Abstract
Exposure of bacteria to a sub-lethal dosage of antibiotic is one the major causes for the onset of antibiotic resistance. Therefore, we aimed to assess the emergence of antibiotic cross-resistance in bacteria after exposure to a sub-lethal dose of veterinary feed directive (VFD) antibiotics, tilmicosin, and florfenicol. The minimum inhibitory concentrations (MICs) of tilmicosin and florfenicol against Salmonella enterica serovar Enteritidis, Klebsiella pneumoniae, Staphylococcus aureus, and Listeria monocytogenes were determined. Next, the pathogens were exposed to a sub-inhibitory concentration of tilmicosin (0.5, 5, 20 µg/ml) and florfenicol (1, 20 µg/ml) for 24 h and 48 h, and acquired cross-resistance to human therapeutic antibiotics was measured by determining the increase in MIC values. MICs of ampicillin, tetracycline, nalidixic acid, and meropenem against Salmonella and Klebsiella were in the range of 20–1000 µg/ml, 5–62.5 µg/ml, 5–125 µg/ml, and 0.05–0.1 µg/ml, respectively, whereas MICs against Staphylococcus and Listeria were 2.5–10 µg/ml, 2.5 µg/ml, 62.5–500 µg/ml, and 0.1–0.2 µg/ml, respectively. Pre-exposure of these bacteria to a sub-inhibitory concentration of tilmicosin and florfenicol, increased cross-resistance against ampicillin, tetracycline, and nalidixic acid from 1.25- to 40-fold compared to the antibiotic unexposed bacteria with the exception of meropenem, which did not show increased resistance. This study could serve as a foundation to understand the mechanisms of acquired cross-resistance to traditional therapeutic antibiotics, and to develop strategies to alleviate such problem by using alternative antimicrobials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extensive and indiscriminate use of antibiotics in the community, hospitals, and clinics have fueled the crisis of antibiotic resistance [1,2,3,4]. Globally, antibiotic resistance is projected to cause 700,000 deaths each year by 2050 at a cost to world GDP of US$100 trillion [5]. Around 80% of all antibiotics sold in the United States are administered to food animals, primarily as a growth supplement and (or) for controlling infection [6]. Widespread application of antibiotics as a therapeutic agent in animals and humans, and as a growth promoter in livestock exposes bacteria to the sub-inhibitory (non-lethal) dose of antibiotics. This has played a critical role in the evolution of antibiotic resistance [7, 8], selection for antibiotic-resistant bacteria [9], and the emergence of multidrug-resistant (MDR) bacterial pathogens, such as extended spectrum β-lactamase (ESBL) Gram-negative bacteria [10, 11].
In food animals, antibiotics are used widely as growth promoting agents and therapeutics. Due to increased concern about antibiotic resistance in microorganisms, antibiotics that are used for the treatment of human infectious diseases are forbidden in food animals as growth promoting agents [12, 13]. Therefore, the US Food and Drug Administration (FDA) has approved veterinary antibiotics, referred to as VFD drugs; tilmicosin, florfenicol, and avilamycin for exclusive therapy in food animals [14] with the premise that these antibiotics are safe and may not contribute to the emergence of antibiotic resistance in human foodborne pathogens.
Tilmicosin is a macrolide antibiotic that inhibits bacterial protein synthesis, specifically peptidyl transferase activity [15]. It is generally active against Gram-positive bacteria and possesses limited activity against Gram-negative bacteria. It is approved for the treatment of bacterial infection in swine and cattle, and the duration of use is 21 and 14 days, respectively. Florfenicol is a broad-spectrum bacteriostatic antibiotic that inhibits protein synthesis by binding to ribosomal subunits, leading to the inhibition of peptidyl transferase [16]. It has been approved for the treatment of bacterial infection in swine and fish and the recommended length of use is 5 and 10 days, respectively. Both florfenicol and tilmicosin are primarily used to treat respiratory tract infections in cattle [14].
