Abstract
Heart rate variability (HRV) is a useful tool for the detection of sympathetic-parasympathetic balance in the autonomic nervous system. Autonomic nervous system involvement in patients with rheumatoid arthritis (RA) has rarely been studied and has shown conflicting results. Our purpose was to determine if HRV showed changes in patients with RA in comparison with the normal population. Short-term analysis of HRV was performed for time-domain frequency in 42 patients with RA and 44 matched controls. In this analysis, patients displayed lower standard deviation of the mean than healthy subjects (P<0.0001). Patients tended to display higher pNN50 and root-mean-square of successive difference values than did healthy subjects, but these differences were not statistically significant (P>0.05). In frequency domain analysis, the spectral measures of HRV showed reduced high-frequency (HF) values and an higher low-frequency (LF) values; as a result, the ratio between low and high frequencies (LF/HF), representative of sympathovagal modulation, was significantly increased (P=0.001, P=0.012, and P=0.003, respectively). Our data suggest an increase in sympathetic control of the heart rate in patients with RA. This increased sympathetic activity could play a key role in the development of ventricular tachyarrhythmias in RA and may be related to the higher incidence of sudden death in this disorder.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As a connective tissue disease, rheumatoid arthritis (RA) may affect various organs. In it, a greater number of changes in the cardiac system have been noted after death. Several large epidemiological studies found more excess cardiovascular mortality in RA patients than in controls [1, 2, 3, 4]. Myocardial infarction and sudden death were the main sources of excess mortality [5, 6].
Normal heart rate variation depends on the balance between sympathetic and parasympathetic systems. A high variability in heart rate is a sign of good adaptability, implying a healthy individual with well-functioning autonomic control mechanisms. Conversely, lower variability is often an indicator of abnormal and insufficient adaptability of the autonomic nervous system. Reduced HRV has emerged as a strong indicator of risk for adverse events in patients with a wide range of diseases [7, 8, 9.] Compared to traditional tests, HRV analysis is a practical, reproducible, and noninvasive method of detecting early autonomic impairment, allowing better quantitative and qualitative evaluation of sympathovagal modulation of cardiovascular function [10, 11].
Rheumatoid arthritis may produce an imbalance in the autonomic nervous system, but the relationship has rarely been studied and has shown conflicting results [12, 13]. Increased heart rate and decreased HRV might be associated with increased mortality in patients with RA. The aim of this study was to assess the presence and severity of autonomic impairment by evaluating HRV in a series of randomly selected patients with RA.
Materials and methods
Patients
The study group was composed of 48 patients with RA (35 female and 13 male, mean age 47±11.2 years) and 50 healthy subjects (33 female and 17 male, mean age 45±9.4 years). The patients were enrolled in the study between January 1999 and June 2002. In all cases, routine physical examination, 12-lead electrocardiography, telecardiography, routine biochemistry, transthoracic echocardiography, and exercise stress tests were performed. According to the test results, none of the cases had evidence of cardiovascular disease. All RA patients were treated according to the diagnosis based on the Association of Rheumatoid Arthritis criteria, and all were in stages I–IV of the disease according to Steinbrocker's criteria [14]. Patients were tested for autoantibodies, including antinuclear and anti-DNA antibodies, using enzyme-linked immunosorbent assay. Rheumatoid factor was detected in serum samples using the RA latex test. The control group was randomly selected among the patients admitted to the cardiology department with atypical chest pain and normal exercise stress tests.
No patients had clinical signs of autonomic dysfunction, history of myocardial infarction, arterial hypertension, diabetes mellitus including type I and II, or pulmonary disease. Four patients with RA were excluded from the analyses due to the usage of beta-blocker therapy. None of the subjects in either group were taking any drug that could affect the autonomic nervous system. Also, due to smoking habits, two patients and six control subjects were excluded from the study. Therefore, the final group consisted of 42 patients with RA (31 female and 11 male, mean age 48±10.4 years) and 44 healthy controls (31 female and 13 male, mean age 45±8.4 years). All subjects agreed to participate in the research, and the consent of an ethics committee was obtained.
