Abstract
Postural changes are sometimes a risk factor for low back pain. Abnormal posture creates a strain on ligaments and muscles that indirectly affects the curvature of the lumbar spine. This study was planned to investigate the relationship between the angles of the lower lumbar spine and spinal mobility in acute and chronic low back pain patients. Fifty patients (25 female, 25 male) with chronic low back pain and fifty (30 female, 20 male) with acute low back pain were included the study. Both groups were subjected to lumbosacral radiography in the lateral position while standing. Patients were assessed by parameters including spinal mobility, sacral inclination angle, lumbosacral angle, and sacral horizontal angle. Spinal mobility included the maximal range of motion of lumbar flexion and extension. The value of the sacral inclination angle was significantly higher and correlated with lumbar extension in chronic low back pain patients ( P <0.005, r =0.32). There was no statistical difference or correlation in lumbosacral and sacral horizontal angles and spinal mobility between the two groups ( P >0.05). Chronic low back pain affects the lower lumbar spine and limits the maximal range of ̇lumbar extension.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Low back pain (LBP) is a major health problem affecting the adult population. Postural changes are one of the risk factors. Abnormal posture makes a strain on ligaments and muscles that indirectly affects the curvature of the lumbar spine. It is known that several complex factors affect the lumbar curve, which has a role in balancing compressive forces. Various studies have examined the relationship between changes in the angle of the lumbar spine and back pain [1, 2].
The degree of spinal mobility indicates the extent of the limitation in LBP patients. The role of postural differences and spinal mobility in LBP disability are uncertain. Any knowledge of the associations between spinal morphology and mobility in LBP will help in preventing disability and in determining diagnosis and the therapy program. Most investigators examined the relationship between pelvic inclination and lumbar lordosis in healthy or chronic LBP (CLBP) patients [3, 4]. A few authors examined the association of the lumbar spine angles in acute LBP (ALBP) patients [5].
The purpose of this study was to investigate the relationships between angles of the lumbar spine and spinal mobility in both acute and chronic LBP patients.
Materials and methods
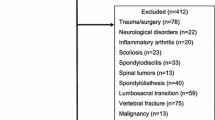
Fifty patients (25 female, 25 male) with CLBP and fifty patients (30 female, 20 male) with ALBP were included in the study. The CLBP patients were expected to have had back pain for at least 3 months. Those with previous spine surgery, inflammatory or tumoral diseases, or spinal deformity including scoliosis were excluded. Before a detailed clinical and radiographic examination, all participants gave written informed consent. After physical examination, both groups were subjected to lumbosacral radiography in the lateral position while standing. Measurements were made directly from the radiographs. Patients were assessed by parameters such as spinal mobility, sacral inclination angle (SIA), lumbosacral angle (LSA), and sacral horizontal angle (SHA). Spinal mobility was defined as the maximal range of lumbar flexion and extension. It was measured by double inclinometer while the patients were standing and bending forward and upward. Sacral inclination angle was measured between the vertical line and a line drawn tangential to the posterior border of the S1 vertebra. The LSA was subtended by lines drawn across the upper border of the sacrum and the lower border of the L5 vertebra. The SHA was measured between a horizontal line and a line drawn tangentially to the upper border of the sacrum. Measurement of the angles is shown in Fig. 1.
The means and standard deviations of all angles and the ranges of lumbar flexion and extension were calculated. Statistical differences between the angles of both groups were calculated by Mann-Whitney U test. Correlation of spinal mobility with the angles of lumbar spine was assessed by Spearman's correlation analysis in SPSS for Windows, version 6.0.
Results
The mean age of the CLBP patients (30 female, 20 male) was 40.3±8.2 years, and that of the ALBP patients (25 female, 25 male) was 42.7±7.9 years. No significant differences in age, gender, and lumbar spine angles were observed between these groups ( P >0.05).
Sacral inclination angle
The SIA value was significantly higher and correlated with maximal range of lumbar extension in CLBP patients ( P <0.005, r =0.32). We also observed that these angles were generally greater in females than in males.
Lumbosacral angle
There was no statistical difference in LSA between acute and chronic LBP patients ( P >0.05). However, females had greater LSA in both groups. No relationship between LSA and the range of motion of lumbar extension and flexion was found in both groups ( P >0.05).
Sacral horizontal angle
Sacral horizontal angle was not age- or gender-related. There was no observable difference between the two groups and no correlation with lumbar flexion and extension for men or women.
The results of the lower lumbar spine angles in acute and chronic LBP patients are shown in Table 1. Correlations of lumbar lordosis angles with the maximal ranges of lumbar flexion and extension for both groups are shown in Table 2.
Discussion
Different authors measured the lumbar spine angles with various methods. The changes in LSA and SIA and the curvature of the lumbar spine during aging were reported before. There is great agreement that females have greater angles than males [6, 7, 8].
Kendall et al. determined that, because of the muscle balance between the back/hip muscles and abdominal muscles in standing position, lumbar lordosis should be associated with pelvic inclination [9].In contrast, Walker et al. found a weak relationship between lumbar lordosis and pelvic inclination in standing position in asymptomatic patients [10]. Youdas et al. observed that gender correlated highly with pelvic inclination and lumbar lordosis but found no correlation of lumbar lordosis with abdominal muscle performance in either males or females [11]. They examined CLBP patients and reported an association between lumbar extension and lumbar lordosis in males [12].
In our study, correlations were found between SIA and lumbar extension in both males and females. However, an increase in LSA was expected in CLBP patients, but we could find no difference in LSA for both groups.