Exposure of bacteria to the sub-inhibitory dose of antibiotics in the environment can lead to the development of antibiotic resistance. Sub-inhibitory concentrations of antibiotics can reach environment either through pharmaceutical industry waste, veterinary feed or animal, and human fecal waste, and considered a major selection pressure for the development of antibiotic resistance [17]. There is a huge knowledge gap in our understanding of the amount or class of antibiotics that are responsible for the onset of cross-resistance and acquired resistance in bacteria. Therefore, our goal was to investigate whether veterinary-use antibiotics have the potential to contribute to the emergence of acquired resistance in foodborne or enteric pathogens such as Salmonella enterica, Klebsiella pneumoniae, Staphylococcus aureus, and Listeria monocytogenes to the commonly used human therapeutic antibiotics.
Materials and Methods
Antibiotics
Ampicillin, nalidixic acid, and tetracycline (Sigma Aldrich) were dissolved in water to prepare stock solutions of 100 mg/ml, 50 mg/ml, and 100 mg/ml, respectively. Meropenem (Carbapenem) (Tokyo Chemical Industry) was resuspended in dimethyl sulfoxide (DMSO, Sigma Aldrich) to prepare a stock solution of 10 mg/ml. Tilmicosin and florfenicol (Sigma Aldrich) were dissolved in a mixed solvent of acetone and water (1:1) to prepare a stock concentration of 30 mg/ml. All antibiotics were freshly prepared and used within 30 days. Antibiotic stock solutions were stored at 4 °C except tetracycline stored at room temperature.
Bacterial Strains and Culture Conditions
Gram-negative bacteria, Salmonella enterica serovar Enteritidis PT21(Salmonella Enteritidis), Klebsiella pneumoniae ATCC 33495, and Gram-positive bacteria, Staphylococcus aureus ATCC 25923, and Listeria monocytogenes F4244 strains were used in this study. Bacterial stock solutions (20% glycerol) were directly streaked on tryptic soy agar-yeast extract (0.6%) (TSAYE) to obtain single pure colonies, which were aseptically inoculated into Mueller–Hinton broth (MHB) to raise cultures for MIC estimation.
Minimum Inhibitory Concentration of Animal and Human Antibiotic
The MIC of ampicillin, tetracycline, nalidixic acid, tilmicosin, florfenicol, and meropenem for S. Enteritidis, K. pneumoniae, S. aureus, and L. monocytogenes was determined in MHB using broth dilution assay in microtiter plates after taking spectrophotometric absorbance measurements at 600 nm [18, 19] in a microtiter plate reader (BioTek, Teknova, Hollister, CA). All antibiotics were double diluted in 96-well microtiter plate in 100 µl MHB as diluent. For MIC estimation, antibiotic final concentrations in the microtiter plates were as follows: ampicillin, nalidixic acid and tetracycline, 0–1000 µg/ml; tilmicosin, 0–500 µg/ml; florfenicol, 0–40 µg/ml; and meropenem, 0–0.4 µg/ml. The test bacteria were Salmonella Enteritidis, K. pneumoniae, S. aureus, and L. monocytogenes. Initial concentration of test bacteria was calculated by plating tenfold serial dilution of 20 h grown cultures on TSAYE. An aliquot of 100 µl inoculum of about 5 × 107 CFU/ml of each strain suspended in MHB was added in each well of microtiter plate except the negative controls and incubated at 37 °C in a shaking incubator (70 rpm) for 24 h.
After estimating MIC values for each VFD, we determined the sub-inhibitory dose (0.04 − 0.5 × MIC) for each pathogen. Salmonella Enteritidis and K. pneumoniae were pre-exposed to sub-inhibitory concentrations of tilmicosin at 20 µg/ml each, while S. aureus and L. monocytogenes were exposed to tilmicosin at 0.5 µg/ml and 5 µg/ml, respectively, and incubated at 37 °C for 24–48 h. Similarly, Salmonella Enteritidis and K. pneumoniae were grown in the presence of sub-inhibitory dose of florfenicol (1 µg/ml and 20 µg/ml), respectively, and both S. aureus and L. monocytogenes in the presence of 1 µg/ml, and bacteria were incubated at 37 °C for 24–48 h. These pre-exposed test bacteria were used as inoculum to determine MIC of each antibiotic (ampicillin, tetracycline, meropenem, and nalidixic acid) by microtiter plate dilution method [18].