Heart rate variability measurement
A standard ambulatory Holter recording system (Biomedical System Century 2000/3000 Holter monitoring system, version 1.32) was used. A three-channel apparatus recorded the electrocardiographic traces. All recordings were analysed using a Century 2000/3000 HRV Package System (Biomedical Systems, St. Louis, Mo., USA) after adjustment of R-R intervals manually. All recordings were obtained for just an hour between 9:30 AM and 12:30 AM; patients had fasted overnight and remained in recumbent position throughout the recordings. The subjects were asked to remain awake and relaxed, but the depth and rate of breathing were not controlled. Only cycles in which beats had normal morphological characteristics were used for analysis. Intervals between ectopic beats, between normal and ectopic beats, and intervals inaccurately measured because of artefacts were excluded from analysis. Heart rate variability was assessed in two ways: time domain analysis and frequency domain analysis. The mean heart rate, standard deviation of all R-R intervals (SDNN), root-mean square of successive differences (RMSSD), and number of R-R intervals differing by >50 ms from adjacent intervals divided by the total number of all R-R intervals (pNN50) were measured in the time domain analysis. Spectral measures were obtained by the fast-Fourier transform method. According to the Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology [15], recordings were taken as the means of five different 5-min periods. The power in the heart rate spectrum between 0.003 MHz and 0.40 Hz was defined as total energy (ms2). This power was divided into two components: low frequency (LF) (0.04–0.15 Hz) and high frequency (HF) (0.16–0.4 Hz). It is believed that HF is a marker of parasympathetic activity and LF is a marker of sympathetic activity [15]. We also measured the ratio of low-to-high frequency power (LF/HF), reflecting the sympathovagal balance [16]. High values of this ratio indicated dominant sympathetic activity. As in previous reports, many time and frequency domain variables strongly correlated with each other [17]. The SDNN correlated with total power and RMSSD and pNN50 with HF power.
Statistical method
Data were expressed as proportions or mean±SD. Student's t-test was used for evaluation of continuous variables in the two groups and Fisher's exact test for proportions when appropriate. Chi-squared analysis and Student's unpaired t-test were used to compare variables between groups for univariate analysis. The Kruskal-Wallis H test was used to compare variables between stages of the RA group, and Pearson's correlation analysis was performed to see the relation between HRV parameters and stages of RA according to Steinbrocker's criteria. P values of <0.05 were considered statistically significant.
Results
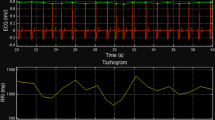
The demographic and clinical data of the 42 study patients with RA are summarized in Table 1. There were no significant differences between RA and controls in these parameters, including coronary risk factors. The results of HRV analysis in patients with RA and controls are shown in Table 2. Figure 1 shows frequency domain analysis in RA and controls. Patients tended to display higher heart rates and greater pNN50 and RMSSD than did healthy subjects, but these differences were not statistically significant (Table 2). The SDNN values, which correlate with total power, were lower in patients with RA (P<0.0001). In frequency domain analysis in the RA group, HF power, which reflects parasympathetic activity, was found to decrease (P=0.012) and LF power, a marker of sympathetic activity, was found to increase (P=0.001) (Table 2). As a result, the LF/HF ratio, a representative of sympathovagal modulation, was significantly higher (P=0.003). There was no significant difference between HRV parameters and stages of RA. Also, no correlation was found between HRV parameters and disease duration, Steinbrocker's classification, or erythrocyte sedimentation rate (ESR) (Table 3, Table 4).
Discussion
The analysis of HRV is considered a valid method to assess autonomic nervous system fluctuations in normal healthy individuals and patients with various cardiovascular and noncardiovascular disorders [11]. There are two approaches to measuring HRV: time domain and frequency domain analyses. In the former, the standard deviation of the mean of R-R intervals (SDNN) represents a general measurement of autonomic nervous system balance, whereas the percentage of R-R intervals differing from each other by more than 50 ms, or pNN50, predominantly reflects parasympathetic activity. In the frequency domain, spectral analysis of R-R intervals can detect two major components: the so-called high-frequency component (HF) of physiologic HRV (spectral components in the band from 0.16 Hz to 0.5 Hz), and the low frequency (LF) component (spectral band from 0.04 Hz to 0.15 Hz). The former is modulated predominantly by the parasympathetic nervous system, whereas the latter is under the influence of both the parasympathetic and sympathetic systems. The LF/HF ratio can be considered a marker of sympathovagal balance [11, 15].