Hansson et al. evaluated the relationships between the extent of lumbar lordosis in asymptomatic, acute, and chronic LBP patients. No difference was observed between the groups, except in gender [5]. Some other investigators also could find no differences in lumbar lordosis and pelvic inclination between asymptomatics and CLBP patients [13, 14]. Some researchers compared lordotic measurements of normal, chronic, and ALBP patients and reported that patients with CLBP had hypolordosis, whereas the acute back pain group was hyperlordotic, with the largest L1–5 angle, Cobb angle, Ferguson's angle, and pelvic tilt angle [15]. Jackson et al. reported that lumbar lordosis was significantly lower and not age- or gender-related in chronic back pain patients [3]. The lumbar lordosis angles were related to each other.
As lumbar lordosis increases, sacral inclination and lumbosacral and sacral horizontal angles also increase. However, studies that examined the relationships between lumbar lordosis angles in chronic back pain patients showed different results on this process. Korovessis et al. found that sacral inclination correlated with thoracic kyphosis and lumbar lordosis and that it also decreased as lumbar lordosis decreased [16]. He also reported that L5–S1 segmental lordosis was greater in chronic back pain patients [17]. We only found that the SIA was larger in CLBP patients and that there was a relationship between this angle and maximal range of lumbar extension for both males and females.
Various studies examined the changes in range of motion of lumbar flexion and extension in chronic back pain patients. Some authors reported no difference from controls in the range of lumbar flexion in CLBP patients . Some investigators noted decreased lumbar extension range in male CLBP patients [12, 14]. We found this decrease in both males and females.
Changing lumbar lordosis seems to depend on the abdominal muscles, back muscles, and pelvic/back ligament function and tonus. Acute LBP is a temporary, painful disorder that limits patients' activities but mostly plays a role in the disease chronicity. Changes in lumbar lordosis angles may affect the diagnosis and treatment in LBP patients and also affect the planning of a proper exercise program for the back or abdominal muscles.
In this study, abdominal muscle force and function were not examined. We only conclude that the SIA is greater in CLBP patients. This angle is mostly related with spondylolisthesis and isthmic pathologies. It also increases and thus correlates with the maximal range of lumbar extension. Probably there will be isthmic pathologies or silent spondylolisthesis in the L5–S1 region that we cannot determine in lateral radiographs. Also, chronic back pain makes a chronic muscle strain that may result in a vertical position of the sacrum. This may cause additional facet joint problems, spinal stenosis, and limitation in lumbar extension. These conditions should be taken into consideration while preparing a proper exercise program.
Additional research should be helpful in confirming the relationships between lumbar spine angles and LBP.
References
Lin RM, Jou IM, Yu CY (1992) Lumbar lordosis: normal adults. J Formos Med Assoc 9:329–333
Keegan JJ (1953) Alterations of the lumbar curve related to posture and seating. J Bone Joint Surg Am 35:589–603
Jackson RP, McManus AC (1994) Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex and size. A prospective controlled clinical study. Spine 19:1611–1618
During J, Goudfrooij H, Keessen W, Beeker TW, Crowe A (1985) Toward standards for posture. Postural characteristics of the lower back system in normal and pathologic conditions. Spine 10:83–87
Hansson T, Bigos S, Beecher P, Wortley M (1985) The lumbar lordosis in acute and chronic low-back pain. Spine 10:154–155
Fernand R, Fox DE (1985) Evaluation of lumbar lordosis: a prospective and retrospective study. Spine 10:799–803
Amonoo-Kuofi HS (1992) Changes in the lumbosacral angle, sacral inclination and the curvature of the lumbar spine during aging. Acta Anat 145:373–377
Ericksen MF (1978) Aging in the lumbar spine. Am J Phys Anthropol 48:241–246
Kendall FP, McCreary EK, Provance PG (1993) Muscles: testing and function. Fourth edn. Williams and Wilkins, Baltimore
Walker ML, Rothstein JM, Finucane SD, Lamb RL (1987) Relationships between lumbar lordosis, pelvic tilt and abdominal muscle performance. Phys Ther 67:512–516
Youdas JW, Garrett TR, Harmsen S, Suman VJ, Carey JR (1996) Lumbar lordosis and pelvic inclination of asymptomatic adults. Phys Ther 76:1066–1081
Youdas JW, Garrett TR, Egan KS, Therneau TM (2000) Lumbar lordosis and pelvic inclination in adults with chronic low back pain. Phys Ther 80:261–275
Day JW, Smidt GL, Lehmann T (1984) Effect of pelvic tilt on standing posture. Phys Ther 64:510–516
Pope MH, Bevins T, Wilder DG, Frymoyer JW (1985) The relationship between anthropometric, postural, muscular and mobility characteristics of males ages 18–55. Spine 10:644–648
Harrison DD, Calliet R, Janik TJ, Troyanovich SJ, Harrison DE, Holland B (1998) Elliptical modeling of the sagittal lumbar lordosis and segmental rotation angles as a method to discriminate between normal and low back pain subjects. J Spinal Disord 11:430–439
Korovessis P, Stamatakis M, Baikousis A (1998) Reciprocal angulation of vertebral bodies in the sagittal plane in an asymptomatic Greek population. Spine 23:700–705
Korovessis P, Stamatakis M, Baikousis A (1999) Segmental roentgenographic analysis of vertebral inclination on sagittal plane in asymptomatic versus chronic low back pain patients. J Spinal Disord 12:131–137
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was presented at the European Congress of Rheumatology "EULAR 2001," Prague, 13–16 June 2002
Rights and permissions
About this article
Cite this article
Evcik, D., Yücel, A. Lumbar lordosis in acute and chronic low back pain patients. Rheumatol Int 23, 163–165 (2003). https://doi.org/10.1007/s00296-002-0268-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-002-0268-x