Statistical Analysis
The MIC values for each treatment were calculated from the bacterial absorbance (A600nm) values from three independent experiments and each had three replicate wells. GraphPad Prism version 6 was used to analyze data and plot graphs.
Results and Discussion
MIC of Animal and Human Antibiotics Against Pathogens
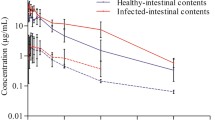
It is essential to estimate the MIC of tilmicosin and florfenicol against test pathogens before assessing the effect of sub-inhibitory dosage on bacterial cross-resistance to other therapeutic human/animal antibiotics. Depending on the pathogen, the MIC of tilmicosin and florfenicol along with human therapeutic antibiotics (ampicillin, tetracycline, nalidixic acid, and meropenem) varied (Table 1; Figs. 1, 2). The MIC of tilmicosin against Salmonella Enteritidis and K. pneumoniae was 125 and 500 µg/ml, respectively, while for L. monocytogenes and S. aureus 62.5 µg/ml and 2.5 µg/ml, respectively (Fig. 1a; Table 1). Salmon et al. [20] reported the MIC90 of tilmicosin against Gram-negative bacteria such as Salmonella Choleraesuis and E. coli to be > 64 µg/ml, which corroborates with our observation. Collectively, these data show Gram-negative bacteria are more resistant to tilmicosin than the Gram-positive bacteria.
Minimum inhibitory concentration (MIC) of veterinary feed directive (VFD) antibiotics, tilmicosin (a) and florfenicol (b) against Salmonella enterica serovar Enteritidis PT21 (SE), Klebsiella pneumoniae ATCC 33495 (Kp), Staphylococcus aureus ATCC 25923 (Sa), and Listeria monocytogenes F4244 (Lm). The absorbance of blank (Mueller–Hinton broth, MHB) was 0.045 ± 0.015 at 600 nm. The broken straight line indicates threshold absorbance value (0.09), and an absorbance > 0.09 indicates growth of cultures in the wells of the microtiter plate (Color figure online)
Minimum inhibitory concentration (MIC) of extended spectrum beta-lactam (ESBL) antibiotic, meropenem against Salmonella enterica serovar Enteritidis PT21 (SE), Klebsiella pneumoniae ATCC 33495 (Kp), Staphylococcus aureus ATCC 25923 (Sa), and Listeria monocytogenes F4244 (Lm). The absorbance of blank (Mueller–Hinton broth, MHB) was 0.045 ± 0.015 at 600 nm. The broken straight line indicates threshold absorbance value (0.09), and an absorbance > 0.09 indicates growth of cultures in the wells of the microtiter plate (Color figure online)
The MIC of florfenicol against Salmonella Enteritidis and L. monocytogenes was 2.5 µg/ml, S. aureus 10 µg/ml and K. pneumoniae 40 µg/ml (Table 1; Fig. 1b). In general, the tested pathogens were more sensitive to florfenicol than tilmicosin. Among the bacterial pathogens, K. pneumoniae exhibited the highest MICs (62.5, 125, 1000 µg/ml) and S. aureus the lowest MICs (2.5, 62.5, 2.5 µg/ml) against tetracycline, nalidixic acid, and ampicillin, respectively (Table 1). Meropenem, a broad-spectrum antibacterial agent of the carbapenem family [21] showed the highest antimicrobial activity against all tested pathogens, where the MIC for Salmonella Enteritidis was 0.05 µg/ml, K. pneumoniae 0.1 µg/ml, S. aureus 0.1 µg/ml, and L. monocytogenes 0.2 µg/ml (Table 1; Fig. 2). This is encouraging since meropenem is used as an antibiotic of last resort in empirical therapy of infection, where the causal bacterial agent is unknown [21].