Abnormal autonomic function is known to predispose to arrhythmogenesis in clinical and experimental conditions. The loss of HRV and sympathovagal imbalance (either increased sympathetic or reduced vagal activity) has been shown to be a strong and independent predictor of postinfarction mortality and is of prognostic value in patients with heart failure and diabetic neuropathy [18, 19, 20, 21]. Conversely, vagal predominance could exert protective and antifibrillatory effects [18].
In autoimmune diseases such as systemic lupus erythematosus (SLE) and systemic sclerosis, several studies have shown a significant reduction in HRV [22, 23]. In particular, spectral analysis in SLE has revealed a reduction in high-frequency components, indicating reduced parasympathetic cardiovascular tone. Although peripheral and central nervous system involvement has been well recognized in patients with RA, autonomic nervous system involvement has rarely been studied and has shown conflicting results. Louthrenoo et al. reported diminished heart rate response in patients with RA using standard cardiovascular reflex tests [12]. They also found that diminished heart rate response showed no correlation with disease duration, number of swollen joints, ESR, or rheumatoid factor in the RA group. This result was similar to ours. Maule et al. also showed impaired autonomic nervous function in patients with RA. They reported as well that autoantibodies directed against autonomic nervous system structures might play a role in the pathogenesis of the autonomic dysfunction [13].
In our study, results conflicted between time and frequency domain parameters in the patients and control subjects. They showed a slight increase in pNN50 and RMSSD but a significant reduction in SDNN in time domain parameters in the group with RA (P=0.34, P=0.48, and P<0.0001, respectively). However, we found a significant decrease in HF and increase in LF and LF/HF ratio in patients with RA, suggesting predominance of the sympathetic modulation of the heart. Frequency domain techniques facilitate more precise evaluation of the direction and magnitude of changes in sympathovagal balance than is possible with time domain analysis. Also, frequency domain analysis obtained from short recordings (particularly when conditions are standardized by using the modified orthostatic protocol) are more useful for predicting mortality [24, 25]. Therefore, time domain analysis is a more useful detection method in sustained recording periods. In our study, frequency domain parameters were more reliable for short recording times, so conflicting results between time and frequency domain parameters can be considered less important.
The relative predominance in sympathetic tone plays a key role in the development of ventricular tachyarrhythmia. Indeed, in a recent long-term follow-up study on the cause of death in patients with RA, more sudden deaths were found than in controls. Riise et al. reported that sudden deaths accounted for 11.3% of total mortality in patients with RA [6].
To conclude, in our patients with RA, there are indications of increased sympathetic control of heart rate, as has been observed in other autoimmune diseases. This observation might be of some importance with reference to increased rate of sudden death in RA due to the risk of fatal arrhythmia. However, considering the small number of cases enrolled in this study, further work is necessary to confirm our data.
