatine blocks in the treatment of pain in fibromyalgia and myofascial pain syndrome. Laryngoscope 107:1420–1422
Scudds RA, Janzen V, Delaney G, Heck C, McCain GA, Russell AL, Teasel RW, Varkey G, Woodbury MG (1995) The use of topical 4% lidocaine in spheno-palatine ganglion blocks for the treatment of chronic muscle pain syndromes: a randomized, controlled trial. Pain 62:69–77
Travell JG, Simons DG (1992) Myofascial pain and dysfunction: the trigger point manual. Williams and Wilkins, Baltimore
Simons DG (1988) Myofascial pain syndrome due to trigger points. In: Goodgold J (ed) Rehabilitation medicine. Mosby, St. Louis, pp 686–723
Fricton JR (1994) Myofascial pain. Baillieres Clin Rheumatol 8:858–880
Yunus MB, Kalyan-Raman UP (1989) Muscle biopsy findings in primary fibromyalgia and other forms of nonarticular rheumatism. Rheum Dis Clin North Am 15:115–134
Cheshire WP, Abashian SW, Mann JD (1994) Botulinum toxin in the treatment of myofascial pain syndrome. Pain 59:65–69
Wheeler AH, Goolkasian P, Gretz SS (2001) Botulinum toxin A for the treatment of chronic neck pain. Pain 94:255–260
Wheeler AH, Goolkasian P (2001) Open label assessment of botulinum toxin A for pain treatment in a private outpatient setting. J Musculoskelet Pain 9:67–82
Wheeler AH, Goolkasian P, Gretz SS (1998) A randomized, double-blind, prospective pilot study of botulinum toxin for refractory, unilateral, cervicothoracic, paraspinal, myofascial pain syndrome. Spine 23:1662–1667
Porta M (2000) A comparative trial of botulinum toxin type A and methylprednisolone for the treatment of myofascial pain syndrome and pain from chronic muscle spasm. Pain 85:101–105
Rosen NB (1994) Physical medicine and rehabilitation approaches to the management of myofascial pain and fibromyalgia syndromes. Baillieres Clin Rheumatol 8:881–916
Hong CZ, Hsueh TC (1996) Difference in pain relief after trigger point injections in myofascial pain patients with and without fibromyalgia. Arch Phys Med Rehabil 77:1161–1166
Fischer AA (1986) Pressure threshold meter: its use for quantification of tender spots. Arch Phys Med Rehabil 67:836–838
Fischer AA (1987) Pressure algometry over normal muscles. Standard values, validity and reproducibility of pressure threshold. Pain 30:115–126
Esenyel M, Çaglar N, Aldemir T (2000) Treatment of myofascial pain. Am J Phys Med Rehabil 79:48–52
Reeves JL, Jaeger B, Graff-Redford SB (1986) Reliability of the pressure algometer as a measure of myofascial trigger point sensitivity. Pain 24:313–321
Ozgocmen S, Ardicoglu O (2000) Lipid profile in patients with primary fibromyalgia and myofascial pain syndromes. Yonsei Med J 41:541–545
Durett MR, Rodriguez AA, Agre JC, Silverman JL (1991) Needle electromyographic evaluation of patients with myofascial or fibromyalgic pain. Am J Phys Med Rehabil 70:154–156
Hong CZ, Kuan TS, Chen JT, Chen SM (1997) Referred pain elicited by palpation and by needling of myofascial trigger points: a comparison. Arch Phys Med Rehabil 78:957–960
Berker E (1997) Miyofasiyal agri sendromu ve tedavisi. Romatol Tıb Rehab 8:121–124
Buskila D (1999) Fibromyalgia, chronic fatigue syndrome, and myofascial pain syndrome. Curr Opin Rheumatol 11:119–126
Dohrenwend BP, Raphael KG, Marbach JJ, Gallagher RM (1999) Why is depression comorbid with chronic myofascial face pain? A family study test of alternative hypotheses. Pain 83:183–192
Heikkila H, Heikkila E, Eisemann M (1998) Predictive factors for the outcome of a multidisciplinary pain rehabilitation programme on sick-leave and life satisfaction in patients with whiplash trauma and other myofascial pain: a follow-up study. Clin Rehabil 12:487–496
Han SC, Harrison P (1997) Myofascial pain syndrome and trigger point management. Reg Anesth 22:89–101
Tschopp KP, Gysin C (1996) Local injection therapy in 107 patients with myofascial pain syndrome of the head and neck. ORL J Otorhinolaryngol Relat Spec 58:306–310
Genc H, Erdem R, Karaoglan B, Ertürk C, Yorgancšoglu R (1997) Effectivity of local anesthetic injection and dry needling in myofascial pain syndrome. J Rheum Med Rehab 8:29–33
Wreje U, Brorsson B (1995) A multicenter randomized controlled trial of injections of sterile water and saline for chronic myofascial pain syndromes. Pain 61:441–444
Hong CZ, Hsueh TC (1996) Difference in pain relief after trigger point injections in myofascial pain patients with and without fibromyalgia. Arch Phys Med Rehabil 77:1161–1166
Eden L, Ejlertsson G, Leden I, Nordbeck B (2000) High rates of psychosomatic and neurotic symptoms among disability pensioners with musculoskeletal disorders. J Musculoskelet Pain 8:75–88
Faucette MT, Gil K, Williams DA, Keefe FJ, Goli V (1993) Predictors of response to pain management treatment. Clin J Pain 9:115–123
Katz WA (1998) The needs of a patient in pain. Am J Med 105:2S–7S
Keefe FJ, Dolan E (1986) Pain behavior and pain coping strategies in low back pain and myofascial pain dysfunction syndrome patients. Pain 24:49–56
Lewit K, Simons DG (1984) Myofascial pain: relief by post-isometric relaxation. Arch Phys Med Rehabil 65:452–456
Hanten WP, Olson SL, Butts NL, Nowicki AL (2000) Effectiveness of a home program of ischemic pressure followed by sustained stretching for treatment of myofascial trigger points. Phys Ther 80:997–1003
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kamanli, A., Kaya, A., Ardicoglu, O. et al. Comparison of lidocaine injection, botulinum toxin injection, and dry needling to trigger points in myofascial pain syndrome. Rheumatol Int 25, 604–611 (2005). https://doi.org/10.1007/s00296-004-0485-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-004-0485-6