Based on the MIC values, the sub-inhibitory concentration for tilmicosin was estimated to be 20 µg/ml for Salmonella Enteritidis and K. pneumoniae, 0.5 µg/ml for S. aureus, and 5 µg/ml for L. monocytogenes. The sub-inhibitory concentration for florfenicol was 1 µg/ml for Salmonella Enteritidis, S. aureus, and L. monocytogenes, while 20 µg/ml for K. pneumoniae.
Pre-exposure to Tilmicosin and Florfenicol Increases MIC to Human Therapeutic Antibiotics
Bacterial pathogens were pre-exposed to the sub-inhibitory concentrations of tilmicosin and florfenicol for 24–48 h before testing their sensitivity (MIC) to ampicillin, tetracycline, meropenem, and nalidixic acid. Tilmicosin pre-exposed Salmonella Enteritidis (Fig. 3a), S. aureus (Fig. 3c), and L. monocytogenes (Fig. 3d) exhibited 2.5-, 5-, and 1.25-fold increased cross-resistance (i.e., increased MIC) to ampicillin; and 1.25-, 5-, and 5-fold increased resistance to tetracycline, respectively. Likewise, Salmonella Enteritidis and S. aureus showed 1.25- and 3.2-fold increased resistance to nalidixic acid, respectively, while K. pneumoniae and L. monocytogenes did not show any change in sensitivity to nalidixic acid (Figs. 3b, d). Nalidixic acid, a quinolone antibiotic, targets DNA gyrase or topoisomerase IV and is active against Gram-negative bacteria [22]. Nalidixic acid is a paradoxical antibiotic, which shows higher antibacterial activity at a lower antibiotic concentration (50–200 µg/ml) and lower antibacterial activity at higher concentration (> 200 µg/ml). Antibacterial effect is bacteriostatic at the concentration of 400 µg/ml against Gram-negative bacteria [22].
Development of cross-resistance in bacteria after pre-exposure to the sub-inhibitory concentrations of veterinary feed directive (VFD) antibiotic, tilmicosin in Mueller–Hinton broth (MHB). Effect of sub-inhibitory concentrations of tilmicosin (TIL) pre-exposure to aSalmonella enterica serovar Enteritidis PT21 (SE), bKlebsiella pneumoniae ATCC 33495 (Kp), cStaphylococcus aureus ATCC 25923 (Sa), and dListeria monocytogenes F4244 (Lm) for 24 and 48 h on the cross-resistance against human therapeutic antibiotics, ampicillin, tetracycline, meropenem, and nalidixic acid. TIL0.5, TIL5, and TIL20 represent exposure of bacteria to 0.5 µg/ml, 5 µg/ml, and 20 µg/ml sub-inhibitory concentrations of tilmicosin (Color figure online)
Moreover, our data suggest that K. pneumoniae used in this study were naturally resistant to ampicillin (MIC 1000 µg/ml) and pre-exposure of K. pneumoniae to 20 µg/ml of tilmicosin did not change the MIC against ampicillin (Fig. 3b). None of the pathogens showed any change in sensitivity to meropenem (Fig. 3), and all tested pathogens revealed a MIC value of 0.1 µg/ml regardless of pre-exposure to the sub-inhibitory concentration of tilmicosin. These data clearly suggest an emergence of acquired cross-resistance after pre-exposure of bacteria to the sub-inhibitory concentration of tilmicosin for 24–48 h. In a previous study, Langsrud et al. [23] observed a sixfold to tenfold increase in MIC of benzalkonium chloride and chloramphenicol when E. coli cells were pre-exposed to the sub-inhibitory concentration of benzalkonium chloride.