References
Kvalvik AG, Jones MA, Symmons DPM (2000) Mortality in a cohort of Norwegian patients with rheumatoid arthritis followed from to 1992. Scand J Rheumatol 29:29–37
Monson RR, Hall AP (1976) Mortality among arthritics. J Chron Dis 29:459–467
Mutru O, Laakso M, Isomaki H, Koota K (1985) Ten year mortality and causes of death in patients with rheumatoid arthritis. BMJ 290:1797–1799
Prior P, Symmons DPM, Scott DL et al (1984) Cause of death in rheumatoid arthritis. Br J Rheumatol 23:92–99
Del Rincon I, Williams K, Stern MP et al (2000) High incidence of cardiovascular events in a rheumatoid arthritis cohort not explained by traditional cardiac risk factors abstract. Arthritis Rheum 43 [Suppl]:385
Riise T, Jacopsen BK, Gran JT et al (2001) Total mortality is increased in rheumatoid arthritis. A 17-year prospective study. Clin Rheumatol 20:123–127
Ewing DJ, Campbell IW, Clarke BF (1980) The natural history of diabetic autonomic neuropathy. Q J Med 193:95–108
Multicentre post infarction research group, Kleiger RE, Miller JP et al (1987) Decreased heart rate variability and its association with increased mortality after acute myocardial infarction. Am J Cardiol 59:256–262
Malliani A, Lombardi F, Pagani F et al (1994) Power spectral analysis of cardiovascular variability in patients at risk for sudden cardiac death. J Cardiovasc Electrophysiol 5:274–86
Malpas SC, Gordon LP (1990) Circadian variation of heart rate variability. Cardiovasc Res 24:210–213
Stein PK, Bosner MS, Kleiger RF et al (1994) Heart rate variability: a measure of cardiac autonomic tone. Am Heart J 127:420–424
Louthrenoo W, Ruttanaumpawan P, Aramrattana A et al (1999) Cardiovascular autonomic nervous system dysfunction in patients with rheumatoid arthritis and systemic lupus erythematosus. QJM 92:97–102
Maule S, Quadri R, Mirante D et al (1997) Autonomic nervous dysfunction in systemic lupus erythematosus and rheumatoid arthritis: possible pathogenic role of autoantibodies to autonomic nervous structures. Clin Exp Immunol 110:423–427
Arnett FC (1989) Revised criteria for the classification of rheumatoid arthritis. Bull Rheum Dis 38:1–6
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology (1996) Heart rate variability, standards of measurement, physiological interpretation, and clinical use. Circulation 93:1043–1065
Pagani M, Lombardi F, Guzzetti S et al (1986) Power spectral analysis of heart rate and arterial pressure variability as a marker of sympato-vagal interaction in man and conscious dog. Circ Res 59:178–193
Bigger JT, Fleiss JL, Steinman RC et al (1992) Correlations among time and frequency domain measures of heart period variability two weeks after acute myocardial infarction. Am J Cardiol 69:891–898
Pumprla J, Howarka K, Groves D et al (2002) Functional assessment of heart rate variability: physiological basis and practical applications. Int J Cardiol 84:1–14
Kao T, Hsiao HC, Chiu HW et al (2000) The relationship of late potentials to assessment of heart rate variability in post-infarction patients. Int J Cardiol 74:207–214
Nolan J, Batin PD, Andrews R, Lindsay SJ et al (1998) Prospective study of heart rate variability and mortality in chronic heart failure: results of the United Kingdom Heart Failure Evaluation and Assessment of Risk Trial (UK-HEART). Circulation 98:1510–1516
O'Brien IA, McFadden JP, Corrall RJM (1991) The influence of autonomic neuropathy on mortality in insulin-dependent diabetes. Q J Med 79:495–502
Ferri C, Emdin M, Giuggioli D et al (1997) Autonomic dysfunction in systemic sclerosis: time and frequency domain 24 hour heart rate variability analysis. Br J Rheumatol 36:669–676
Laversuch CJ, Hiromi S, Modarres H et al (1997) Reduction of heart rate variability in patients with systemic lupus erythematosus. J Rheumatol 24:1540–1544
Fei L, Copie X, Malik M et al (1996) Short- and long-term assessment of heart rate variability for risk stratification after acute myocardial infarction. Am J Cardiol 77:681–684
Howarka K, Pumprla J, Schabmann A (1998) Optimal parameters of short-term heart rate spectrogram for routine evaluation of diabetic cardiovascular autonomic neuropathy. J Auton Nerv Syst 69:164–172
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no proprietary interest in the products mentioned in the manuscript, and this study was neither supported nor sponsored by commercial interests.
Rights and permissions
About this article
Cite this article
Evrengül, H., Dursunoglu, D., Cobankara, V. et al. Heart rate variability in patients with rheumatoid arthritis. Rheumatol Int 24, 198–202 (2004). https://doi.org/10.1007/s00296-003-0357-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-003-0357-5