Florfenicol pre-exposed Salmonella Enteritidis (Fig. 4a), S. aureus (Fig. 4c), and L. monocytogenes (Fig. 4d) exhibited 20-, 5-, and 1.25-fold increased resistance to ampicillin; and 40-, 5-, and 5-fold increased resistance to tetracycline, respectively (Fig. 4). Furthermore, Salmonella Enteritidis, S. aureus, and K. pneumoniae (Fig. 4b) exhibited 40-, 6.4-, and 1.6-fold increased resistance to nalidixic acid, respectively, while L. monocytogenes did not show any sensitivity to nalidixic acid (Fig. 4). Similar to tilmicosin, pre-exposure to florfenicol also did not increase bacterial resistance to meropenem, (Fig. 4). These data clearly show that use of VFD drugs even at the sub-inhibitory concentrations have the potential to develop cross-resistance in pathogens against human use antibiotics. Any residual passage of these antibiotics from veterinary feed or animal to the environment may contribute to the exposure of bacteria to the sub-inhibitory levels of antibiotics and the development of antibiotic resistance. Therefore, this study could serve as a foundation for our understanding of the development of cross-resistance in meat or milk-borne pathogens that were pre-exposed to VFD antibiotics and help develop an eventual strategy to avoid transfer of such traits to pathogens. Application of antibiotics in agriculture is debated as a major cause for the rise of antibiotic-resistant bacterial diseases in human medicine [24]. With limited literature on animal-human antibiotic cross-resistance, this study could serve as a groundwork to gain insight into understanding the development of acquired antibiotic cross-resistance.
Development of cross-resistance in bacteria after pre-exposure to the sub-inhibitory concentrations of veterinary feed directive (VFD) antibiotic, florfenicol in Mueller–Hinton broth (MHB). Effect of sub-inhibitory concentrations of florfenicol (FLN) pre-exposure to aSalmonella enterica serovar Enteritidis PT21 (SE), bKlebsiella pneumoniae ATCC 33495 (Kp), cStaphylococcus aureus ATCC 25923 (Sa), and dListeria monocytogenes F4244 (Lm) for 24 and 48 h on the cross-resistance against human therapeutic antibiotics, ampicillin, tetracycline, meropenem, and nalidixic acid. FLN1 and FLN20 correspond to an exposure of bacteria to 1 µg/ml and 20 µg/ml sub-inhibitory concentrations of florfenicol (Color figure online)
Conclusion
In this study, we observed that pre-exposure of enteric bacterial pathogens to the sub-lethal (sub-inhibitory) concentrations of veterinary feed antibiotics, tilmicosin, and florfenicol substantially increased the antibiotic cross-resistance by 1.25- to 40-fold against human/animal-use antibiotics, ampicillin, tetracycline, and nalidixic acid but not to meropenem. Meropenem showed the highest antimicrobial activity against all four pathogens tested and had the least chance for developing cross-resistance. These results indicate that there is a potential for the emergence of cross-resistance to human use therapeutic antibiotics if pathogens are exposed to a sub-inhibitory dose of animal antibiotics.
References
Neu HC (1992) The crisis in antibiotic resistance. Science 257(5073):1064–1073
Beceiro A, Tomas M, Bou G (2013) Antimicrobial resistance and virulence: a successful or deleterious association in the bacterial world? Clin Microbiol Rev 26(2):185–230
Davies J, Davies D (2010) Origins and evolution of antibiotic resistance. Microbiol Mol Biol Rev 74(3):417–433
Rodriguez-Rojas A, Rodriguez-Beltran J, Couce A, Blazquez J (2013) Antibiotics and antibiotic resistance: a bitter fight against evolution. Int J Med Microbiol 303(6–7):293–297
O’Neill J (2014) Antimicrobial resistance: tackling a crisis for the health and wealth of nations. Rev Antimicrob Resist 20:1–16
Marshall BM, Levy SB (2011) Food animals and antimicrobials: impacts on human health. Clin Microbiol Rev 24(4):718–733
Andersson DI, Hughes D (2014) Microbiological effects of sublethal levels of antibiotics. Nat Rev Microbiol 12(7):465–478
Zhu X, Liu D, Singh AK, Drolia R, Bai X, Tenguria S, Bhunia AK (2018) Tunicamycin mediated inhibition of wall teichoic acid affect Staphylococcus aureus and Listeria monocytogenes cell morphology, biofilm formation and virulence. Front Microbiol 9:1352
Gullberg E, Cao S, Berg OG, Ilback C, Sandegren L, Hughes D, Andersson DI (2011) Selection of resistant bacteria at very low antibiotic concentrations. PLoS Pathog 7(7):e1002158
Carlet J, Jarlier V, Harbarth S, Voss A, Goossens H, Pittet D, Participants of the 3rd World Healthcare-Associated Infections F (2012) Ready for a world without antibiotics? The pensieres antibiotic resistance call to action. Antimicrob Resist Infect Control 1(1):11
Blair JMA, Richmond GE, Piddock LJV (2014) Multidrug efflux pumps in Gram-negative bacteria and their role in antibiotic resistance. Future Microbiol 9(10):1165–1177
Mathew AG, Cissell R, Liamthong S (2007) Antibiotic resistance in bacteria associated with food animals: a United States perspective of livestock production. Foodborne Pathog Dis 4(2):115–133
Cheng G, Hao H, Xie S, Wang X, Dai M, Huang L, Yuan Z-H (2014) Antibiotic alternatives: the substitution of antibiotics in animal husbandry? Front Microbiol 5:217
Allen HK, Stanton TB (2014) Altered egos: antibiotic effects on food animal microbiomes. Annu Rev Microbiol 68:297–315
Debono M, Willard KE, Kirst HA, Wind JA, Crouse GD, Tao EV, Vicenzi JT, Counter FT, Ott JL, Ose EE (1989) Synthesis and antimicrobial evaluation of 20-deoxo-20-(3, 5-dimethylpiperidin-l-yl) desmycosin (tilmicosin, EL-870) and related cyclic amino derivatives. J Antibiot 42(8):1253–1267
Cannon M, Harford S, Davies J (1990) A comparative study on the inhibitory actions of chloramphenicol, thiamphenicol and some fluorinated derivatives. J Antimicrob Chemother 26(3):307–317
Bengtsson-Palme J, Larsson DJ (2016) Concentrations of antibiotics predicted to select for resistant bacteria: proposed limits for environmental regulation. Environ Int 86:140–149
Andrews JM (2001) Determination of minimum inhibitory concentrations. J Antimicrob Chemother 48(Suppl 1):5–16
Singh AK, Drolia R, Bai X, Bhunia AK (2015) Streptomycin induced stress response in Salmonella enterica serovar Typhimurium shows distinct colony scatter signature. PLoS ONE 10(8):e0135035
Salmon SA, Watts JL, Case CA, Hoffman LJ, Wegener HC, Yancey R (1995) Comparison of MICs of ceftiofur and other antimicrobial agents against bacterial pathogens of swine from the United States, Canada, and Denmark. J Clin Microbiol 33(9):2435–2444
Baldwin CM, Lyseng-Williamson KA, Keam SJ (2008) Meropenem: a review ot its use in the treatment of serious bacterial infection. Drugs 68(6):803–838
Crumplin GC, Smith JT (1975) Nalidixic acid: an antibacterial paradox. Antimicrob Agents Chemother 8(3):251–261
Langsrud S, Sundheim G, Holck A (2004) Cross-resistance to antibiotics of Escherichia coli adapted to benzalkonium chloride or exposed to stress-inducers. J Appl Microbiol 96(1):201–208
Chang Q, Wang W, Regev-Yochay G, Lipsitch M, Hanage WP (2015) Antibiotics in agriculture and the risk to human health: how worried should we be? Evol Appl 8(3):240–247
Funding
Funding was provided by Agricultural Research Service (Grant Number 59-8072-6-001).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singh, A.K., Bhunia, A.K. Animal-Use Antibiotics Induce Cross-Resistance in Bacterial Pathogens to Human Therapeutic Antibiotics. Curr Microbiol 76, 1112–1117 (2019). https://doi.org/10.1007/s00284-019-01744-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00284-019-01744-2